PCOD / PCOS
PCOD and PCOS: Differences, Symptoms, and Treatment
Generally, when we talk about PCOD (Polycystic Ovarian Disease) and PCOS (Polycystic Ovary Syndrome), most people—men, women, or anyone—when they hear terms like irregular periods or notice difficulty in weight reduction, immediately consider the possibility of PCOD. People often decide to check for PCOD as soon as such symptoms appear. Regularly, we hear more about PCOD, whereas PCOS is less commonly discussed, even though it is equally important.
From my experience, when speaking with clients, we often ask whether they are suffering from PCOD, but rarely do we inquire about PCOS. This highlights a lack of awareness about PCOS despite its significance.
In clinical and practical contexts, it is essential to understand the differences between PCOD and PCOS. While many symptoms overlap, especially regarding irregular periods and weight issues, the causes, treatment methods, and preventive measures differ significantly.

Approximately 70% of the symptoms are similar between PCOD and PCOS. These include:
- Irregular menstrual cycles
- Difficulty in losing weight
- Hormonal imbalances
- Fatigue or other related discomforts
The main differences lie in:
- Causes: PCOD and PCOS arise due to different underlying physiological and hormonal factors.
- Treatment: While some general approaches may overlap, specific treatments vary. PCOS may require more targeted interventions compared to PCOD.
- Prevention: Preventive strategies differ due to the distinct origins of each condition.
The approach to treatment includes:
- Dietary modifications suited to the individual’s condition
- Lifestyle changes
- Use of Ayurveda and natural herbs to manage hormonal imbalances and improve ovarian health
By analyzing client cases and symptoms, we can see how PCOD and PCOS manifest differently. Understanding these differences is crucial for designing appropriate treatment plans, dietary recommendations, and preventive strategies.
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are two distinct conditions affecting women, particularly during their reproductive years. PCOD is a disease, whereas PCOS is a syndrome. This distinction is important because it highlights that a disease can be caused by a variety of factors, including weight gain, stress, improper lifestyle habits, a sedentary lifestyle, or other medical conditions such as thyroid disorders. These factors contribute to the development of PCOD, which is very common in the population. Studies and observations indicate that approximately one-third of women suffer from PCOD.
PCOD (Polycystic Ovarian Disease) is most frequently seen in women aged 12 to 45 years—essentially from the age they attain maturity. Many girls start showing PCOD symptoms as early as 11 to 12 years old, often due to unhealthy lifestyle practices and poor dietary habits. PCOD is considered a common hormonal disorder, and it is widely observed across different populations.
In contrast, PCOS (Polycystic Ovary Syndrome) was previously considered a rare condition, affecting only about 1% of women around 10 to 15 years ago. However, in recent years, the prevalence of PCOS has increased significantly, and it is now more commonly diagnosed among women of reproductive age.
The primary difference between the two lies in their frequency and underlying mechanisms:
- PCOD is a common hormonal disorder that develops due to a combination of lifestyle factors, stress, weight fluctuations, and minor medical issues.
- PCOS, on the other hand, is a syndrome with more complex hormonal and metabolic disturbances, which makes it more severe and harder to manage in comparison to PCOD.
Understanding the distinction between PCOD and PCOS is essential for accurate diagnosis, proper treatment planning, and effective lifestyle interventions. While PCOD can often be managed with lifestyle changes and dietary adjustments, PCOS may require a more targeted approach due to its more severe and systemic effects.
PCOD in Young Girls: Early Onset, Symptoms, and Complications:
PCOD can start affecting girls at a very young age, even before attaining full maturity. Children between 8 to 10 years old may already begin to show signs of obesity, particularly if they have poor sleep habits, limited physical activity, and a highly sedentary lifestyle dominated by school schedules. Many children spend their entire day studying, with minimal extracurricular activities, and some even study late into the night without proper attention to nutrition. As a result, from ages 8 to 11, obesity is increasingly observed among children.
When these children reach 12 years of age, entering puberty while already obese, they are at a higher risk of developing irregular menstrual cycles within the first 6 to 12 months after maturity. This early onset of PCOD is becoming more visible in young girls aged 12 to 14 years. Along with obesity and irregular periods, affected girls often experience acne and unusual pigmentation on various body areas.
This combination of physical changes and stress can further worsen their condition. Some girls may overeat due to stress, or alternatively, restrict their food intake, leading to a cycle of weight gain, inactivity, and the manifestation of PCOD. Currently, one-third of the female population shows signs of PCOD, and it is now common to see one or two affected children per family. Fortunately, early intervention can help reduce the severity of these symptoms.
Characteristics and Symptoms of PCOD:
PCOD is primarily characterized by hormonal imbalance, which manifests in multiple physical and metabolic symptoms:
- Irregular Periods:
- Young girls may experience periods that are inconsistent, delayed, or sometimes absent.
- Some girls, after initially starting menstruation, may have periods that stop for 2–3 days and only resume with medication, dietary adjustments, and weight reduction.
- Weight Gain and Obesity:
- Obesity is often a visible early sign in young girls before and after puberty.
- Sedentary habits and stress contribute to excessive weight gain.
- Acne:
- Persistent and excessive acne is a common symptom due to hormonal imbalance.
- Hirsutism (Excessive Hair Growth):
- Unusual hair growth can appear on the hands, legs, upper lip, and chin.
- Many children as young as 12 years old seek treatment specifically for hair removal.
- Pigmentation Changes:
- Darkened or unusual pigmentation may develop on certain areas of the body.
Complications of Untreated PCOD:
If timely treatment is not initiated, PCOD can lead to severe health complications even at a young age:
- Insulin-Resistant Diabetes: Hormonal imbalance can disrupt insulin regulation, increasing diabetes risk.
- Obesity: Persistent weight gain exacerbates PCOD symptoms.
- High Cholesterol: Metabolic changes may increase cholesterol levels.
- Heart Diseases: Obesity, high cholesterol, and insulin resistance collectively raise the risk of cardiovascular conditions.
Many cases go untreated due to lack of awareness, misconceptions, or neglect. Parents and children may misinterpret symptoms, thinking they are caused solely by poor diet or sleep, or they may believe issues like low iron or hemoglobin are the primary concern. Such misunderstandings often delay treatment, leading to the development of metabolic complications at a very young age.
Summary of Early-Onset PCOD Symptoms:
- Obesity before and after puberty
- Irregular menstrual cycles within the first 6–12 months of maturity
- Acne and skin changes
- Excessive hair growth on face and body
- Unusual pigmentation
- Stress and eating behavior fluctuations
Recognizing these symptoms early and initiating appropriate dietary, lifestyle, and medical interventions is crucial to prevent long-term complications and manage PCOD effectively in young girls.
Common Symptoms of PCOD and Challenges in Weight Management
People suffering from PCOD often display a range of visible and persistent symptoms, which can affect both young girls and adult women, typically up to ages 45 to 50. One of the most common and noticeable features is acne, which can appear on multiple parts of the body, including the face, neck, and back.
- Facial Acne (Acne Vulgaris):

- Acne often develops on the face due to hormonal imbalance associated with PCOD.
- Poor hair hygiene, irregular washing habits, or scalp conditions like dandruff can worsen acne.
- Back and Neck Acne:
- Accumulation of sweat, infection, and dandruff on the back and neck can contribute to localized acne in these areas.
- Hair Fall and Dandruff:
- Excessive hair loss and dandruff are frequently observed among individuals with PCOD.
- These issues are often linked to hormonal imbalance and poor scalp care.
Weight Gain and Difficulty Losing Weight:
Another significant concern for people with PCOD is weight gain, coupled with difficulty in losing weight despite efforts such as gym workouts, aerobics, physical exercises, and various dietary changes.
- Many patients observe little to no change in weight even after following different routines.
- The key reason often lies in inconsistency:
- Engaging in exercises or following a diet for only a few days without maintaining it regularly leads to minimal results.
- Weight management requires consistent and sustained effort, rather than sporadic or intensive short-term activity.
Guidelines for Consistency:
- Activities should be performed regularly and consistently, even if it is a short duration, such as 15 minutes of exercise daily.
- Overexertion on a single day (for example, 1 hour) followed by reduced activity in subsequent days (15–30 minutes) does not produce effective results.
- A structured and steady approach to diet and physical activity is crucial for controlling weight and managing PCOD symptoms.
By focusing on consistent lifestyle practices, patients with PCOD can better manage their weight, acne, hair problems, and overall hormonal imbalance. Irregular or inconsistent efforts, even with high-intensity workouts or strict diets on select days, often fail to yield results, emphasizing the importance of daily, sustainable habits.
Hair Thinning, Menstrual Irregularities, and Emotional Impact in PCOD/PCOS
One of the major concerns observed in women with PCOD/PCOS is the thinning of hair on the scalp. Many patients report that despite regularly using hair growth oils, the hair continues to become thin and weak. This indicates that the issue is not external but internal. While hair oils may provide temporary nourishment to the scalp, they cannot correct the underlying hormonal or nutritional imbalances that cause hair thinning. The primary factors contributing to scalp and hair issues in PCOD include deficiencies in vitamins, minerals, and proteins. These deficiencies must be addressed through proper dietary management and nutritional intake. Once the body’s internal nutrition is corrected, issues like scalp thinning, hair breakage, and weak hair growth can be controlled effectively. Relying solely on external treatments like oils is insufficient because the root cause lies within the internal hormonal and nutritional imbalance, which requires dietary correction and supportive natural interventions.
Another prominent symptom of PCOD is the irregularity of the menstrual cycle. This symptom manifests differently in different individuals. Some women may not experience periods at all, even though their bodies have matured and should be menstruating regularly. On the other hand, some women may experience excessively heavy bleeding, which can last far longer than the typical 4–5 days. In some cases, the heavy flow can persist for 20 to 50 days, significantly disrupting normal life and daily routines. These irregularities are not just a physical concern—they directly impact a woman’s reproductive health, often leading to fertility problems. Women with PCOD/PCOS may find it challenging to conceive naturally due to irregular ovulation and hormonal imbalances caused by the disorder.
The impact of PCOD/PCOS extends beyond the physical symptoms and deeply affects the psychological and emotional well-being of women. Persistent physical changes such as heavy menstrual bleeding, irregular cycles, acne, hirsutism, and hair thinning can lead to depression, low self-confidence, and emotional distress. Women may feel frustrated or embarrassed about their appearance or their inability to maintain a regular cycle. The prolonged bleeding or the complete absence of periods can result in stomachaches, backaches, and discomfort, making it difficult for women to concentrate on daily tasks or professional responsibilities.
For those women whose periods do not occur at all, or for whom menstruation is extremely irregular, the symptoms can include bloating, fatigue, lethargy, and numbness, making them feel lazy or low in energy throughout the day. These women often experience reduced motivation and difficulty focusing on both personal and professional tasks, which further reduces their self-confidence. Even when minor remedies or medications are applied, unless the internal hormonal imbalance and nutritional deficiencies are addressed, these symptoms tend to persist or recur.
Overall, the combined effect of physical symptoms (hair thinning, acne, hirsutism, menstrual irregularity) and emotional stress (depression, loss of confidence, fatigue) makes PCOD/PCOS a complex condition that requires a holistic approach. This approach must focus on:
- Correcting internal nutritional deficiencies including vitamins, minerals, and proteins.
- Managing hormonal imbalance through lifestyle, diet, and natural interventions.
- Supporting emotional and mental well-being, addressing stress, depression, and loss of self-confidence caused by the chronic and visible symptoms of PCOD/PCOS.
This detailed understanding emphasizes that PCOD/PCOS is not just a superficial problem, like hair fall or acne, which can be managed externally. Instead, it is a systemic issue, where the body’s internal hormonal and nutritional environment plays a critical role in both the physical manifestations and the emotional impact experienced by women. Proper dietary correction, consistent lifestyle management, and targeted natural remedies are essential to mitigate these symptoms effectively, restore hormonal balance, and improve both physical health and mental well-being.
Medical Consultation, Investigations, and Causes of PCOD
Women experiencing PCOD often suffer from emotional distress and depression, which arises due to the ongoing physical and hormonal changes in their body. It is crucial to monitor and recognize the early symptoms of PCOD to prevent long-term complications. Any unusual changes in the body, particularly irregular periods or abnormal weight gain, should prompt immediate medical consultation. Even if the changes appear over one or two months, it is advisable to consult a doctor promptly rather than waiting for the symptoms to worsen.
Investigations and Diagnostic Measures:
When a patient visits a doctor with suspected PCOD, several investigations and tests are typically conducted to determine the underlying causes and severity of the condition. These investigations help the doctor design an appropriate treatment plan. The commonly performed tests include:
- Sugar Estimation:
- Conducted to check insulin sensitivity and detect early signs of insulin resistance.
- Insulin resistance is a common feature in PCOD, contributing to weight gain and metabolic disturbances.
- Thyroid Hormone Testing:
- Hypothyroidism or other thyroid disorders can aggravate PCOD symptoms.
- Assessing T3, T4, and TSH levels helps identify whether the thyroid is contributing to hormonal imbalance.
- Pelvic Ultrasound:
- Used to examine the ovaries and pelvic region for any cysts or structural abnormalities.
- This test helps in confirming the presence of polycystic ovaries and assessing their size and condition.
- Hormonal Assessment:
- Measurement of serum androgens (male hormones) and Luteinizing Hormone (LH) levels.
- Elevated androgens and LH levels are indicators of PCOD and help in tailoring hormonal treatment.
These investigations allow doctors to detect hormonal imbalances early and provide appropriate medication or interventions to manage the condition effectively. Timely diagnosis helps prevent the escalation of complications such as severe obesity, metabolic disorders, infertility, and psychological distress.
Causes of PCOD:
PCOD develops due to a combination of hormonal, metabolic, genetic, and lifestyle factors. The primary contributing factors include:
- High Levels of Androgens:
- Androgens are male hormones that are naturally present in females but at lower levels.
- Excessive androgen production in women leads to acne, hirsutism, irregular periods, and hair thinning.
- Low-Grade Inflammation:
- Inflammation in the body, often influenced by heredity, contributes to hormonal imbalance and the development of cysts in the ovaries.
- High Insulin Levels and Insulin Resistance:
- Increased insulin levels can stimulate excess androgen production in the ovaries, worsening PCOD symptoms.
- Insulin resistance is strongly associated with weight gain, obesity, and metabolic disturbances in affected women.
- Obesity:

- Obesity is both a cause and a consequence of PCOD.
- Excess weight aggravates hormonal imbalance, leading to further irregularities in menstrual cycles and metabolic health.
By understanding these causes, women can take proactive measures to manage PCOD through proper diet, lifestyle changes, and medical interventions, in addition to monitoring and controlling hormonal levels under professional guidance.
Causes of PCOD: Hormonal Imbalance, Heredity, and Medical Factors
Understanding the root causes of PCOD is essential for providing appropriate treatment. Each individual may have different contributing factors, so it is important to consult a doctor to identify the specific cause in each case. PCOD is not a condition that can be generalized or treated the same way for everyone. While some women may experience PCOD due to physical inactivity or poor diet, others may develop it due to heredity, underlying medical conditions like thyroid disorders, or other hormonal imbalances. Proper evaluation allows the doctor to rule out the underlying causes and provide treatment targeted to the specific problem, rather than applying a generic solution.
In women, the primary responsibility of producing sex hormones lies in the ovaries. Females mainly produce female sex hormones, but they also produce small amounts of male sex hormones, called androgens. While androgen levels in females are naturally low, an increase in androgen production can lead to significant problems in the body. Androgens in females play a role in regulating the natural development of eggs in the ovaries during the menstrual cycle. Proper hormonal balance ensures healthy ovulation and the development of healthy ovaries.
However, in PCOD, this hormonal balance is disrupted, leading to an increase in androgen production. This imbalance affects ovulation in several ways:
- Irregular Ovulation:
- Ovulation may not occur on time or may occur inconsistently.
- In some cases, the ovaries produce multiple cysts or abnormal follicles instead of a mature egg.
- Ovulation may even stop completely in certain cases, preventing normal menstrual cycles.
- Physical Manifestations of Hormonal Imbalance:
- The excess androgens result in visible symptoms such as acne and unusual or excessive hair growth (hirsutism) on the body.
- These physical signs often appear immediately after hormonal changes, signaling the internal imbalance to the individual.
It is common for many women to ignore early warning signs. For example, if a period is missed for a day or even a month, many women assume it is due to stress or temporary changes, and postpone seeking medical advice. However, the body often displays external symptoms, such as pimples, acne, or excessive hair growth, as soon as internal hormonal imbalance occurs. These visible signs are an indication that ovulation and hormonal regulation are disrupted, and early consultation with a doctor is necessary to prevent worsening of PCOD symptoms.
The root causes of PCOD are closely linked to hormonal imbalance, particularly the overproduction of male sex hormones (androgens) in females. This hormonal imbalance affects ovulation, disrupts the menstrual cycle, and leads to the visible symptoms of acne, excessive hair growth, and other manifestations. Early recognition and prompt medical consultation are essential to identify the cause and manage the condition effectively, preventing long-term complications such as infertility, metabolic disorders, and psychological stress.
Ovulation, Follicle Maturity, and Development of PCOD
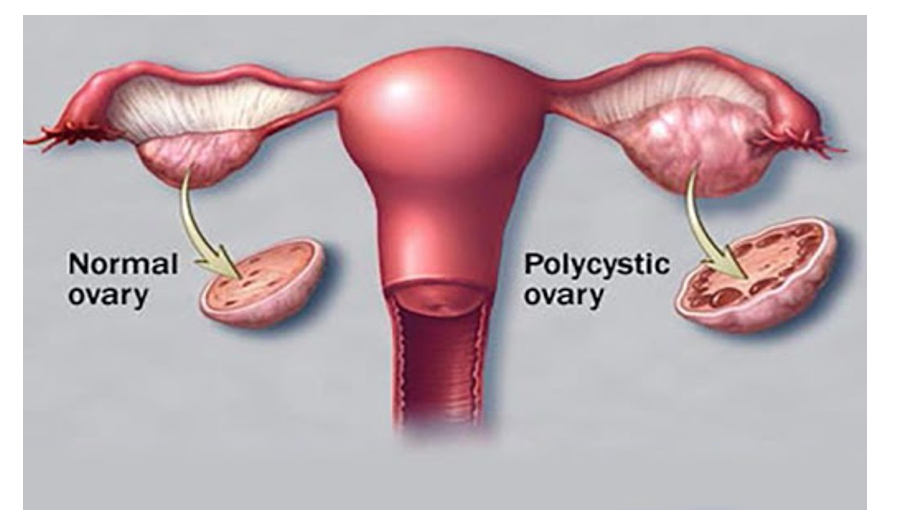
A critical process affected in PCOD and PCOS is ovulation, which is the release of eggs from the ovaries. The ovaries contain sack-like structures called follicles, and each follicle contains a female egg. During a normal menstrual cycle, one or more of these eggs are released from the follicles at the time of ovulation. This process of releasing a mature egg is essential for regular menstruation and fertility.
In women with PCOD or PCOS, the eggs inside these follicles fail to attain full maturity. During a normal cycle, which typically lasts about 25 days, the eggs in the follicles should mature and be released from the ovaries. However, due to hormonal imbalance and increased androgen levels, the eggs fail to mature properly. Instead of being released during ovulation, these immature follicles form small cysts in the ovaries.
- These cysts accumulate around the ovary, giving rise to the term polycystic ovarian disease (PCOD).
- The presence of multiple cysts on the ovaries is a hallmark of PCOD and is the direct result of disrupted ovulation.
Genetic and Hereditary Factors:
PCOD often appears to run in families, indicating a hereditary component. Women with PCOD may have inherited the condition from their mothers or close family members, such as maternal aunts. Additionally, a family history of irregular periods or diabetes may increase the likelihood of developing PCOD. This shows that both genetic predisposition and hereditary factors play an important role in the development of the disease.
The hereditary nature of PCOD emphasizes the need for early screening and monitoring in girls whose mothers or close female relatives have experienced irregular menstruation, diabetes, or PCOD symptoms. Early identification allows for timely interventions and lifestyle modifications, which can help reduce the severity of symptoms and prevent long-term complications such as infertility, metabolic disorders, and obesity.
By understanding the process of ovulation, follicle maturation, and cyst formation, it becomes clear why PCOD develops and how it manifests in the body. Disruption in the natural ovulatory cycle leads to the accumulation of immature follicles, which is central to the pathophysiology of PCOD.
Transition to PCOS:
While PCOD primarily refers to the presence of multiple cysts in the ovaries caused by irregular ovulation, polycystic ovary syndrome (PCOS) encompasses a broader spectrum of hormonal and metabolic disturbances. PCOS is often considered more severe than PCOD and includes additional systemic effects beyond the ovaries, which will be discussed in the next section.
Polycystic Ovary Syndrome (PCOS): Definition, Hormonal Imbalance, and Risks
While PCOD primarily involves the formation of cysts on the ovaries due to irregular ovulation, PCOS is a more complex syndrome that affects women’s hormonal balance during their reproductive years, typically between 12 and 45 years of age. Unlike PCOD, which can often be managed effectively through diet, physical activity, and lifestyle changes, PCOS involves more severe hormonal disturbances that require early detection and careful management to prevent long-term complications.
PCOS occurs due to imbalances in hormone secretion, either in the form of excessive hormone production or insufficient hormone production. Women with PCOS may experience very irregular menstrual cycles, including:
- Infrequent periods, where menstruation may occur only once every few months.
- Prolonged periods, which may last for an unusually long duration.
- Absence of periods for years in severe cases.
A hallmark of PCOS is the excess secretion of male hormones (androgens). Women with PCOS have higher androgen levels compared to normal, which contributes to:
- Hirsutism (excess hair growth on the face and body)
- Acne
- Hair thinning on the scalp
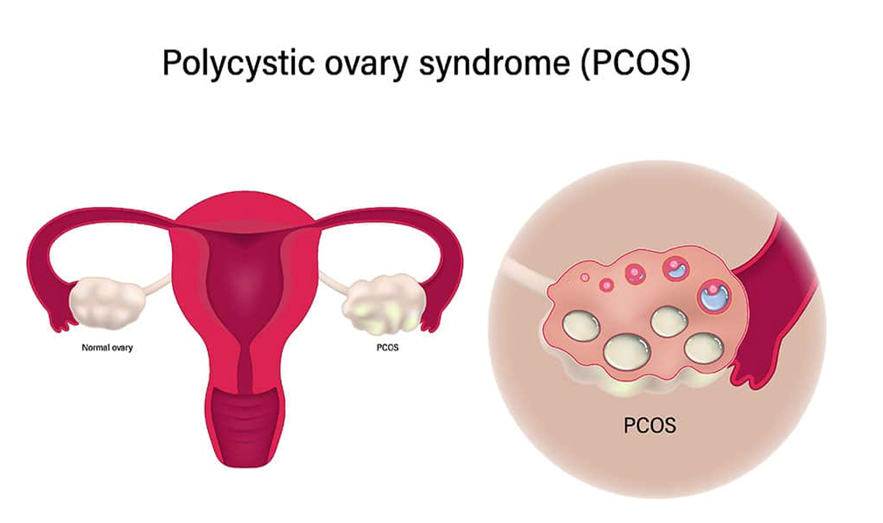
Ovarian Changes in PCOS:
In PCOS, small fluid-filled sacs develop along the outer edge of the ovaries. These small sacs, also called follicles, contain immature eggs that fail to mature or release regularly. While PCOD may involve one or two larger cysts, PCOS typically presents with multiple small follicles distributed along the ovary, which prevents regular ovulation. This severely reduces the chances of natural conception:
- In PCOS, approximately 90% of affected women may face difficulties in conceiving due to irregular or absent ovulation.
- The eggs remain immature, and ovulation is inconsistent, further complicating fertility.
Causes and Diagnosis:
The exact cause of PCOS remains unknown, though it is understood to involve hormonal imbalance, genetic predisposition, and metabolic disturbances. Because PCOS affects multiple systems in the body, early diagnosis and intervention are crucial. Prompt detection allows women to manage symptoms, improve fertility, and reduce the risk of serious long-term complications.
Long-Term Risks of PCOS:
Unlike PCOD, which can often be controlled with diet, exercise, and minor medical interventions, PCOS carries significant risks beyond fertility issues, including:
- Type 2 diabetes due to insulin resistance.
- Heart disease and cardiovascular complications.
- Obesity, which further exacerbates hormonal imbalance and metabolic disturbances.
Importance of Medical Consultation:
Given the potential severity of PCOS, it is essential to consult a doctor immediately if any symptoms are observed. Proper investigations, including hormonal assessments, ultrasound examinations, and metabolic screenings, help distinguish between PCOD and PCOS. Early identification of PCOS is critical not only for conceiving naturally but also for preventing long-term health complications like diabetes and heart disease.
While PCOD can often be managed through dietary adjustments, physical activity, and limited medication, PCOS is a broader hormonal syndrome requiring early diagnosis, careful monitoring, and comprehensive management to avoid serious health consequences. Awareness of the condition, prompt medical consultation, and sustained lifestyle changes are essential steps for women at risk of PCOS.
Key Symptoms of PCOS: Menstrual Irregularities, Hirsutism, Acne, and Metabolic Risks
Women with PCOS often experience a range of severe symptoms that affect both reproductive and metabolic health. Some of the key and most noticeable symptoms include:
- Severe Menstrual Irregularities:
- Women may have very irregular periods, with cycles that are unpredictable.
- Some women experience excessively heavy bleeding, while others may have light or absent menstruation.
- Periods may last longer than usual, and some women may skip months, getting periods only 9 times in a year or with cycles 35–40 days apart.
- Because of these irregularities, fertility is affected, and women may experience trouble conceiving.
- Excess Facial and Body Hair (Hirsutism):
- Women may develop male-like facial hair, including hair on the chin, upper lip, and cheeks.
- Hair growth can also occur on the arms, legs, and other parts of the body, which is a direct result of excess androgen production.
- This condition is medically referred to as hirsutism and is one of the distinguishing features of PCOS.
- Persistent Acne:
- Women with PCOS often experience severe acne, which can appear on the face, neck, and back.
- Acne in PCOS is typically resistant to standard treatments, as it is driven by hormonal imbalance rather than superficial skin issues.
- Obesity and Difficulty Losing Weight:
- Obesity is a common feature in PCOS, and weight loss becomes particularly challenging.
- Excess androgen and insulin resistance make it difficult for women to reduce body weight even with diet, physical activity, or exercise.
- Infertility:
- Due to irregular or absent ovulation, women with PCOS often experience difficulty getting pregnant.
- This is a significant concern for women seeking to conceive during their reproductive years.
- Higher Risk of Diabetes and Heart Disease:
- PCOS increases the risk of type 2 diabetes due to insulin resistance.
- Heart disease risk is elevated because of higher cholesterol levels and metabolic disturbances associated with the syndrome.
Onset of Symptoms:
- The symptoms of PCOS may begin at different stages of life.
- In some women, symptoms appear around the time of the first menstrual period, typically between 13–14 years of age.
- In others, symptoms develop later, often between 20–28 years of age, even after regular menstrual cycles have been established.
- This delayed onset can make early detection challenging, highlighting the importance of monitoring menstrual cycles and hormonal changes over time.
Diagnosis Criteria:
- Diagnosis of PCOS is usually made when a woman exhibits at least two of the following key features:
- Irregular or infrequent periods.
- Clinical signs of excess androgen, such as hirsutism, severe acne, or male-pattern baldness.
- Polycystic ovaries on ultrasound, showing multiple immature follicles along the ovary’s outer edge.
Because the early symptoms of PCOS often resemble PCOD, such as irregular periods and mild hair growth, women and healthcare providers may initially confuse the two conditions. Many women may assume they have PCOD and attempt to manage it through diet and activity alone. However, PCOS requires specific evaluation and management, as it carries a higher risk of metabolic and reproductive complications compared to PCOD.
Real-Life Case Examples: Hidden Symptoms of PCOS and Androgen Imbalance
PCOS can often go undetected for years because its symptoms may not always align with commonly expected signs such as obesity or irregular periods. Many women assume they are healthy simply because their weight is normal and menstrual cycles appear regular. However, the underlying hormonal imbalance can still have significant consequences, especially due to excess androgen production.
For instance, consider a 24-year-old woman diagnosed with PCOS:
- She had regular menstrual periods and maintained a healthy, thin body weight. On the surface, she seemed perfectly healthy and was unaware of any internal hormonal imbalance.
- Despite this, she displayed excessive male-pattern hair growth (hirsutism), including a beard-like growth on her face, as well as hair on her arms, legs, and other parts of her body.
- She had not realized that these symptoms were indicative of PCOS. She initially denied the condition, thinking that regular periods and ideal body weight meant her hormones were normal.
This case illustrates that PCOS is not always linked to obesity or irregular menstruation. Many women may have normal weight and still suffer from high androgen levels, which manifest in physical symptoms such as:
- Excessive facial and body hair (hirsutism)
- Melasma or hyperpigmentation, particularly on the face, caused by increased melanin production triggered by hormonal imbalances
- Acne, though in some cases melasma may appear without acne
Another example can be seen in PCOD patients:
- Women with PCOD generally have mild hair growth and more noticeable symptoms such as obesity or irregular periods.
- In contrast, women with PCOS, like the case of the 24-year-old, can appear otherwise healthy with regular periods and normal body weight, making the condition easily overlooked.
Challenges in Patient Awareness and Treatment:
One of the major challenges in PCOS management is patient awareness. Many women do not understand that male hormones (androgens) are present in small amounts in females and that excess androgen production can lead to serious symptoms. In the example discussed:
- The patient initially refused internal treatment, focusing only on cosmetic concerns such as facial hair removal.
- She was hesitant to address the underlying hormonal imbalance, even after guidance to undergo tests such as testosterone measurement.
- This lack of awareness and reluctance to pursue full treatment highlights a broader issue: many women do not seek medical consultation for PCOS, even when experiencing obvious symptoms like hirsutism or melasma.
Importance of Awareness Programs:
This case emphasizes the critical need for awareness programs to educate women about the differences between PCOD and PCOS. While PCOD is often more obvious due to weight gain, irregular periods, and acne, PCOS may remain hidden for years despite significant internal hormonal imbalance. Proper education helps women:
- Recognize subtle signs of PCOS, even when menstrual cycles are regular.
- Understand the risks associated with excess androgen production, including infertility, type 2 diabetes, heart disease, and metabolic disturbances.
- Seek timely hormonal evaluation and treatment, including blood tests for testosterone and other androgens, even if physical appearance seems normal.
Key Lessons from the Case Study:
- PCOS can occur in women with normal weight and regular periods.
- Excess androgen levels may be present even in young, thin women.
- Visible symptoms like hirsutism or melasma may be the only indicators of the condition.
- Patient awareness and acceptance of the condition are often low, hindering early diagnosis and treatment.
- Medical guidance is essential, not only for cosmetic issues but also to prevent long-term metabolic and reproductive complications.
PCOS is a complex condition that can be hidden even in women who appear healthy. Excess androgen production manifests through hirsutism, hyperpigmentation, and other physical signs, often without obvious menstrual or weight-related symptoms. Patient education, early screening, and hormonal evaluation are vital to ensure proper diagnosis and prevent complications. This case clearly demonstrates that external appearance alone cannot rule out PCOS, and medical assessment is necessary even for women with seemingly normal cycles and body weight.
Polycystic Ovaries, Obesity, and Causes of PCOS
In PCOS, the ovaries undergo distinct structural changes that are often visible on ultrasound scans. These changes include:
- Enlarged ovaries, which may appear bigger than normal.
- Multiple follicles along the outer edge of the ovary, each containing immature eggs.
- The ovaries may not function properly, disrupting the regular process of ovulation and hormone production.
When a pelvic scan or ultrasound is performed, these enlarged ovaries filled with immature eggs are often clearly visible. The follicles remain immature, preventing normal egg release, which is a central feature of PCOS.
Impact of Obesity on PCOS Symptoms
The severity of PCOS signs and symptoms is often influenced by body weight:
- In thin women, the primary visible symptom may be excessive hair growth (hirsutism), while other symptoms such as irregular periods, acne, or hair thinning may be absent.
- In contrast, obese women with PCOS often experience more severe symptoms, including:
- Irregular periods due to disrupted ovulation.
- Acne, often persistent and hormone-related.
- Male-pattern baldness or thinning hair on the scalp.
- Metabolic complaints, which may include weight gain, difficulty losing weight, and insulin resistance-related issues.
Despite the presence of such visible and distressing symptoms, many women do not seek hormonal evaluation. They may attribute issues like hair problems, acne, or hair fall to external factors such as water quality, hair care products, or stress, rather than recognizing the underlying hormonal imbalance.
Causes of PCOS
The exact cause of PCOS remains unknown, but several contributing factors have been identified. One of the most significant is insulin resistance:
- Insulin Resistance and Hyperinsulinemia:
- Insulin is a hormone produced by the pancreas that allows the body’s cells to absorb and use glucose for energy.
- When the body’s cells become resistant to insulin, blood glucose levels rise, and the pancreas produces more insulin in an attempt to lower blood sugar.
- Excess insulin in the bloodstream can stimulate the ovaries to produce more male hormones (androgens).
- High androgen levels interfere with normal ovulation, leading to irregular or absent periods and the formation of immature follicles in the ovaries.
One visible sign of insulin resistance is the appearance of dark, velvety patches of skin, often on the back of the neck or other body folds. This symptom can serve as an early indicator that a woman may be at risk of developing PCOS or metabolic complications.
Connection Between Insulin Resistance and Hormonal Imbalance:
Insulin resistance not only disrupts blood sugar regulation but also directly affects reproductive hormones:
- High insulin levels stimulate the overproduction of male hormones (androgens).
- Excess androgens lead to physical symptoms such as hirsutism, acne, and male-pattern hair loss.
- Hormonal imbalance interferes with follicle maturation and ovulation, preventing the regular release of eggs from the ovaries and contributing to the formation of polycystic ovaries.
Insulin resistance forms a critical link between metabolic dysfunction and reproductive disturbance in women with PCOS. Even without obesity, women with insulin resistance may experience androgen excess and ovulatory dysfunction, highlighting the importance of early detection and management.
Hyperpigmentation, Low-Grade Inflammation, and Hereditary Factors in PCOS
One of the common but often overlooked symptoms of PCOS is dark pigmentation in body folds, which can occur across various age groups, from young adolescents to adults in their 30s or 40s.
Hyperpigmentation in Folded Areas:
- Darkened skin often appears in folded areas such as the neck, underarms, under the breasts, inner thighs, and groin.
- Many people mistake this pigmentation for sun exposure, but in PCOS, it is actually hormone-related, particularly due to excess androgen and insulin resistance.
- Both females and males can experience this type of pigmentation if they have underlying hormonal imbalances.
- Hyperpigmentation is usually accompanied by increased appetite, weight gain, and sometimes obesity, reflecting the metabolic dysfunction often seen in PCOS.

Low-Grade Inflammation:
- PCOS is also associated with a condition called low-grade inflammation, which differs from the normal short-term inflammatory response to infection or injury.
- Typically, white blood cells produce substances to protect the body during injury or infection. This response is short-lived and ends once healing occurs.
- In PCOS, research suggests that there is a long-term, chronic low-grade inflammation in the body.
- This chronic inflammation stimulates the polycystic ovaries to produce excess androgens, contributing to many physical and metabolic symptoms, including hirsutism, acne, and insulin resistance.
- Over time, chronic low-grade inflammation may also increase the risk of cardiovascular problems, affecting the heart and blood vessels.
Hereditary Factors:
- PCOS has a genetic component, meaning it can run in families.
- Studies suggest that certain genes may predispose individuals to PCOS, increasing the likelihood of developing the condition if there is a family history.
- Women with mothers, maternal aunts, or close female relatives affected by PCOS or menstrual irregularities may have a higher risk of experiencing similar hormonal and metabolic issues.
- Hereditary influence highlights the importance of early screening in families with a known history of PCOS.
Summary of These Contributing Factors:
- Hyperpigmentation in body folds is a visible sign of hormonal imbalance and insulin resistance.
- Low-grade inflammation contributes to excessive androgen production and increases the risk of long-term cardiovascular and metabolic complications.
- Hereditary factors may predispose individuals to PCOS, making family history an important aspect of early diagnosis and management.
By understanding these additional features of PCOS, women can become more aware of subtle signs beyond irregular periods or weight gain, and recognize when medical evaluation is necessary. Early recognition of these factors—especially in adolescents or young adults—can help prevent the progression of hormonal imbalance, metabolic disorders, and reproductive complications.
Additional Causes and Comprehensive Symptoms of PCOS
While the exact cause of PCOS remains not fully understood, ongoing research has identified multiple contributing factors. Among these, hereditary predisposition and excess androgen production are particularly significant.
Excess Androgen Production:
- In PCOS, the ovaries may produce abnormally high levels of androgens, which are male hormones present in small amounts in females.
- Excess androgens interfere with normal ovulation, preventing the release of mature eggs from the follicles.
- As a result, eggs fail to develop properly and are not released, leading to infertility or difficulties in conceiving.
- High androgen levels also contribute to physical symptoms such as hirsutism (excessive male-pattern hair growth) and severe acne, both of which are often some of the earliest visible signs of PCOS.
- The previously discussed case of a 24-year-old woman with facial hair and body hair growth exemplifies the effects of androgen excess, even when other symptoms such as weight gain or irregular periods are absent.
Common Signs and Symptoms of PCOS:
PCOS manifests through a combination of reproductive, metabolic, and dermatological symptoms. These include:
- Menstrual Irregularities:
- Oligomenorrhea: Irregular periods occurring every 35–40 days or even longer, sometimes skipping months.
- Amenorrhea: Complete absence of menstruation for 4–6 months or more.
- Menorrhagia: Excessive or prolonged menstrual bleeding lasting 15–20 days or in some cases up to 30–40 days.
- Dermatological Symptoms:
- Acne on the face, back, and other parts of the body, often persistent and hormone-related.
- Hirsutism: Excessive hair growth in areas typically associated with males, including the face, arms, legs, and chest.
- Hair loss (female-pattern baldness): Thinning of hair on the scalp, sometimes progressing to baldness.
- Hyperpigmentation: Darkened skin in folded areas such as the neck, underarms, under the breasts, inner thighs, and groin.
- Skin tags: Small, soft growths in areas like the neck, underarms, and face, appearing in red or brown shades.
- Freckles: Increased pigmentation in certain areas, often exacerbated by hormonal imbalance.
- Metabolic and Physical Changes:
- Weight gain or obesity, particularly in the abdominal area, which can worsen PCOS symptoms.
- Difficulty losing weight, even with proper diet and exercise, due to hormonal imbalance.
- Reproductive Symptoms:
- Infertility caused by irregular or absent ovulation.
- Failure of the eggs to mature and be released properly from the follicles.
- Psychological and Mood-Related Changes:
- Mood swings, depression, fatigue, and decreased self-confidence, often resulting from physical changes, hormonal imbalance, and reproductive challenges.
The combined effects of excess androgen, insulin resistance, hereditary factors, and low-grade inflammation contribute to the complex symptom profile of PCOS. Women with PCOS may experience:
- Irregular, absent, or excessive menstruation
- Acne, hirsutism, and female-pattern hair loss
- Hyperpigmentation, skin tags, and freckles
- Weight gain and obesity
- Infertility and ovulatory dysfunction
- Mood changes, depression, and reduced self-confidence
Recognizing these multiple symptoms together is essential for early diagnosis. Since PCOS can affect both reproductive and metabolic health, it is important for women to seek medical evaluation promptly, rather than attributing isolated symptoms to lifestyle factors or minor cosmetic concerns.
Complications of PCOS
Polycystic Ovary Syndrome (PCOS), if left untreated or unmanaged, can lead to a range of serious health complications, affecting reproductive, metabolic, and cardiovascular systems. Understanding these complications is essential for early detection and timely intervention.
- Infertility and Reproductive Complications:
- One of the primary complications of PCOS is infertility, resulting from irregular ovulation or complete absence of ovulation.
- Even if women with PCOS conceive, they are at higher risk for pregnancy-related complications, including:
- Gestational diabetes: This occurs due to insulin resistance, which is already a common feature in PCOS. High blood sugar levels during pregnancy can affect both the mother and the baby.
- Pregnancy-induced hypertension (PIH): Excess cholesterol and metabolic imbalance can lead to arterial stiffness, resulting in high blood pressure during pregnancy.
- Miscarriages: The hormonal and metabolic disturbances in PCOS increase the risk of early pregnancy loss.
- Premature birth: Infants may be delivered early due to complications arising from maternal metabolic or hormonal issues.
- Liver Complications:
- PCOS is associated with non-alcoholic fatty liver disease (NAFLD), where fat accumulates in the liver even in individuals who do not consume alcohol.
- Fatty liver can progress from mild (Grade 1) to severe (Grade 3), with higher grades causing significant liver dysfunction.
- If left unchecked, fatty liver may lead to non-alcoholic steatohepatitis (NASH), which can cause inflammation, fibrosis, and long-term liver damage.
- Metabolic Syndrome:
- Women with PCOS are at increased risk of developing metabolic syndrome, a cluster of conditions that include:
- High blood pressure (hypertension)
- High blood sugar (hyperglycemia) due to insulin resistance
- Unhealthy cholesterol and triglyceride levels (dyslipidemia)
- Metabolic syndrome significantly increases the risk of cardiovascular diseases, including heart attacks, strokes, and atherosclerosis.
- The combination of obesity, insulin resistance, high cholesterol, and hypertension in PCOS creates a synergistic effect, exacerbating the likelihood of long-term health issues.
If PCOS is neglected or not managed with medical guidance, the following complications can occur:
- Reproductive: Infertility, gestational diabetes, pregnancy-induced hypertension, miscarriages, and premature births.
- Liver-related: Non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH).
- Metabolic and Cardiovascular: Metabolic syndrome, high blood sugar, high blood pressure, unhealthy cholesterol levels, and increased risk of heart disease.
These complications highlight the importance of early detection, proper lifestyle management, and timely medical intervention. Women with PCOS should not ignore irregular periods, hormonal changes, or metabolic symptoms, as these can develop into serious long-term health risks.
Additional Complications of PCOS
Polycystic Ovary Syndrome (PCOS) is not just a reproductive disorder but a systemic hormonal and metabolic condition that can lead to numerous complications if untreated. Understanding these complications can help in early detection, timely intervention, and long-term health maintenance.
- Type 2 Diabetes and Pre-Diabetes
- Women with PCOS are at a significantly higher risk of developing type 2 diabetes or pre-diabetes.
- This is primarily due to insulin resistance, where the body’s cells do not respond effectively to insulin.
- As a result, blood sugar levels remain elevated, forcing the pancreas to produce more insulin.
- Excess insulin in the body can further increase androgen levels, worsening PCOS symptoms and increasing the risk of diabetes.
- Sleep Disorders

- Obesity, common in PCOS, can lead to sleep apnea, a condition characterized by interrupted breathing during sleep.
- Sleep apnea reduces sleep quality, causing fatigue, irritability, and poor concentration during the day.
- Chronic sleep issues also contribute to hormonal imbalance, weight gain, and worsening insulin resistance, forming a vicious cycle.
- Mental Health Issues
- PCOS significantly impacts mental and emotional health due to physical changes, hormonal imbalance, and metabolic stress.
- Common mental health complications include:
- Depression due to chronic symptoms like irregular periods, acne, and excessive hair growth.
- Anxiety, especially regarding body image, fertility concerns, and weight issues.
- Eating disorders, which may manifest as overeating or undereating, further worsening obesity and metabolic imbalance.
- Endometrial (Uterine Lining) Cancer
- In rare cases, PCOS increases the risk of endometrial cancer.
- This is caused by prolonged exposure to estrogen without the balancing effect of progesterone due to irregular ovulation.
- Untreated hormonal imbalances allow the uterine lining to grow excessively, which can, over time, increase the risk of cancer.
- Awareness and early medical intervention are critical to prevent this severe complication.
Differences Between PCOD and PCOS
Understanding the differences between PCOD (Polycystic Ovarian Disease) and PCOS (Polycystic Ovary Syndrome) is essential because these conditions, although related, differ in severity, hormonal imbalance, ovarian changes, and treatment approaches.
- Hormonal Imbalance
- PCOD: Involves mild hormonal imbalance, which can often be managed effectively with diet, exercise, and lifestyle modifications.
- PCOS: A complex hormonal disorder. While diet and activity are supportive, medical treatment is essential to correct severe hormonal imbalance, particularly high androgen levels and ovulatory dysfunction.
- Ovarian Changes
- PCOD: Characterized by the presence of multiple small cysts in the ovaries. These cysts result from irregular ovulation and can often be corrected with lifestyle management.
- PCOS: A syndrome that includes multiple systemic symptoms:
- Irregular periods
- Weight gain
- Acne
- Excess hair growth (herocetism)
- Mood changes, skin changes, and metabolic issues
- The ovaries in PCOS may have numerous immature follicles along the outer edge, which fail to mature and release eggs regularly, making the condition more complex and serious.
- Seriousness and Long-Term Impact
- PCOD: Considered less serious, as it is primarily a hormonal disorder manageable with diet, exercise, and moderate medical support.
- PCOS: Considered more severe, with high androgen levels, ovulatory dysfunction, and systemic complications.
- PCOS can adversely affect fertility due to irregular ovulation.
- It increases the risk of type 2 diabetes, heart disease, metabolic syndrome, and endometrial cancer.
- Early detection and treatment of PCOS are critical to prevent long-term health complications.
- Management Approaches
- PCOD: Can often be controlled through regular diet, consistent physical activity, and healthy lifestyle choices. Hormonal support may be required but is usually mild.
- PCOS: Requires medical intervention, including hormonal therapy, insulin regulation, and sometimes fertility treatment. Lifestyle management alone is insufficient for PCOS, although it supports treatment outcomes.
- PCOD and PCOS are often confused but differ significantly in causes, severity, ovarian changes, and treatment approaches.
- PCOD is primarily influenced by diet, lifestyle, and mild hormonal imbalance and can be corrected with consistent lifestyle modifications.
- PCOS is a complex metabolic and hormonal syndrome, with severe systemic implications including:
- High androgen levels
- Ovulatory dysfunction
- Insulin resistance
- Obesity-related complications
- Cardiovascular and liver risks
- Potential reproductive challenges
- Awareness, early diagnosis, and timely medical intervention are critical in managing PCOS to prevent severe long-term health issues.
Reversibility of PCOD and PCOS:
One of the most significant differences between PCOD and PCOS is their reversibility, which directly impacts how each condition is managed and treated.
PCOD, or Polycystic Ovarian Disease, is primarily a hormonal imbalance. It occurs due to factors such as poor diet, irregular lifestyle, lack of physical activity, stress, and sometimes mild medical issues. Because the hormonal imbalance in PCOD is generally mild and functional, it can be effectively reversed with proper intervention. Reversal typically involves consistent and balanced dietary habits, regular physical activity, adequate sleep, and stress management. Mild medical support or hormone regulation may also be necessary in some cases. When these interventions are followed consistently, the ovaries can resume normal functioning, ovulation becomes regular, and symptoms such as irregular periods, acne, weight gain, and excessive hair growth gradually improve.
In contrast, PCOS, or Polycystic Ovary Syndrome, is a complex endocrine disorder that involves severe hormonal imbalance, metabolic disturbances, and systemic complications. Unlike PCOD, PCOS cannot be easily reversed with lifestyle changes alone. Effective management requires medical intervention, including hormone therapy, medications for insulin resistance, and sometimes fertility treatments. Regular monitoring and follow-up are critical to managing symptoms such as irregular or absent periods, excessive androgen levels, severe acne, infertility, and obesity. While lifestyle modifications like diet and exercise support treatment and improve overall health, medical management is essential to address the underlying endocrine and metabolic dysfunction in PCOS.

Commonality and Prevalence:
PCOD is more common than PCOS. Clinical observations suggest that approximately one-third of women experience PCOD during their reproductive years, typically between the ages of 12 and 45. PCOS, while less common, is increasingly being diagnosed due to lifestyle changes, rising obesity rates, and hereditary factors. Though less prevalent, PCOS is more serious because of its systemic and long-term health implications.
Overall Distinctions and Implications:
Understanding the differences between PCOD and PCOS is essential for accurate diagnosis, treatment planning, and prevention of complications.
PCOD involves mild hormonal imbalance, is generally reversible, and can often be managed effectively with lifestyle modifications and dietary interventions. Women with PCOD may experience irregular periods, mild acne, slight weight gain, and some hair growth, but these symptoms are usually manageable and do not lead to severe long-term complications if treated early.
PCOS, on the other hand, is more severe, involving high androgen levels, ovulation dysfunction, metabolic disturbances, and systemic complications. It can cause persistent irregular periods, excessive facial and body hair, severe acne, obesity, insulin resistance, fertility issues, and increased risk of diabetes, heart disease, liver problems, and endometrial cancer. Early diagnosis and timely medical intervention are critical in PCOS to prevent these complications. Lifestyle changes can support treatment, but medical management remains essential, as PCOS cannot be fully controlled through diet and activity alone.
Overall, the distinctions between PCOD and PCOS are critical because they influence how treatment is approached, how early intervention is prioritized, and how long-term health outcomes are safeguarded. While PCOD can often be corrected through consistent lifestyle and diet changes, PCOS demands structured medical care alongside lifestyle support to manage its hormonal, reproductive, and metabolic effects.
Occurrence and Prevalence
Historically, PCOS (Polycystic Ovary Syndrome) was considered a rare condition, with very few cases reported about 10–15 years ago. At that time, most healthcare providers and patients rarely encountered PCOS, and it was not widely recognized. In contrast, PCOD (Polycystic Ovarian Disease) has been much more common, affecting approximately one-third of women in the population. PCOD has been routinely observed in clinics, primarily because it arises from more prevalent lifestyle-related and metabolic factors.
However, in recent years, PCOS is becoming increasingly common, even though many people are still unaware of the condition. This rise in prevalence is partially due to lifestyle changes, dietary patterns, stress, obesity, and hereditary factors. Awareness about the differences between PCOD and PCOS remains limited, and many women continue to confuse the two conditions, which can delay proper diagnosis and treatment.
Definition and Nature of the Conditions
PCOS is primarily an endocrine disorder of the ovaries. It is characterized by the presence of immature follicles, which are sacs containing eggs that fail to develop and release properly. These endocrine disturbances affect hormonal balance, ovulation, and metabolic function, and the ovaries may produce only a few cysts. In contrast, PCOD is primarily a metabolic disorder. It arises from hormonal imbalance and is associated with the development of multiple ovarian cysts, often 10 or more per ovary. These cysts result from irregular ovulation and hormonal disruptions but are largely manageable through lifestyle interventions.
Causes and Contributing Factors
The causes of PCOS are predominantly genetic, accounting for nearly 70% of cases, though lifestyle, dietary habits, and mental health factors also play a role. In PCOS, the genetic predisposition leads to endocrine disruption, increased androgen production, and ovulation issues that are difficult to reverse without medical intervention.
In PCOD, the causes are more varied and often modifiable. Key contributing factors include genetic predisposition, insulin resistance, low-grade inflammation, weight issues, and lifestyle-related habits. Unlike PCOS, the majority of these factors in PCOD can be managed or corrected with consistent diet, physical activity, stress management, and targeted medical support if required.
Severity and Reversibility
The severity of PCOS is higher than PCOD because it involves complex endocrine dysfunction, high androgen levels, and ovulation irregularities, making it difficult to reverse. Medical intervention is crucial for managing PCOS, as lifestyle and diet alone are insufficient to correct the hormonal and metabolic abnormalities.
PCOD, on the other hand, is easily reversible. With proper diet, exercise, and consistent lifestyle management, the hormonal imbalance can be corrected. Medication can be used as needed to assist with ovulation and symptom management. In some cases, surgery may be considered, but it is rarely necessary if PCOD is identified and managed early.
Treatment Approaches
For PCOS, treatment primarily relies on medical intervention to regulate hormones, manage insulin resistance, and support ovulation. Lifestyle modifications such as diet and activity are important but secondary to medical management.
For PCOD, treatment focuses on lifestyle modification, including balanced diet, regular physical activity, and weight management. Medication is used as a supportive measure when required, and in most cases, PCOD responds well to these interventions. Surgery is considered only in rare, severe cases.
Complications and Risks
Both PCOD and PCOS can impact fertility, but the severity differs. Women with PCOD can often conceive within a few months with proper treatment, including medication to regulate ovulation. In contrast, PCOS is associated with more significant fertility challenges due to high androgen levels, immature follicles, and ovulatory dysfunction.
Other complications in PCOS include a higher risk of type 2 diabetes, high blood pressure, obesity, metabolic syndrome, and endometrial cancer. PCOD carries a lower risk for such severe complications, as timely intervention with diet, lifestyle, and medication generally prevents long-term health issues.
Major Differences Between PCOD and PCOS
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) may seem similar at first glance, but they have several important differences in terms of pathophysiology, hormonal imbalance, cyst formation, prevalence, and health impact. Understanding these distinctions is critical for proper diagnosis, treatment, and long-term health management.
PCOD is generally not considered a severe problem and is highly manageable with lifestyle modifications and minor medical assistance. In PCOD, the ovaries release immature or partially developed eggs, which leads to the formation of small cysts. On an ultrasound scan, these cysts are easily visible as multiple small structures on the ovary. In contrast, PCOS involves larger, more pronounced ovaries, and it is a complex endocrine and metabolic disorder. In PCOS, multiple cysts grow around both ovaries, disrupting ovulation and leading to more severe reproductive and metabolic issues.
Prevalence also differs between the two conditions. PCOD is much more common, affecting nearly one-third of women, whereas PCOS has historically been less common, affecting about 2–2.5% of women worldwide, although recent trends indicate that its prevalence is rising. PCOD typically begins during adolescence or early reproductive years, whereas PCOS may begin in adolescence but often presents more pronounced symptoms in women aged 20–30 years.
Hormonal imbalances are another key distinction. In PCOD, there is a mild hormonal imbalance, primarily affecting the female hormones estrogen and progesterone. PCOS, however, involves a significant hormonal imbalance, including elevated androgen levels and an increase in male hormones, which can lead to more severe symptoms such as hirsutism, acne, and irregular ovulation.
Cyst formation also differs between the two conditions. In PCOD, the ovaries may contain a few small cysts that can often shrink with proper diet and lifestyle changes, making management relatively straightforward. In PCOS, the ovaries develop larger cysts that do not resolve with lifestyle or diet alone, requiring medical intervention for effective treatment.
The menstrual cycle is affected differently as well. In PCOD, periods may be slightly delayed or irregular, but with minor medication, women often achieve regular cycles quickly. In PCOS, menstrual irregularities are more severe, often resulting in highly irregular or completely absent periods. Additionally, hirsutism (excessive hair growth) is more prominent in PCOS due to elevated androgen levels.
Impact on fertility also highlights the differences. In PCOD, infertility is rare, and about 95% of women with PCOD can conceive naturally or with minor medical assistance, resulting in healthy pregnancies. In PCOS, infertility is much more common due to disrupted ovulation and hormonal imbalances. Even in cases where pregnancy occurs, there is a higher risk of miscarriage, preterm birth, and other complications.
Weight management differs between the two conditions as well. PCOD often involves weight gain, but it is usually manageable through consistent lifestyle changes, diet, and physical activity. In PCOS, weight gain can be more significant and may occur even in women with normal weight, making the condition harder to detect. Moreover, PCOS patients often experience difficulty losing weight or maintaining weight, primarily due to insulin resistance and metabolic disturbances.
Finally, the metabolic impact of these two conditions varies considerably. In PCOD, metabolic effects are minimal, and insulin resistance is less pronounced. In PCOS, there is a strong association with metabolic syndrome, which includes insulin resistance, type 2 diabetes, high cholesterol, and an increased risk of cardiovascular disease. These metabolic complications make PCOS a more serious long-term health concern compared to PCOD.
Health Complications, Emotional Impact, and Treatment Approaches in PCOD vs. PCOS
When comparing PCOD (Polycystic Ovarian Disease) and PCOS (Polycystic Ovary Syndrome), one of the key distinctions lies in the severity of health complications.
In PCOD, health complications are generally mild and manageable. They usually do not lead to severe or long-term health issues unless the condition is completely neglected. Women with PCOD may experience minor symptoms such as oily skin, mild acne, occasional hair thinning, and mild irregular periods. These issues are often visible early on, and timely intervention with lifestyle modifications can prevent progression to serious complications.
In contrast, PCOS is more severe and can result in serious health complications. PCOS is associated with metabolic, cardiovascular, and reproductive issues, including type 2 diabetes, hypertension, heart disease, and endometrial cancer. Women with PCOS also experience severe skin and hair problems, such as persistent acne, excess facial and body hair (hirsutism), hair thinning, and female-pattern baldness. These symptoms are far more pronounced than in PCOD and often cause significant distress.
Emotional and Psychological Impact
The emotional impact of these two conditions also differs. In PCOD, mood swings may occur due to irregular periods, but they are usually mild, and the stress is often manageable. Women may feel slight anxiety or mild stress about their appearance or menstrual irregularities.
In PCOS, however, women frequently experience emotional stress, depression, and anxiety, often as a result of severe acne, excessive hair growth, infertility issues, and metabolic complications like high blood sugar, high cholesterol, and high blood pressure. These symptoms can significantly affect self-confidence and overall mental health.
Treatment Approaches
PCOD treatment primarily focuses on lifestyle changes. Doctors generally recommend:
- Weight loss and maintaining a healthy body weight
- Balanced diet, reducing sugar and processed foods
- Regular exercise, including aerobic activity or yoga
- Stress management through relaxation techniques, meditation, and sleep regulation
Medication may be prescribed if necessary, but often diet, activity, and lifestyle adjustments are sufficient to regulate symptoms and restore hormonal balance. With timely intervention, PCOD symptoms are often reversible, and improvements can typically be seen within one to two months.
PCOS treatment, on the other hand, is more complex and requires both lifestyle modifications and medical intervention. Key aspects include:
- Hormonal therapy to manage androgen levels and control excessive hair growth and acne
- Addressing metabolic issues, particularly insulin resistance, through diet, exercise, and sometimes medication
- Weight management to prevent excessive insulin production, which directly affects androgen levels
- Regular monitoring and medical follow-ups to manage long-term risks such as diabetes, heart disease, and endometrial cancer
While PCOS cannot be fully reversed, its symptoms can be effectively managed with consistent medical care, disciplined lifestyle, and dietary adherence.
Reversibility and Long-Term Risks
- PCOD: Hormonal imbalances are mild and reversible with proper intervention. Long-term risks of chronic diseases are minimal if treatment is timely.
- PCOS: Endocrine and metabolic disruptions are not reversible, and long-term risks include serious chronic diseases affecting major organs, such as the heart, liver, and reproductive system. Management requires ongoing medical supervision, lifestyle consistency, and patient patience.
Fertility and Pregnancy

Fertility management differs as well:
- PCOD: Fertility issues are rare. Most women can conceive naturally or with minor medical assistance. Pregnancy outcomes are generally healthy.
- PCOS: Fertility is often compromised due to irregular or absent ovulation. Pregnancy may involve complications such as miscarriages, premature births, or difficulty conceiving, even with medical support. Lifestyle changes similar to PCOD are important, but medical intervention is more critical in PCOS.
In essence:
- PCOD is a mild, manageable hormonal disorder primarily corrected through lifestyle and minor medication, with low long-term risk.
- PCOS is a serious endocrine and metabolic disorder, requiring medical treatment, hormonal therapy, and lifestyle management, with higher risks for chronic diseases and reproductive complications.
Both conditions require timely recognition and consistent management, but the severity, reversibility, and long-term impact differ significantly. Awareness, early diagnosis, and patient education are crucial to prevent complications and improve quality of life.
Treatment Approaches for PCOS
After understanding the differences between PCOD and PCOS, it’s essential to know how to manage and treat these conditions. While some treatment approaches overlap, it is crucial to first determine whether a person has PCOD or PCOS, because the severity, underlying causes, and medical requirements differ.
For PCOS, the treatment primarily revolves around a combination of lifestyle management and medical care. Nothing should cause panic—PCOS is manageable with discipline and consistency. The key steps include:
- Lifestyle Management:
- Maintain a structured diet, focusing on whole grains, vegetables, lean protein, and low sugar intake. Avoid processed and high-glycemic foods.
- Engage in regular physical activity, including walking, yoga, aerobic exercises, and strength training. Consistency is far more important than intensity; even 15–30 minutes daily can be effective if followed regularly.
- Stress management is crucial. Practice meditation, mindfulness, or other relaxation techniques to regulate hormonal balance.
- Medical Intervention:
- PCOS often requires hormonal therapy to manage high androgen levels, regulate menstrual cycles, and improve ovulation.
- Insulin-sensitizing medications may be prescribed to control insulin resistance, prevent excessive androgen production, and reduce the risk of metabolic syndrome.
- Regular check-ups for blood sugar, cholesterol, liver function, and reproductive hormones are important to monitor the progression of the condition.
Naturopathy and Herbal Interventions for PCOS
In addition to lifestyle and medical care, Ayurvedic and organic herbal tonics can support hormonal balance, menstrual regularity, and overall reproductive health. Some of the effective herbal remedies include:
- Ashokarista
- Origin: Made from the bark of the Ashoka tree, a well-known herb in Ayurvedic medicine.
- Benefits:
- Helps regulate menstrual cycles.
- Balances reproductive hormones.
- Reduces pelvic pain associated with irregular or heavy periods.
- Dosage: Take 2 tablespoons twice daily after meals with water.
- Application: Useful for both PCOD and PCOS, particularly in controlling irregular periods.
- Triphala

- Origin: A classical Ayurvedic formulation containing Amalaki, Haritaki, and Bibhitaki.
- Benefits:
- Acts as a natural colon cleanser, promoting detoxification.
- Helps balance hormones by reducing excess metabolic waste in the body.
- Supports digestive health, which indirectly benefits reproductive and endocrine function.
- Dosage: Commonly taken as a powder or tablet form once daily at night, ideally with warm water.
- Additional Herbal Support (optional supplements based on need):
- Shatavari (Asparagus racemosus): Supports reproductive health, regulates ovarian function, and balances estrogen levels.
- Neem: Helps reduce inflammation and supports detoxification of the liver, indirectly supporting hormonal balance.
- Cinnamon and Fenugreek: Can help regulate blood sugar levels and improve insulin sensitivity, which is especially beneficial in PCOS.
Consistency is Key
Regardless of whether using lifestyle, medical, or herbal approaches, the most important factor in managing PCOS is consistency:
- Diet and exercise must be followed regularly and not intermittently.
- Herbal remedies like Ashokarista and Triphala should be taken as prescribed daily.
- Medical follow-ups must be scheduled to monitor hormones, insulin, and reproductive health.
Even though PCOS cannot be fully reversed, maintaining a disciplined lifestyle, following medical guidance, and supporting the body with herbal tonics can:
- Improve hormonal balance
- Control excessive hair growth and acne
- Regulate menstrual cycles
- Reduce insulin resistance
- Minimize long-term complications such as diabetes, heart disease, and endometrial issues
Detoxification and Fluid Intake During PCOS/PCOD Management
When managing PCOS or PCOD, especially while taking medications or following a structured activity regimen, the body can accumulate toxins as a byproduct of hormonal imbalance, increased metabolism, and cellular activity. This buildup can interfere with the effectiveness of treatment and slow down recovery. Therefore, detoxification is a key supportive strategy in the management of these conditions.
Importance of Adequate Fluids
Consuming adequate fluids helps in:
- Flushing out toxins produced during metabolism and hormonal adjustments.
- Maintaining hydration, which is critical for proper hormonal function, digestion, and elimination.
- Supporting kidney and liver function, which are essential for natural detoxification.
Recommended Fluids:
- Water: At least 2–3 liters daily.
- Coconut Water: Hydrating and full of electrolytes.
- Buttermilk: Supports digestion and balances gut bacteria.
- Lemon Water: Helps stimulate liver detoxification and improves digestion.
- Barley Water: Supports kidney function and reduces bloating.
- Soups, stews, and natural juices: Provide hydration along with nutrients.
Tip: The goal is not just plain water, but a variety of liquids to improve detoxification and nutrient absorption. Aim for around 4 liters of total fluids in a day in different forms.
Triphala – A Natural Detoxifier
Triphala is a classical Ayurvedic formulation, composed of three fruits:
- Haritaki
- Bibhitaki
- Amalaki
Benefits of Triphala:
- Colon cleanser: Improves bowel regularity and removes accumulated waste.
- Supports digestion: Reduces bloating, constipation, and heaviness in the abdomen.
- Toxin removal: Helps flush out harmful metabolites generated during metabolic activity and medication usage.
- Improves overall gut health: A healthy gut contributes to better hormonal balance and enhanced nutrient absorption.
Usage:
- Take 1 teaspoon of Triphala powder mixed with warm water at night before bed.
- For those who prefer convenience, Triphala is also available in tablet or capsule form.
Key Note: Triphala is especially helpful when combined with adequate liquid intake as it helps in natural cleansing of the body, improving metabolic efficiency and enhancing the benefits of diet, exercise, and medications.
In the management of PCOD and PCOS, detoxification is an important yet often overlooked aspect. Proper hydration combined with natural detoxifiers like Triphala:
- Supports digestion and elimination of toxins.
- Reduces bloating and abdominal discomfort.
- Complements medical and lifestyle interventions.
- Enhances overall treatment outcomes, ensuring hormones, metabolism, and ovulation processes are supported effectively.
Ayurvedic and Herbal Support for PCOD and PCOS
In addition to lifestyle changes and medical management, Ayurvedic herbs and tonics can play a supportive role in balancing hormones, improving metabolism, and aiding fertility in women with PCOD and PCOS. These natural remedies complement conventional therapy and help detoxify the body while minimizing side effects.
1. Triphala – Natural Detoxifier
- Purpose: Triphala is a classic Ayurvedic formulation that acts as a natural colon cleanser and detoxifier.
- Composition: Made of three fruits – Haritaki, Bibhitaki, and Amalaki.
- Benefits:
- Improves digestion and reduces bloating.
- Removes toxins accumulated in the body due to hormonal imbalance and metabolic changes.
- Supports regular bowel movements and enhances nutrient absorption.
- Dosage:
- Powder: 1 teaspoon mixed with warm water at night.
- Tablet/Capsule: Can also be taken as per convenience.
- Duration: Continuous use is safe as it is a natural herbal product with no side effects.
Note: Detoxification is particularly important during PCOD/PCOS treatment as medications and lifestyle changes increase metabolism and toxin production. Adequate liquid intake (water, coconut water, buttermilk, lemon water, barley water, soups, juices) should accompany Triphala for optimal detox benefits.
2. Shatavari – Hormone Balancer

- Purpose: Shatavari is a powerful female tonic in Ayurveda.
- Benefits:
- Balances estrogen levels.
- Nourishes and supports the reproductive system.
- Enhances fertility and menstrual regularity.
- Dosage:
- Powder: 1 teaspoon with warm milk or warm water.
- Capsule: As per recommended dosage.
- Use: Effective for both PCOD and PCOS due to its hormone-balancing properties.
3. Virana – Ayurvedic Detox Therapy
- Purpose: Virana is a Panchakarma detox therapy available at naturopathy and Ayurvedic clinics.
- Benefits:
- Removes excess Pitta and toxins from the liver and gut.
- Improves metabolism and hormonal balance.
- Particularly helpful for patients with constipation or metabolic buildup.
- Recommendation: Should be performed under professional supervision as part of holistic PCOD/PCOS management.
4. Spearmint (Peppermint) Tea – Anti-Androgenic Support
- Purpose: Spearmint tea acts as a natural anti-androgen.
- Benefits:
- Reduces excessive male hormones (androgens) in women.
- Helps manage unwanted facial and body hair.
- Improves menstrual regularity.
- Useful for men with hormonal imbalances, e.g., gynecomastia.
- Dosage: 1–2 cups daily.
5. Giloy (Guruchi) – Immunity and Detox Herb
- Purpose: Giloy is a detoxifying and immunity-boosting herb.
- Benefits:
- Balances hormones and improves insulin sensitivity.
- Cleanses the liver and supports metabolic health.
- Aids in controlling weight gain and insulin resistance in PCOD/PCOS patients.
- Dosage: 1 capsule or 1 teaspoon of juice daily.
- Additional Use: Can be taken by healthy individuals 3–4 times per month to maintain normal insulin levels and liver health.
Lifestyle Modifications for PCOD/PCOS
Ayurveda emphasizes daily habits (Dinacharya) for optimal hormonal and metabolic health. Consistency is key.
Daily Routine Recommendations:
- Wake up before 7:00 a.m.
- Engage in regular exercise and yoga
- Eat freshly cooked meals, avoiding cold and oily foods
- Sleep before 10:00 p.m.
- Practice stress management techniques, including meditation and mindful breathing
Yoga for PCOD/PCOS
Certain yoga poses are highly beneficial for improving blood flow to the pelvic region, reducing stress, and supporting hormonal balance. Regular practice can complement Ayurvedic and medical treatments.
Recommended Poses:
- Butterfly Pose (Baddha Konasana): Opens the pelvic area and improves ovarian function.
- Cobra Pose (Bhujangasana): Stimulates abdominal organs and improves metabolism.
- Bridge Pose (Setu Bandhasana): Strengthens pelvic muscles and supports reproductive organs.
- Sun Salutations (Surya Namaskar): Enhances circulation, reduces stress, and promotes overall metabolic health.
Tip: Yoga and exercise should be performed regularly and consistently rather than sporadically to achieve maximum benefits.
The combination of herbal tonics, detox therapies, proper hydration, lifestyle management, and yoga creates a comprehensive approach to managing PCOD and PCOS. While medications are important for PCOS, these natural interventions:
- Support hormonal balance
- Reduce androgen excess
- Improve fertility
- Detoxify the body
- Manage weight and insulin sensitivity
Consistency and early intervention are key to preventing complications and maintaining reproductive and metabolic health.
NPCOD – Fenugreek Seed, Flax Seeds, and Jeera
Some of fenugreek seeds and flax seeds these are very much important in our diet and also jeera, which helps in digestion. So, fenugreek helps in improving the insulin levels and also balances the hormones in PCOD. It may also aid in weight loss.
So fenugreek and flax seeds, jeera water—this is very much important whether our children or we, whether we are suffering with any hormonal issues or not. On a healthy basis, when we start giving the children from 6 years of age, a little bit about fenugreek seed powder, flax seed powder for female children—then this will be very good so that they will not have a problem in maturity and page problem.
So fenugreek helps to improve insulin levels, balance hormones in PCOD, and also it may also aid in weight loss.
How to use:
- Soak one teaspoon of seeds overnight and drink the water in the morning.
- We can make a powder, we can powder it and use it, or if not, we can soak it and have only water.
Ayurvedic Diet Plan for PCOD (Based on Doshic Type)
So coming to the diet plan based on Ayurveda, like following a PCOD diet based on your DSHA. We need to know clearly which DSA we come from, like Vata, Pitha, and Kapha Dsha.
- Know what type of body type we have and accordingly follow it.
- Avoid foods which are not suitable for our body.
- Identify anti-inflammatory foods and unsuitable foods over two to three months and come to a conclusion.
Recommended Foods:
- Eat more whole grains, fruits, and vegetables.
- Include ghee, flax seeds, and turmeric.
Foods to avoid:
- Processed, sugary, and dairy-rich foods.
- Sugar and dairy products—check if there is lactose intolerance.
Notes:
- In few conditions like PCOD and PCOS, when milk or milk-related products are stopped, it shows much improvement.
- Sugar and milk products can be avoided based on individual tolerance.
Naturopathy Approach: Eat to Heal, Not to Fill
We have to eat what can heal our body, improve our immune system, and detoxify the body. Food is a medicine.
PCOD Treatment via Diet:
- Supports hormone balance and lowers insulin resistance.
- Avoid refined/simple carbohydrates like white bread, sugar, and snacks.
- Switch to complex carbohydrates with low glycemic index (GI): lentils, oats, barley, brown rice, and ragi.
- Anti-inflammatory foods: berries, turmeric, spinach, avocado.
- Healthy fats: nuts, seeds, ghee, olive oil.
Morning Routine:
- Start your day with soaked fenugreek seeds, cinnamon water, jeera water, club water, and flax seeds.
- Important from 6 to 7 years of age.
- Both fenugreek and flax seeds are powerful in regulating insulin levels and addressing the root cause of PCOS.
Move Your Body – Gentle and Consistent Exercise
- Daily exercise should be consistent, not too much or too little.
- Half an hour of walking every day, whether working or taking leave, should be maintained.
- Avoid over-exercising—it can spike cortisol, worsening PCOS.
What works best:
- 30 minutes of walking
- Yoga poses that improve flexibility and reduce stress: Butterfly Pose, Cobra Pose, Bridge Pose, Surya Namaskar.
- Meditation: 10–15 minutes daily.
- Strength exercises: 2–3 times per week to build muscle and improve insulin sensitivity.
- Dancing: relaxing and increases activity gently.
Avoid sporadic long sessions like 2–3 hours one day and none the next; consistency is key.
- Seeds, herbs, and water help regulate insulin and hormones.
- Ayurvedic diet supports detoxification and reduces inflammation.
- Gentle, consistent movement improves metabolic and hormonal health.
- Meditation and stress management support overall hormonal balance.
Say Hello to Herbal Helpers: Natural Remedies for PCOD and PCOS
PCOD (Polycystic Ovarian Disease) and PCOS (Polycystic Ovary Syndrome) are conditions affecting women’s hormonal balance, menstrual cycles, and overall health. While lifestyle, diet, and medical intervention are essential, natural herbs and remedies can support treatment and help manage symptoms effectively.
Herbal Helpers and Their Benefits
Herbs are natural and generally safe. Even if taken in higher quantities, they rarely cause severe side effects, though some people may experience mild diarrhea initially. Incorporating herbs in your diet—through water, tablets, or powders—can help control hormonal imbalances.
Ashwagandha (Withania somnifera)
Ashwagandha is well-known for reducing stress and cortisol levels. Studies in 2019 found that taking 240 mg of ashwagandha daily significantly lowered stress and cortisol levels in the blood. Unlike placebo treatments, which provide only temporary relief, consistent intake of ashwagandha offers long-term benefits in controlling stress-related hormonal imbalances.
Spearmint Tea
Spearmint tea helps reduce androgen levels, which are often elevated in PCOS. This herb can support hormonal balance and reduce excessive facial or body hair in women.
Licorice Root
Licorice root may support estrogen balance, although more research is needed. It can contribute to hormonal regulation and improved reproductive health.
Importance of Sleep
Sleep is crucial for hormone regulation and overall health. Chronic lack of sleep can worsen insulin resistance and negate the benefits of diet, herbs, and lifestyle interventions. Adults should aim for 7–9 hours of sound sleep every night. Screens should be avoided at least one hour before bed, and calming activities such as meditation or herbal teas like chamomile or lavender can promote relaxation.
Dairy and Protein Considerations

Women with PCOS may notice improvements in acne, bloating, and menstrual regularity when reducing or eliminating dairy products, especially if they are lactose intolerant or sensitive to casein. Protein intake should remain sufficient, but milk may need to be limited depending on individual tolerance.
Seed Cycling
Seed cycling is a simple, food-based method to balance hormones naturally. It involves consuming specific seeds during different phases of the menstrual cycle:
- Follicular Phase (Day 1–14): Flax seeds or pumpkin seeds, which can be consumed as powders, soaked overnight, or added to dishes.
- Luteal Phase (Day 15–28): Sunflower seeds or sesame seeds, consumed similarly.
Benefits of Seed Cycling:
- Balances estrogen and progesterone levels
- Reduces excess androgens through zinc content
- Supports thyroid function
- Improves insulin sensitivity
- Lowers cholesterol levels
These seeds also provide omega-3 fatty acids, which are beneficial for heart and metabolic health.
Managing Stress
Chronic stress negatively affects ovulation. Even with proper diet, exercise, and herbal treatments, stress can disrupt hormonal balance. Daily practices such as 10 minutes of breathing exercises, counseling, or hobbies like coloring and painting can help reduce stress. Maintaining a calm mind supports ovarian function and overall reproductive health.
Insulin Management
Insulin resistance is a major factor in PCOD symptoms. High sugar intake triggers excess insulin production, which worsens hormonal imbalances. To manage insulin levels:
- Eat smaller, frequent meals
- Pair carbohydrates with protein (e.g., apple with nut butter, rice with dal)
- Include apple cider vinegar before meals (1 teaspoon in water, if no ulcers exist)
Herbal interventions, proper sleep, seed cycling, stress management, and diet modifications all work together to support hormonal balance in women with PCOD and PCOS. While these methods may not completely cure the conditions, they can significantly reduce symptoms and improve overall well-being. Consistency and a holistic approach are key to managing these hormonal disorders effectively.
Natural and Lifestyle-Based Approaches for PCOD and PCOS
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are common hormonal disorders affecting women’s reproductive health, metabolism, and overall well-being. Along with conventional treatments, natural remedies, lifestyle modifications, and mindful practices can play a significant role in managing these conditions effectively.
Apple Cider Vinegar and Digestion
Apple cider vinegar can aid digestion and help regulate blood sugar. However, patients should not have any existing digestive problems before using it. A typical recommendation is one teaspoon in water before meals, provided there are no ulcers or sensitivity issues.
Barberry Plant Compound: A Natural Alternative
Barberry plant compounds have shown promise as a natural alternative to metformin in women with PCOD/PCOS. Studies indicate that these compounds can help improve insulin sensitivity and support metabolic balance, providing a natural approach for managing PCOS symptoms.
Detox Your Lifestyle and Environment
Environmental factors and everyday products can significantly affect hormonal health. Reducing exposure to endocrine-disrupting chemicals (EDCs) is crucial. Some practical steps include:
- Use paraben- and phthalate-free skincare and cosmetics
- Switch to natural cleansing products
- Store food in glass containers instead of plastic to avoid BPA (Bisphenol A), a compound linked to hormonal disruption
Minimizing chemical exposure supports hormonal balance and overall reproductive health.
Cycle Syncing: Aligning Lifestyle with Menstrual Phases
Understanding the four phases of the menstrual cycle—menstrual, follicular, ovulation, and luteal—can help women tailor their lifestyle, nutrition, and self-care routines:
- Adjust food intake according to hormonal needs
- Incorporate cycle-supportive nutrients
- Align exercise intensity with your cycle
- Prioritize rest during specific phases
Cycle syncing has been shown to reduce PMS symptoms, improve energy levels, and support fertility. Women can manage their stress, sleep, diet, and exercise according to each phase, promoting both hormonal and overall well-being.
Dietary Approaches for PCOD/PCOS
A whole-foods-based diet is essential for managing PCOD/PCOS. Focus on:
- Whole foods: Fruits, vegetables, legumes, and whole grains
- Complex carbohydrates: Provide stable blood sugar and insulin control
- High biological value protein: Supports muscle and hormone production
- Anti-inflammatory foods: Berries, turmeric, spinach, avocado
Whole foods are free from artificial sugars and preservatives. Combining complex carbohydrates with protein, fiber, and healthy fats (e.g., ghee or olive oil) creates balanced meals. For example, a meal of rice, dal, vegetables, spices, and ghee provides complex carbohydrates, protein, and micronutrients.
Managing Carbohydrate Intake
Carbohydrates influence blood sugar and insulin levels, which are crucial in PCOD/PCOS management. Women should:
- Avoid simple/refined carbs (white bread, sugar, snacks)
- Prefer complex carbs (oats, barley, ragi, lentils)
- Combine carbs with protein and fiber to maintain stable glucose levels
This approach helps control insulin resistance, weight gain, and associated metabolic issues.
Anti-Inflammatory Approach
PCOS is often considered a chronic inflammatory condition. Including anti-inflammatory foods in the diet can reduce systemic inflammation, support hormonal balance, and promote overall health.
Managing PCOD and PCOS requires a holistic approach: integrating diet, natural remedies, lifestyle modifications, and environmental detoxification. Natural compounds such as barberry, herbal tonics, and seed cycling, along with mindful habits like cycle syncing, stress management, and whole-foods consumption, can significantly reduce symptoms and improve overall quality of life. Consistency and discipline in these practices are key to maintaining long-term hormonal balance and metabolic health.
Dietary Strategies for Managing PCOD and PCOS
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are hormonal disorders that can significantly affect women’s reproductive and metabolic health. Alongside lifestyle and herbal interventions, diet plays a crucial role in managing symptoms, balancing hormones, and supporting overall well-being.
Anti-Inflammatory Foods
Consuming anti-inflammatory foods can help reduce the symptoms of PCOS. These include:
- Berries, leafy vegetables, and greens
- Fatty fish such as mackerel and tuna
- Nuts and olive oil
These foods not only reduce inflammation but also support hormone regulation, insulin sensitivity, and overall metabolic health.
Iron-Rich Foods for Hemoglobin Support
Women with PCOD/PCOS often experience excess menstrual bleeding, which can lead to iron deficiency and anemia. Maintaining adequate iron intake is essential to prevent life-threatening low hemoglobin levels.
Iron-rich foods to include in the diet:
- Spinach, eggs, liver, broccoli
- Ragi, rice flakes, jaggery, beetroot, pomegranate
Tip: Pair iron-rich foods with vitamin C sources (lemon, sweet lime, orange juice) to improve absorption. For example, spinach salad with a squeeze of lemon significantly enhances iron uptake.
Magnesium and Micronutrients
Magnesium is crucial for insulin regulation, restful sleep, and metabolic balance. Include magnesium-rich foods such as:
- Cashews, almonds, bananas, spinach
Other important nutrients for PCOS management:
- Zinc, Omega-3 fatty acids, Vitamins B1, B3, B6, B12, and C
These nutrients support hormonal balance, improve insulin sensitivity, and contribute to overall reproductive health.
Fiber for Digestion and Blood Sugar Control
High fiber intake is beneficial for digestion, bowel regularity, and sugar level control. Fiber-rich foods include:
- Lentils, lima beans, broccoli, Brussels sprouts, pears, avocado
Note: Excessive fiber without sufficient protein or carbohydrates may negatively affect hormonal balance. Balance is key.
Avoid Coffee and Caffeine
Caffeine can reduce absorption of iron and other nutrients and may stimulate estrogen production, leading to hormonal imbalance. Avoid coffee and replace it with:
- Green tea, lemon tea, ginger tea, or other herbal teas
These alternatives support insulin regulation and weight management while avoiding negative hormonal effects.

Incorporating Soy Products
Soy-based foods are excellent for vegetarians and help in maintaining estrogen balance and normal hormone secretion. Include:
- Soy protein, tofu, soy milk, miso (fermented soybean paste used in soups and stews)
Note: Individuals with soy allergies should avoid these products.
A well-planned diet for PCOD/PCOS focuses on:
- Anti-inflammatory foods for hormonal balance
- Iron-rich foods with vitamin C for hemoglobin support
- Magnesium, zinc, omega-3, and B vitamins for insulin and hormonal balance
- Adequate fiber for digestion and sugar control
- Avoiding coffee and replacing it with herbal teas
- Incorporating soy-based proteins for vegetarians
By combining these dietary strategies with lifestyle modifications, exercise, herbal interventions, and proper sleep, women with PCOD/PCOS can achieve better hormone regulation, improved metabolic health, and symptom relief.
Comprehensive Natural Management of PCOD and PCOS
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are common hormonal disorders affecting women’s reproductive and metabolic health. Alongside lifestyle interventions, diet, exercise, sleep, and herbal remedies play a vital role in symptom management, hormone regulation, and overall wellness.
Soy and Fermented Soy Products
Soy products are a natural source of plant-based protein and can help balance estrogen and hormone secretion. Common soy foods include:
- Tofu, soy milk, miso (fermented soybean paste)
- Tempeh – an Indonesian fermented soy product pressed into firm blocks
Important caution: Women with estrogen-related conditions (e.g., breast cancer) should avoid soy products. Always consult a doctor before including soy in the diet to ensure it is safe and beneficial.
Avoid Junk and Oily Foods
Excessive junk and oily/fried foods contribute to:
- Weight gain
- Digestive issues
- Worsening PCOS symptoms
Recommendation: Replace unhealthy fats with small amounts of ghee in cooking. Adding ghee to rice or curries supports healthy fat metabolism and subcutaneous fat balance.
Exercise and Physical Activity
Consistent exercise is crucial for managing weight, reducing stress, and supporting hormone regulation. Guidelines include:
- At least 150 minutes of moderate exercise per week
- Activities should be enjoyable, not stressful
- Examples: walking, yoga, dancing, meditation, or exercises with friends/family
- Consistency helps control insulin levels and improves mental health
Enjoyable physical activity also supports peer engagement, reduces depression, and promotes overall well-being.
Sleep and Stress Management
Proper sleep cycles and stress management are essential for hormonal balance:
- Aim for 7–9 hours of sound sleep
- Maintain consistent sleep schedules regardless of work, school, or social events
- Stress reduction techniques: meditation, breathing exercises, adult coloring books, hobbies
Adequate sleep and reduced stress improve hormone regulation, insulin sensitivity, and overall PCOD/PCOS management.
Frequently Asked Questions (FAQs)
- What is the treatment for PCOD?
- Focus on diet, physical activity, regular exercise, and proper sleep
- Natural methods improve symptoms in most cases (80% diet/activity, 20% medication)
- Medications are rarely needed if lifestyle changes are followed consistently
- What is the treatment for PCOS?
- Similar to PCOD: low glycemic diet, herbal remedies, workouts, and sleep hygiene
- Medications like birth control pills and metformin may be used in severe cases
- Natural approaches support long-term health and reduce risk of heart, liver, or diabetic complications
- Can PCOD improve fertility naturally?
- Following diet and lifestyle changes for 2–3 months can help regulate periods and improve fertility
- Neglected cases may require medication for 6–12 months before conception
- Can PCOS be cured permanently with natural treatment?
- No, PCOS cannot be completely cured
- Symptoms can be managed effectively with natural strategies, diet, exercise, and herbal interventions
Key Takeaways for Natural Management
- Include soy and fermented soy products if safe
- Avoid junk and oily foods; use ghee moderately
- Maintain consistent exercise and enjoy your activities
- Ensure adequate sleep and manage stress
- Follow a low glycemic, anti-inflammatory diet with iron, magnesium, fiber, and essential micronutrients
- Use herbal remedies like spearmint tea and ashwagandha for hormonal balance
- Lifestyle management can reduce the need for medication and prevent long-term complications
By adopting a holistic, natural approach, women with PCOD or PCOS can achieve better hormone regulation, improve insulin sensitivity, and maintain overall health.
Understanding PCOD and PCOS: Natural and Ayurvedic Approaches
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are common hormonal disorders affecting women’s reproductive, metabolic, and overall health. While PCOS cannot be permanently cured, its symptoms, complications, and chronic conditions such as heart or liver issues can be controlled and even reversed with lifestyle, dietary, and Ayurvedic interventions.
Can Ayurveda Completely Cure PCOD/PCOS?
- Ayurveda does not claim permanent cure of PCOS, but regular treatments, dietary management, and lifestyle adjustments can help control symptoms effectively.
- Symptoms can be reversed, ovulation can improve, and risk of chronic complications can be reduced.
Timeline for Ayurvedic Treatment
- The duration of Ayurvedic therapy depends on:
- Individual body constitution (Prakriti)
- Severity of PCOD/PCOS
- Timing of when the patient approaches the doctor
- Typical results are observed within 3–6 months of consistent Ayurvedic treatment, including herbal remedies, dietary changes, and lifestyle modifications.
Safety of Ayurvedic Treatments
- Panchakarma: Safe and effective for PCOD, aids in detoxification, and supports overall hormonal balance.
- Ayurvedic Herbs with Modern Medicine: Always consult both your gynecologist and Ayurvedic doctor before combining treatments.
- Self-medicating with herbs bought online (e.g., Amazon) may cause side effects such as diarrhea or gastric issues.
- Inform doctors about any herbal treatment being followed to avoid confusion or unnecessary prescriptions.
Ayurveda and Fertility in PCOD/PCOS
- Ayurvedic herbs such as Shatavari and Ashoka help balance hormones and support ovulation.
- Detoxification and yoga therapy further enhance fertility naturally.
- Regular Ayurvedic care can improve chances of conception in women with PCOD/PCOS without relying solely on modern medications.
Key Takeaways
- Symptoms Management: While PCOS cannot be permanently removed, symptoms can be reversed and chronic complications can be prevented.
- Ayurvedic Control: Herbal treatments, dietary changes, detox therapies, and yoga can effectively regulate hormones and improve overall health.
- Integration with Modern Medicine: Always consult both Ayurvedic and modern doctors before combining treatments.
- Fertility Support: Ayurveda enhances natural fertility through ovulation regulation and hormonal balance.
- Patient Awareness: Early intervention and consistent treatment significantly improve outcomes.
By combining dietary management, herbal remedies, exercise, stress reduction, and proper sleep, women with PCOD and PCOS can achieve hormonal balance, improved fertility, and better overall health. Understanding the difference between PCOD and PCOS allows timely intervention, preventing long-term complications while maintaining a holistic approach to wellness.
Conclusion:
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are common hormonal disorders that can significantly affect women’s reproductive health, metabolic function, and overall well-being. While these conditions cannot be permanently cured, their symptoms and associated chronic complications—such as insulin resistance, obesity, heart, or liver problems—can be effectively managed and often reversed with a holistic, natural, and Ayurvedic approach.
Dietary management forms the cornerstone of treatment. Consuming low glycemic, anti-inflammatory foods, rich in protein, fiber, iron, magnesium, zinc, omega-3 fatty acids, and essential vitamins, helps regulate insulin levels, balance hormones, and improve overall metabolic health. Incorporating herbs like fenugreek, flax seeds, Ashwagandha, spearmint, and licorice root further supports hormonal balance and stress reduction. Practices such as seed cycling during menstrual phases, along with maintaining healthy iron and nutrient combinations, enhance fertility and manage menstrual irregularities.
Lifestyle interventions are equally important. Consistent physical activity, including yoga, walking, and strength exercises, aids insulin sensitivity, reduces stress, and helps maintain a healthy weight. Adequate sleep (7–9 hours), stress management, screen detox, and mindful self-care play a crucial role in regulating hormones and preventing symptom exacerbation. Avoiding harmful habits—such as excessive caffeine, processed foods, and exposure to endocrine-disrupting chemicals—further supports overall health.
Ayurvedic interventions provide additional support. Treatments like Panchakarma, herbal remedies, detoxification, and yoga can regulate hormonal imbalance, improve ovulation, and enhance fertility naturally. Ayurveda, combined with careful monitoring and consultation with modern medical professionals, ensures safe and effective integration of natural therapies with conventional treatments.
Ultimately, the best management strategy for PCOD and PCOS is a holistic approach: a combination of mindful eating, nutrient-rich diets, herbal supplementation, regular physical activity, stress management, proper sleep, and medical guidance. With consistent efforts over time, women can achieve hormonal balance, improved fertility, better metabolic health, and reduced risk of chronic complications, leading to a healthier and more empowered life.