Liver Cirrhosis
About one in 400 persons in the United States, according to scientists, have liver cirrhosis. Cirrhosis most frequently affects adults between the ages of 45 and 54 or roughly 1 in 200 of them. As the sixth largest cause of death in the country for adults aged 25 to 64, cirrhosis accounts for roughly 26,000 facilities annually in the United States.
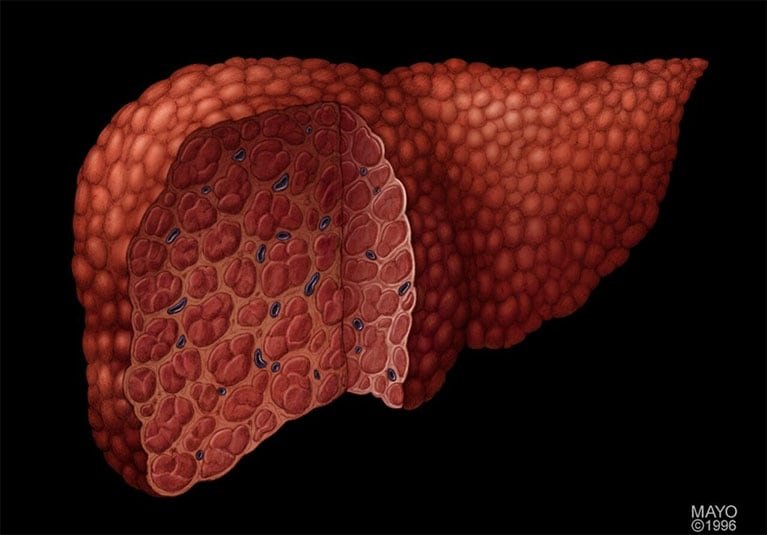
What is Liver Cirrhosis?
Cirrhosis is a severe form of liver disease in which good liver tissue is permanently replaced with scar tissue. Your liver is unable to function properly due to scar tissue. Many different liver disorders and diseases harm healthy liver cells, leading to cell death and inflammation.

Cell repair comes next, and after that comes tissue scarring as a byproduct of the repair process. The scar tissue reduces the liver’s capacity to handle nutrients, hormones, medicines, and natural toxins and limits blood flow through the liver (poisons). Additionally, it reduces the liver’s ability to produce proteins and other chemicals. Over time, cirrhosis prevents the liver from functioning normally. Cirrhosis in its advanced stages is fatal.
The condition of cirrhosis is not one that is inherited (transmitted from parent to kid). However, some of the conditions that might harm the liver and result in cirrhosis are inherited conditions.
Even if you have liver cirrhosis, you don’t necessarily need to seek emergency medical attention. But when cirrhosis worsens, additional scarring develops, and liver function keeps deteriorating. Your weakening liver may eventually develop into a life-threatening condition. There is nevertheless hope. If you are a candidate for a liver transplant, your medical team and you will talk about it. If so, the procedure for adding your name to the national registry of liver transplant candidates will start.
Who gets Cirrhosis, and who is at more risk?
The following factors increase your risk of developing liver cirrhosis:
- Long-term alcohol use.
- Have viral hepatitis.
- Have diabetes.
- Have obesity.


- Inject drugs using shared needles.
- Have a history of liver disease.
- Have unprotected sex.
Symptoms of Liver Cirrhosis:
According to the disease’s stage, cirrhosis symptoms vary. You might not exhibit any symptoms in the initial stages. Even if you experience symptoms, many are broad and can be easily confused for those of a wide range of other conditions.
The following are some early cirrhosis symptoms and signs:
- Appetite loss.
- Feeling drained or feeble.
- Nausea.
- Fever.
- Unanticipated weight loss

Other, more well-known signs of cirrhosis start to manifest as liver function declines, including:
- Simple bleeding and bruises
- Your skin or the whites of your eyes have a yellow tint (jaundice).
- Rough skin.
- Edema (swelling) in your ankles, foot, and legs.
- Fluid accumulation in your abdomen or belly (ascites).
- Your urine has a brownish or orange tint.
- Stool in a light colour.
- Confusion, brain fog, memory loss, and personality shifts.
- Stool with blood in it.
- Your hands’ palms may be red.
- Blood vessels that resemble spiders encircle tiny, red skin lesions (telangiectasias).
- Loss of sex desire, gynecomastia, and shrinking testicles are all symptoms in men.
- Premature menopause in women (no longer having your menstrual period).
Cirrhosis can be uncomfortable, particularly if the condition worsens. Up to 82% of those with cirrhosis report experiencing discomfort, and more than half of them believe it lasts for a long time (chronic). Abdominal pain is a common symptom of liver disease.
A stabbing or dull throbbing pain in your right upper abdomen, just below your ribs, may be the result of pain in your liver itself. Swelling from fluid retention and liver and spleen enlargement brought on by cirrhosis can also produce generalized abdominal pain and discomfort.
Cirrhosis can exacerbate the pain from pre-existing diseases, or it can cause discomfort from diseases that are already present. For instance, if you are obese and have non-alcohol-related fatty liver disease, you may also have osteoarthritis, and cirrhosis exacerbates the pain in your bones and joints.
Your entire body goes into an inflammatory state as a result of cirrhosis. General discomfort can be brought on by inflammation and your body’s response to inflammation.

What are the most common causes of Cirrhosis?
Cirrhosis can result from liver damage brought on by a variety of illnesses and situations. Among the causes are:
- Prolonged alcoholism
- Persistent viral hepatitis (hepatitis, B, C, and D).
- Fat builds up in the liver in a condition known as non-alcoholic fatty liver disease.
- An illness called hemochromatosis results in an accumulation of iron in the body.
- The immune system of the body results in a liver illness known as autoimmune hepatitis.
- Biliary duct damage brought on by primary biliary cholangitis.
- Bile duct hardening and scarring brought on by primary sclerosing cholangitis.
- Wilson’s disease is a condition where the liver develops copper buildup.
- Cystic fibrosis
- Lack of alpha-1 antitrypsin.
- Biliary atresia is a disorder marked by abnormally developed bile ducts.
- Long-term heart failure (causes fluid to back up in your liver, swelling in other areas of your body, and other symptoms).
- Rare disorders like amyloidosis, which causes abnormal liver protein deposits called amyloid to interfere with normal liver function, are rare.
Cirrhosis is caused by liver conditions that gradually change the body. When liver cells are damaged, they begin to degenerate and eventually begin to die. Over time, the liver’s injured cells are replaced by scar tissue, impairing its ability to operate.
Anything that damages the liver can lead to Cirrhosis.
How Cirrhosis is diagnosed?

Your doctor will initially inquire about your medical background, including any past usage of prescription and over-the-counter medications. They will also inquire about any herbal remedies or dietary supplements you may be taking.
If you have a lengthy history of alcohol use, injectable drug use, or hepatitis B or C and exhibit the symptoms outlined in this article, your doctor may believe you have cirrhosis.
Your doctor will do a physical examination and might recommend one or more of the following tests to diagnose cirrhosis:
- Physical exam: The red, spider-like blood vessels on your skin, the yellowing of your skin or the whites of your eyes, bruises on your skin, redness on your palms, swelling, tenderness, or pain in your abdomen, and an enlarged, firmer-feeling, bumpy texture to the lower edge of your liver are all signs and symptoms of cirrhosis that your doctor will look for during the examination (the part of your liver below the rib cage that can be felt).

- Blood tests: Your blood will be examined for indications of liver disease if your doctor suspects cirrhosis. Liver injury symptoms include:
- Decreased amounts of albumin and blood clotting elements (lower levels mean your liver has lost its ability to make these proteins).
- Increased liver enzyme levels (suggests inflammation).
- Higher iron content (may indicate hemochromatosis).
- availability of autoantibodies (may indicate autoimmune hepatitis or primary biliary cirrhosis).
- Raised bilirubin level (indicates an inefficient liver function in removing bilirubin from the blood).
- High level of white blood cells (indicates an infection).
- The high amount of creatinine (a sign of kidney disease that suggests late-stage cirrhosis).
- Lower sodium levels (an indicator of cirrhosis).
- Increased alpha-fetoprotein concentration (indicates the presence of liver cancer).
Another blood test will be a viral hepatitis test to check for hepatitis B or C, as well as a complete blood count to detect infections and anemia brought on by internal bleeding.
- Imaging testing: Imaging tests display the liver’s size, shape, and texture. These examinations can also reveal the level of scarring, the amount of fat in your liver, and the quantity of fluid in your belly. You could be given a computerized tomography (CT) scan, an abdominal ultrasound, or a magnetic resonance imaging test to examine your liver (MRI). Your liver’s stiffness and fat content are determined by a specialized ultrasound procedure called transient elastography. An endoscopic retrograde cholangiopancreatography and/or upper endoscopy may be recommended in order to check for bile duct issues as well as varices or bleeding in the oesophagus, stomach, or intestines.
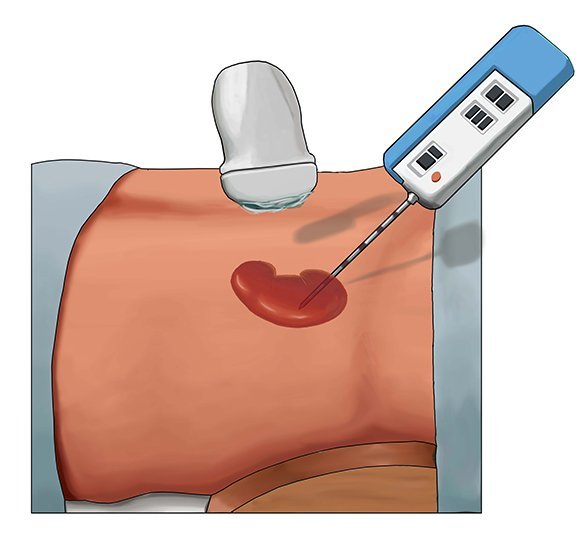
- Biopsy: Your liver is sampled for a biopsy, which is a piece of liver tissue that is taken out and inspected under a microscope. A liver biopsy can identify additional causes of liver damage or enlargement, confirm a cirrhosis diagnosis, or even diagnose liver cancer.
Stages of Cirrhosis:
If you have been told that you have liver cirrhosis, you are already through the initial stages of liver disease. If you have cirrhosis, your liver has scar tissue because it was injured.
In order to forecast outcomes and direct the management of chronic liver disease, liver experts and researchers have created a wide variety of scoring systems. There are also individual score systems for several distinct liver disorders. There is no scoring system if you happen to have more than one liver illness at the same time, and not all liver diseases have one.
For these reasons, it might be simpler to discuss cirrhosis using a classification scheme that your doctor is more likely to use. He or she might use the terms “compensated cirrhosis” or “decompensated cirrhosis” to describe you.
- Compensated Cirrhosis: You have compensated for cirrhosis if you have the disease but don’t yet exhibit any symptoms (you are asymptomatic). It’s possible that your test results and imaging results are normal. Cirrhosis can only be definitively diagnosed by a liver biopsy. Patients with compensated cirrhosis have a nine to twelve-year median survival. (Since the median is the midpoint in a set of statistics, the same amount of people survived for fewer than 9 to 12 years as did so for the entire time period.)
- Decompensated Cirrhosis: Decompensated cirrhosis refers to cirrhosis that has progressed to the point where symptoms are present. Based on your medical history, physical examination, and lab results, your doctor can identify your illness. You have at least one problem, such as liver cancer, variceal haemorrhage, ascites, hepatic encephalopathy, hepatorenal syndrome, or jaundice. Usually, you are taken to the hospital for treatment. Patients with decompensated cirrhosis have a median survival time of about two years.
The liver disease cirrhosis is not cancer. Cirrhosis, however, affects the majority of those with liver cancer. You are more likely to get liver cancer if you have cirrhosis.
If you have been diagnosed with cirrhosis, your liver disease is in its final stages, and any irreparable damage has already been done. Cirrhosis can result from any number of liver conditions and their consequences. It may be possible to delay or stop the progression of your liver illness or complication if it is identified early and successfully treated.
Complications of Liver Cirrhosis:
Cirrhosis of the liver has a lot of side effects. Some of these consequences may be your first observable signs and symptoms of cirrhosis because the illness takes several years to develop.
Portal Hypertension: Most frequently occurring significant consequence is portal hypertension. A rise in your portal vein’s pressure is referred to as portal hypertension (the large blood vessel that carries blood from the digestive organs to the liver). This rise in pressure is brought on by cirrhosis, which blocks blood flow via your liver. Your oesophagus, stomach, or intestines may develop larger veins when blood flow through veins is partially stopped (a condition called varices). These veins can haemorrhage or even break as the pressure inside them increases, resulting in serious internal bleeding.
Additional Complications:
- Edema in your legs, ankles, or feet is another complication of portal hypertension.
- Abdominal fluid accumulation (called ascites).
- Spleen swelling or enlargement (splenomegaly).
- Hepatopulmonary syndrome is the formation and dilatation (expansion) of blood vessels in the lungs, which results in low oxygen levels in the blood and body and shortness of breath.
- Kidney failure is brought on by portal hypertension, which is a side effect of cirrhosis (hepatorenal syndrome). This kind of renal failure exists.
- Confusion, mental problems, behavioural abnormalities, and even coma. When your damaged liver is unable to eliminate toxins from your intestines, they circulate in the circulation and accumulate in your brain (a condition called hepatic encephalopathy).
Hypersplenism: A hyperactive spleen is known as hypersplenism. Blood cells are quickly and prematurely destroyed as a result of this disorder.
Infections: Having cirrhosis makes it more difficult for you to prevent and treat life-threatening infections like bacterial peritonitis (infection of the tissue that lines the inner wall of your abdomen).
Nutritional deficiencies: Your liver breaks down nutrients. This is more challenging with a diseased liver, which also causes weight loss and general weakness.
Liver Cancer: Liver cirrhosis is a common factor in the development of liver cancer.
Liver Failure: Cirrhosis of the liver is one of many diseases and situations that can result in liver failure. Liver failure, as its name suggests, happens when your liver isn’t functioning properly enough to carry out all of its various tasks.
Prevention of Liver Cirrhosis:
Cirrhosis has no known treatment. Your liver is already permanently damaged.
To prevent your cirrhosis from worsening, you might be able to take some steps, depending on the underlying cause of your condition. These actions comprise:
- Issues with food and drink:

Use alcohol sparingly. If you do use alcohol, keep your intake and frequency to a minimum. You run a higher danger if you consume more than two drinks per day if you’re a man or more than one if you’re a woman.
A drink is a 12-ounce can of beer, a glass of wine, or a 1.5-ounce serving of alcoholic beverage. You should never drink alcohol if you have liver illness. Consume a healthy, balanced diet that is low in fat, like the Mediterranean diet. Fruits, vegetables, lean proteins, and whole grains make up a diet that is healthful and well-balanced. Avoid consuming raw seafood, especially clams and oysters. One of the germs that might cause serious sickness may be present in these foods. Cut back on salt.
- Healthy Body Habits
- Maintain a healthy weight with good body habits. Having too much body fat can harm your liver. If you are overweight, request a weight loss plan from your doctor.
- Regular exercise
- For checkups, visit your healthcare practitioner frequently. Obesity, diabetes, hypertension (high blood pressure), high cholesterol (high bad cholesterol [LDL] and/or low good cholesterol [HDL]), and high triglycerides should all be managed according to medical advice.
- If you smoke, stop doing so.
Healthy Liver Habits:
- Avoid engaging in high-risk activities that can result in hepatitis B or C infection, such as sharing needles for illicit drug use or engaging in unprotected sex.
- Get a hepatitis B vaccination. Ask your doctor if drug treatment is acceptable for you if you already have hepatitis.
- Ask your doctor if a pneumonia vaccine is appropriate for you and receive your annual flu shot (people with cirrhosis are more likely to get infections).
- Avoid NSAIDs (non-steroidal anti-inflammatory medicines), large doses of acetaminophen (Tylenol®), ibuprofen (Advil®, Motrin®), indomethacin (Indocin®), celecoxib (Celebrex®), and aspirin. It is safe to use acetaminophen up to 2,000 milligrams per day. These medications may aggravate or affect liver function.
- As directed by your healthcare professional, take all prescribed drugs and attend all scheduled appointments.
Treatment for Liver Cirrhosis:
Treatment depends on what’s causing your cirrhosis and how much damage exists. By treating the underlying cause of early cirrhosis, liver damage might be minimally impacted. The following are the choices:

- Alcoholic dependency treatment. Alcohol consumption should be reduced in those who have cirrhosis brought on by excessive alcohol consumption. Your doctor could suggest a treatment program for alcohol addiction if quitting drinking is challenging. Since any amount of alcohol is damaging to the liver if you have cirrhosis, it is crucial that you stop drinking.
- Lose weight. If they reduce their weight and manage their blood sugar, people with cirrhosis brought on by non-alcoholic fatty liver disease may improve their health.
- Medication to control hepatitis. By treating these viruses specifically, medications may be able to prevent further hepatitis B or C-related harm to liver cells.
- Non-alcohol-linked fatty liver disease: Managing non-alcohol-related fatty liver disease includes decreasing weight, maintaining a nutritious diet, exercising, and adhering to your doctor’s diabetes management recommendations.
- Hereditary Liver Diseases: Treatment for hereditary liver illnesses varies depending on the condition at hand. The goals of treatments include managing consequences and alleviating symptoms. Antibiotics to treat infections, other medications for problems, and medications to minimize swelling in your belly and legs are all possible treatments for alpha-1 antitrypsin insufficiency. Blood removal is used as a treatment for hemochromatosis to lower blood iron levels. Wilson’s disease is treated with medications to eliminate copper from the body and zinc to stop copper absorption. Medication is administered for cystic fibrosis in order to alleviate problems, clear mucus, and enhance lung function. Maintaining the proper level of glucose is the mainstay of treatment for liver-based glycogen storage disorders.
- Autoimmune hepatitis: Treatment includes medications to suppress your immune system.
- Diseases that damage bile ducts: Diseases that affect or clog the liver’s bile ducts can be treated with surgery or drugs like ursodiol (Actigall®) to widen narrowed or blocked ducts.
- Heart failure: The kind and stage of your heart failure will determine your treatment. Medication can be used to lower cholesterol, manage high blood pressure, eliminate extra fluid from the body (edema), and enhance the heart’s ability to pump blood. Other therapies include the implantation of gadgets to assist with blood pumping or monitoring heart rhythm, operations to open blocked arteries, replace or repair heart valves, and heart transplant surgery.
- Medications to treat further cirrhosis causes and symptoms. The progression of some kinds of liver cirrhosis may be slowed by medication. For those with primary biliary cholangitis who receive an early diagnosis, medication may considerably slow the development of cirrhosis.
Naturopathy for Liver Cirrhosis:

The liver is essential for removing harmful toxins from the body and keeping people healthy and active as they are exposed to polluted environments and processed foods on a regular basis.
A naturopathic strategy, however, performs best when utilized with the appropriate regimen and understanding to maintain the liver in peak health. To maintain the liver’s health and gradually detoxify it, try these straightforward naturopathic suggestions:
• A balanced diet: The general health of the liver benefits from a diet high in fruits and vegetables. Fruits and vegetables typically contain large amounts of antioxidants that protect the liver. Because they are high in vitamin B and help with the enzymatic/metabolic activities in the liver, seeds, nuts, whole grains, and legumes are also crucial to include in the diet.
• Herbal remedies: Sometimes a healthy diet is not enough to improve liver function. This is where the value of herbal remedies is relevant. Hepatic herbs including Dandelion root, Milk Thistle, Rosemary, Schisandra, Goldenseal, and Artichoke have a variety of qualities that enhance the liver’s function by enhancing the metabolic processes of detoxification. They also have the ability to repair damaged liver cells. Before ingesting these herbs, speaking with a naturopathic physician is always a good idea.
• Yoga: Yoga is a holistic form of exercise that improves both the body and the mind, even if any sort of exercise is good for your health. The poses Balasana, Salabhasana, Manduka, Adho Mukha Svana, Nauka, and Bhujangasana all stretch, stimulate, and strengthen the liver. The asanas mentioned above can improve the liver’s function and help reduce fat accumulation there.
• Alternative Naturopathic Treatments: To enhance the function of the liver, naturopathic doctors occasionally also utilize natural cures including colon hydrotherapy, enema, mud packs, mud baths, hip packs, heat and cold fomentation, castor oil packs, and stomach packs.
Hydrotherapy: Water is used to flush waste out of the large intestine, a process known as colonic cleansing or irrigation. It helps to lose weight and diagnose hepatic cirrhosis and refractory ascites.
Enema: Patients who are comatose and unable to take the medication by mouth for hepatic encephalopathy due to liver cirrhosis may get it via an enema.
Mud Therapy (Mud Baths, Mud Packs): Mud therapy helps in lowering body temperature. It relieves chronic discomfort and helps with abdominal cramping.
Heat and Cold Fomentation: The local application of heat and cold may be advantageous and relieve the symptoms of liver pain.
Castor Oil Packs: It is for Liver Detoxification. The passage of chemical energy inside the body is encouraged by the important fatty acids, especially the ricinoleic acid found in castor oil, which has a detoxifying impact.
Natural solutions are often the best! It has the ability to address a wide range of issues from their underlying causes without having the negative side effects that many drugs do.
The goals of treatment for cirrhosis of the liver are to:
- Slow further damage to your liver.
- Prevent and treat symptoms.
- Prevent and treat complications.
An Optimal liver function can be encouraged by making a few changes in lifestyle like consuming low-processed, fresh, and clean vegetable-rich diets,

abstaining from alcohol and smoking and leading a physically active life. Naturopathy is a great way to improve renal and liver functions as well as lead an energetic and healthier life.









