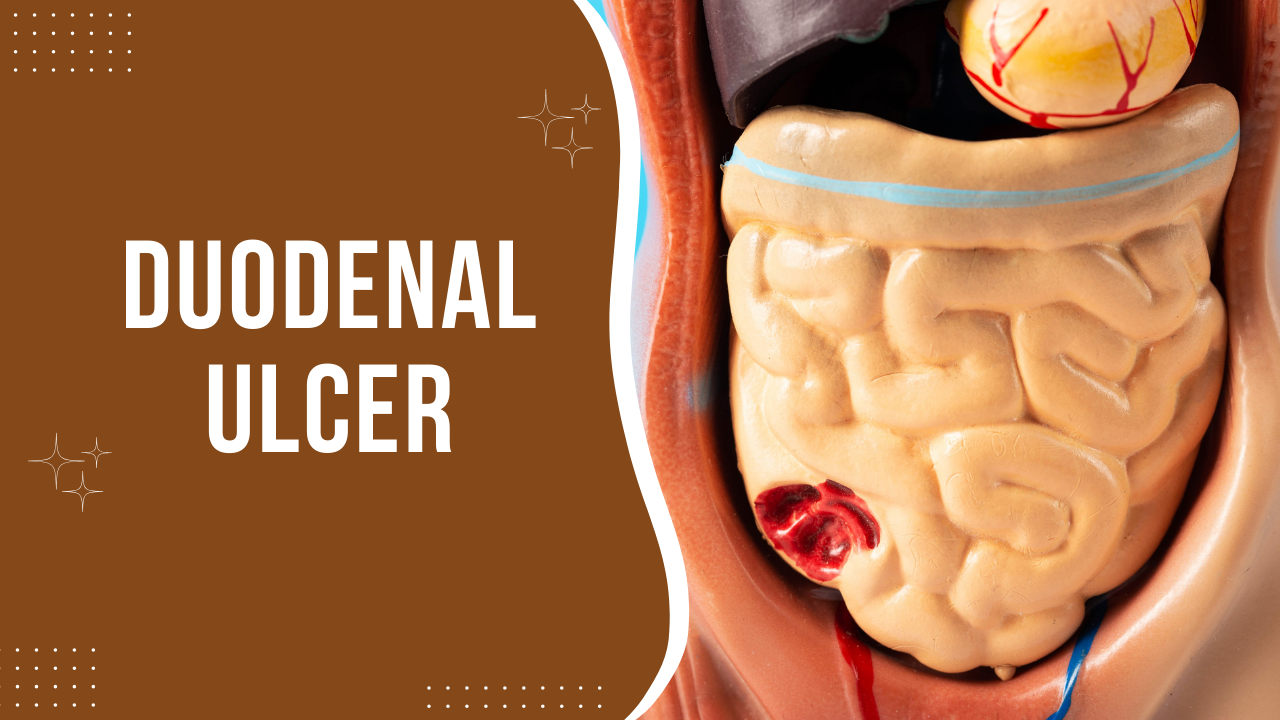
Duodenal Ulcer
Duodenal Ulcer
Ulcers are localized sores or lesions that develop in the lining of various organs, commonly found in the stomach, small intestine, and large intestine. These lesions result from the erosion of the mucous membrane lining, exposing the underlying tissue to digestive juices, primarily hydrochloric acid, in the stomach.
The excessive production of gastric acid, often due to factors such as stress, bacterial infection (Helicobacter pylori), prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), or underlying medical conditions, contributes to the formation of ulcers.
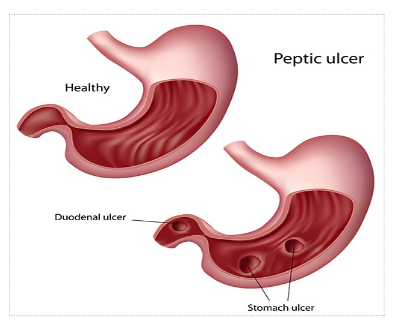
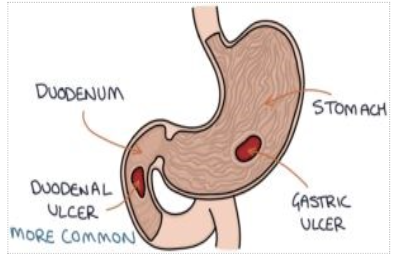
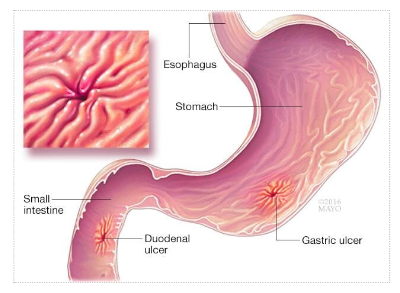
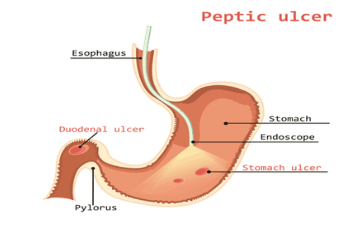
Gastric ulcers and duodenal ulcers are two prevalent types of peptic ulcers. Gastric ulcers develop in the stomach lining, while duodenal ulcers occur in the upper part of the small intestine, known as the duodenum. Both types share common symptoms, including abdominal pain, bloating, nausea, vomiting, and bleeding.
Understanding the pathophysiology of ulcer formation is crucial. The stomach lining typically has a protective layer of mucus that shields it from the corrosive effects of gastric acid. However, when the balance between protective mechanisms and harmful factors is disrupted, erosion occurs, leading to ulceration.
Gastric acid plays a pivotal role in the digestive process, aiding in the breakdown of food particles. However, when its production exceeds normal levels, it can overwhelm the protective mechanisms of the stomach and erode the mucosal lining, leading to ulcer formation.
Treatment strategies for ulcers aim to alleviate symptoms, promote healing, and prevent complications. This often involves a combination of medication, lifestyle modifications, and, in severe cases, surgical intervention.
Medications commonly prescribed for ulcers include proton pump inhibitors (PPIs), which reduce gastric acid production, and antibiotics to eradicate Helicobacter pylori infection if present. Additionally, antacids and cytoprotective agents may be used to neutralize acid and protect the gastric mucosa.
Lifestyle modifications, such as avoiding irritants like spicy foods, alcohol, and NSAIDs, can help reduce the risk of ulcer recurrence. Stress management techniques, dietary changes, and smoking cessation are also recommended.
In severe cases or complications such as perforation, bleeding, or obstruction, surgical intervention may be necessary to repair the ulcer or remove affected tissue.
Ulcers are a common gastrointestinal condition characterized by localized erosion of the mucosal lining, often attributed to factors such as excess gastric acid production, bacterial infection, or medication use. Understanding the underlying causes and implementing appropriate treatment strategies are essential for managing ulcers effectively and preventing complications.
In discussing the management of ulcers, it’s crucial to address prevalent myths and misconceptions surrounding their treatment and dietary considerations. Many individuals believe that once a chronic ulcer develops, they must adhere to a liquid diet indefinitely, viewing the condition as irreversible. However, this notion is rooted in myth rather than medical fact.
Contrary to popular belief, ulcers are not irreparable. With proper treatment and lifestyle adjustments, ulcer healing is attainable. Naturopathic and Ayurvedic approaches offer promising avenues for ulcer management, emphasizing the restoration of balance within the body.
One common myth revolves around dietary restrictions, particularly the misconception that individuals with ulcers must adhere strictly to a liquid diet. However, this restrictive approach is unnecessary and often impractical. Instead, adopting a well-balanced diet that prioritizes alkaline-forming foods can contribute to ulcer healing and symptom management.
The root cause of ulcer formation lies in the disruption of the body’s natural balance, particularly within the gastrointestinal tract. Factors such as increased gastric acid secretion, bacterial infections like Helicobacter pylori, and lifestyle habits can contribute to ulcer development.
Helicobacter pylori, a bacterium found in the stomach, plays a significant role in ulcer pathogenesis. Left untreated, this bacterial infection can compromise the stomach’s protective lining, leading to ulcer formation. Timely intervention to eradicate the infection is crucial in preventing ulcer recurrence and promoting healing.
Maintaining a healthy pH balance within the body is essential for ulcer management. Alkaline-forming foods help neutralize excess acidity, reducing the risk of mucosal damage and ulceration. Additionally, minimizing acidic foods and substances that exacerbate gastric acid production can support ulcer healing.
Addressing common misconceptions surrounding ulcer treatment and dietary management is essential for promoting optimal healing and symptom relief. By debunking myths and implementing evidence-based approaches, individuals can take proactive steps towards ulcer resolution and long-term gastrointestinal health.
Understanding the root causes of ulcer formation, including factors such as gastric acid imbalance and bacterial infections, is crucial for effective management. Through a holistic approach that incorporates dietary modifications, naturopathic interventions, and targeted treatment of underlying infections, individuals can achieve lasting relief from ulcers and promote overall well-being.
Let’s develop deeper into these concepts as we explore the multifaceted nature of ulcer management and the role of diet and natural therapies in promoting healing and symptom relief.
The widespread use of painkillers and certain medications poses a significant risk factor for the development of ulcers. Many individuals’ resort to painkillers to alleviate various symptoms, ranging from headaches to body aches and colds. However, the excessive and indiscriminate use of these medications can lead to adverse health outcomes, including ulceration.
Individuals often develop a habit of relying on painkillers to manage even minor discomforts, contributing to the overuse of these medications. However, it’s crucial to recognize that prolonged and excessive use of painkillers can disrupt the delicate balance within the gastrointestinal tract, ultimately increasing the risk of ulcer formation.
Certain classes of medications, such as blood thinners, commonly prescribed for conditions like high cholesterol or cardiovascular disease, can also contribute to ulcer development. Blood thinners, including medications like aspirin (e.g., Ecosprin), are essential for preventing blood clots and reducing the risk of heart attack or stroke. However, prolonged use of these medications can irritate the stomach lining, leading to ulceration.
Similarly, medications used to manage conditions like osteoarthritis, an autoimmune disorder characterized by joint degeneration, can exacerbate ulcer risk. These medications, often taken over extended periods, may disrupt gastric mucosal integrity and increase gastric acid secretion, further predisposing individuals to ulceration.
Furthermore, lifestyle factors such as smoking and excessive alcohol consumption significantly increase ulcer risk. Research indicates that a substantial proportion of individuals who smoke or engage in heavy alcohol consumption experience acute to chronic ulcers. These habits not only affect liver health and metabolism but also disrupt gastrointestinal function, promoting ulcer formation.
The misuse of painkillers, prolonged use of certain medications, and lifestyle habits such as smoking and excessive alcohol consumption are significant contributors to ulcer development. Understanding these risk factors is essential for implementing preventive measures and promoting gastrointestinal health.
As we continue to delve into the complexities of ulcer management, it’s crucial to address these underlying causes and educate individuals on the importance of mindful medication use and lifestyle modifications in mitigating ulcer risk.
Understanding the anatomical location of ulcers within the stomach is crucial for diagnosis and treatment. By examining the structure of the stomach, we can pinpoint where ulcers typically form.
In visual representations, such as slides or imaging scans, the starting part of the stomach often shows a distinct dark patch indicating the presence of an ulcer. This area, scientifically referred to as the duodenal bulb, is where approximately 90% of ulcers are located, typically within three centimeters of the pylorus. These ulcers are commonly less than or equal to one centimeter in diameter.
The shape and location of ulcers play a key role in diagnosis. Endoscopic examinations or imaging scans provide valuable insights into the size and location of ulcers, aiding doctors in determining the type of ulcer a patient is facing.
Ulcers often exhibit a round shape, with those on the posterior wall tending to be larger than those on the anterior wall. Ulcers located on the anterior wall are around four times more common than gastric ulcers, constituting approximately 80 to 90% of all ulcers.
Individuals between the ages of 30 and 50 are particularly susceptible to duodenal ulcers. Several factors contribute to this increased risk, including the completion of growth periods, high stress levels, and irregular eating habits due to busy lifestyles.
It’s essential to recognize these risk factors and prioritize lifestyle modifications to reduce the likelihood of ulcer development. By adopting healthier eating habits, managing stress levels, and seeking timely medical intervention, individuals can mitigate their risk of duodenal ulcers and maintain gastrointestinal health.
Understanding the nuances of ulcer anatomy and risk factors empowers individuals to take proactive steps towards prevention and management. Through informed decision-making and collaboration with healthcare professionals, individuals can safeguard their digestive well-being and minimize the impact of ulcers on their quality of life.
In the age range between 30 and 50, individuals often find themselves at a critical juncture in life, where they are striving to set the course for their future. Unfortunately, this phase is characterized by a lack of time schedules and punctuality, leading to a disruption in routine and lifestyle. The pursuit of long-term goals amidst the chaos of daily life can result in imbalances, stress, and lifestyle damage, all of which contribute to the development of ulcers.
Conversely, after the age of fifty, individuals may experience a reduction in workload and stress levels, leading to a more relaxed lifestyle. However, this phase is not immune to ulcer development, as years of stress and unhealthy habits may have already taken their toll.
Interestingly, males are more susceptible to ulcers than females, primarily due to their tendency to prioritize career and future security. The pressure to succeed, coupled with a work-oriented mindset, increases stress levels and, consequently, the risk of developing ulcers. While ulcers can occur at any age, males between thirty and fifty years old are particularly vulnerable.
Apart from lifestyle factors, certain behaviors and medical conditions can also increase the risk of ulcer formation. Heavy use of non-steroidal drugs (NSDs) and the indiscriminate consumption of supplements without medical necessity are common culprits. In many cases, individuals habitually self-medicate without proper guidance, leading to an accumulation of foreign substances in the body.
It is crucial to emphasize the importance of adhering to prescribed medication regimens and avoiding unnecessary supplementation. Failure to do so can result in toxicity within the body, leading to various health complications, including ulcer formation.
Additionally, certain medical conditions, such as Helicobacter pylori infection, Zollinger-Ellison syndrome, vascular insufficiency, and a history of malignancy, can predispose individuals to ulcers. Chemotherapy, while an essential treatment for malignancies, can also contribute to ulcer development due to its damaging effects on healthy cells and bodily functions.
Individuals experiencing symptoms or facing these risk factors should seek medical attention promptly. Early intervention and lifestyle modifications can help prevent ulcer formation and mitigate its impact on overall health and well-being.
By understanding the various risk factors associated with ulcer development and adopting proactive measures to address them, individuals can safeguard their gastrointestinal health and maintain a high quality of life.
Individuals at high risk factors are prone to developing ulcers, particularly between the ages of 30 and 50. Identifying the clinical features or symptoms associated with ulcer development is crucial for timely intervention and management.
Initially, ulcer symptoms may go unnoticed or be disregarded, leading to delayed diagnosis. Often, individuals only become aware of the ulcer after significant damage has occurred, typically around 50% of the damage being done. Therefore, it is essential to pay attention to any abnormal signs or symptoms and seek medical evaluation promptly.
The most common symptom of an ulcer is epigastric burning or itching pain below the abdomen, specifically on the left side. This discomfort may manifest as continuous pinching pain, exacerbated by food consumption or certain movements. Additionally, individuals may experience a sensation of heat or congestion in the neckline or chest area.
One characteristic feature of ulcers is that pain tends to improve after meals initially. However, as digestion progresses and gastric juices mix with food, the pain may return, often within two to three hours after eating. This pattern of pain relief followed by recurrence is a typical indicator of duodenal ulcers.
Radiating pain, particularly towards the back, is another common symptom associated with duodenal ulcers. This type of pain distinguishes duodenal ulcers from gastric ulcers, as radiating pain is not typically observed in the latter.
Unexpected weight gain may also be a symptom of ulcer development, resulting from frequent eating to alleviate pain. Continuous snacking to manage discomfort can lead to excess calorie intake and subsequent weight gain.
Fortunately, the majority of duodenal ulcers do not progress to complications such as hemorrhage or malignancy. While wound healing may take time and can present challenges, most cases are non-cancerous.
In the rare instance of bleeding, it may manifest as melena, with approximately a 10% chance of occurrence after the onset of ulcer bleeding.
Recognizing the clinical features associated with ulcers is critical for early detection and management. Timely intervention can prevent complications and ensure optimal outcomes for individuals at risk.
When experiencing persistent symptoms for more than 20 to 30 days, particularly if they disrupt sleep or daily activities, it’s essential to seek medical attention promptly. Difficulty sleeping due to discomfort, especially after meals, can indicate an underlying health issue such as an ulcer. The vicious cycle of disrupted sleep and aggravated symptoms can significantly impact one’s quality of life and exacerbate the ulcer condition.
If persistent symptoms are observed, it’s crucial to consult a healthcare professional for further evaluation. Various diagnostic tests may be recommended based on the individual’s symptoms and stage of the condition. These tests aim to accurately diagnose the problem to initiate appropriate treatment.
Common diagnostic tests include barium X-rays, which involve ingesting a liquid containing barium to highlight specific areas in X-ray imaging. Additionally, breath tests may be conducted to detect infections like Helicobacter pylori, a bacterium associated with ulcers. Blood tests and stool tests may further confirm the presence of specific infections.
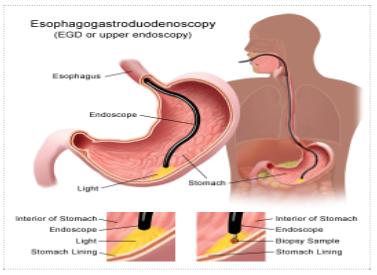
Endoscopy is another common diagnostic procedure wherein a flexible tube with a camera is inserted through the mouth to examine the digestive tract. This procedure allows for visualization of the ulcer site, assessment of bleeding, and even minor interventions to manage bleeding or other complications.
Once diagnosed, treatment approaches vary depending on the severity and cause of the ulcer. In cases of Helicobacter pylori infection or significant damage, medication such as proton pump inhibitors and antacids may be prescribed to reduce stomach acid levels and alleviate symptoms.
Coating agents like sucralfate may also be used to protect the ulcer site and promote healing. In instances of bleeding ulcers, interventions during endoscopy may help manage bleeding and promote healing.
While natural remedies and lifestyle modifications may complement medical treatment, they may not suffice for severe cases or infections requiring specific medications. Therefore, it’s essential to follow the guidance of healthcare professionals to effectively manage ulcers and prevent complications.
Persistent symptoms suggestive of ulcers warrant thorough evaluation and medical intervention. Prompt diagnosis and appropriate treatment can alleviate symptoms, promote healing, and improve overall well-being for individuals affected by ulcers.
In the treatment of ulcers, drying out the affected area is often the initial step to promote healing. Protein agents play a crucial role in this process and are commonly used in allopathic treatments. Medications such as omeprazole and ranitidine are frequently prescribed to reduce acid levels and alleviate symptoms. Additionally, antibiotics may be necessary to treat infections, particularly Helicobacter pylori, which is associated with ulcers. Combinations of antibiotics like clarithromycin and amoxicillin are often used to combat such infections.
While these medications are commonly used in allopathic treatments, it’s essential for healthcare providers to thoroughly review prescriptions and ensure proper administration. In some regions, patients may obtain medications easily from pharmacists, but self-medication without professional guidance can lead to complications.
Complications of ulcers can be severe and life-threatening. Blood vomiting, perforation of the ulcer, or ulcer rupture are critical emergencies requiring immediate medical attention. Gastric outlet obstruction, characterized by narrowing of the stomach’s passage, is another common complication that necessitates prompt intervention to prevent further complications.
In managing ulcers, prevention is often emphasized as the best approach. Dietary modifications play a crucial role, with food acting as a powerful tool in healing and preventing ulcers. However, dietary recommendations should consider factors such as regional availability and individual tolerances. Regular monitoring of dietary changes and their effects on the patient’s symptoms is essential to ensure efficacy and minimize adverse reactions.
Ultimately, in the treatment of ulcers, a comprehensive approach that integrates medical interventions with dietary adjustments is crucial for optimal outcomes. Healthcare providers must prioritize patient safety and well-being by closely monitoring symptoms, administering appropriate medications, and guiding dietary modifications to promote healing and prevent complications.
When it comes to managing ulcers, understanding which foods to include and avoid is essential. Here, we outline the dos and don’ts of dietary choices to aid in ulcer management.
Good Foods: –
- Probiotics: Incorporating probiotics containing beneficial bacteria can be beneficial for ulcer patients. Homemade GERD or buttermilk, prepared without preservatives, is a great option. It’s crucial to ensure freshness by preparing it the night before consumption.
.

2. Fiber-Rich Foods: A diet rich in fiber can aid in digestion and promote healing of stomach ulcers. Whole grains such as dalia, barley, oats, and millets are excellent choices. Avoid processed bakery items and opt for whole grains instead.
3. Fresh Fruits and Vegetables: Fresh fruits and vegetables are rich in fiber and alkaline properties, which can help soothe and heal ulcers. Incorporate a variety of seasonal fruits and vegetables into the diet to benefit from their healing properties. Foods rich in vitamin A, such as sweet potatoes, carrots, and spinach, are particularly beneficial for ulcer healing.
4.Citrus Fruits: Despite their acidic nature, citrus fruits like lemon can be beneficial for ulcer patients. They can be included in salads or consumed in their natural form to aid in healing.
Foods to Avoid for Ulcer Healing: –
When managing ulcers, certain dietary choices can exacerbate symptoms and hinder the healing process. Here are some foods to avoid:
- Milk: Regardless of whether it’s cow or buffalo milk, dairy should be avoided due to its potential to disrupt digestion and exacerbate ulcer symptoms.
- Fatty and Fried Foods: Spicy, fatty, and oily foods can aggravate ulcer symptoms and should be eliminated from the diet.
- Alcohol and Tobacco: Alcohol and tobacco consumption can delay ulcer healing and should be stopped to promote natural wound recovery.
- Strong Coffee and Tea: Caffeinated beverages like coffee and tea can increase acid reflux, further irritating ulcerated regions. Avoiding these beverages can help in ulcer management.
Natural Remedies for Ulcer Healing: –
In addition to dietary modifications, incorporating natural remedies can aid in ulcer healing. Here are some effective options:
- Fresh Coriander and Fennel Juice: Rich in alkaline properties, Hawaiian coriander and fennel juice can help soothe ulcers and aid in digestion. Consuming 100 ml of this juice on an empty stomach or after meals can promote healing.
- Ash Gourd Juice: Known for its cooling properties, ash gourd juice can alleviate acidity and promote ulcer healing. Consuming 200 ml of fresh ash gourd juice daily can help in ulcer management.
- Sugarcane Juice and Lemon Water: Sugarcane juice, rich in nutrients, can serve as an effective remedy for ulcers. If sugarcane juice is unavailable, lemon water can be a suitable alternative. Consuming 200 ml of either juice daily can aid in ulcer healing.
- Fenugreek Seeds (Methi) or Soft Coconut Flesh: Fenugreek seeds are rich in alkaline properties and possess antibacterial and anti-inflammatory benefits. Soaking one tablespoon of fenugreek seeds overnight in 100 ml of water and consuming the strained water in the morning can aid in ulcer management. Additionally, coconut water is a natural remedy that can promote ulcer healing, though it should be avoided if bloating or reflux occurs after consumption.
Incorporating these natural remedies into your routine, alongside dietary changes, can help in the management and healing of stomach ulcers. It’s important to consult with a healthcare professional before making significant changes to your diet or lifestyle.
Naturopathic Treatments for Ulcer Healing
Ulcers can be a challenging condition to manage, but natural remedies and therapies can play a significant role in promoting healing and relieving symptoms. Let’s explore some effective naturopathic treatments for ulcers:
- Mud Therapy:

Mud therapy, particularly using deep sea black mud, has shown promise in ulcer healing. Applying this mud to the stomach for 30 to 60 days, for at least 30 minutes daily, can help soothe ulcers and promote healing. Ensure the mud has a paste-like consistency before application.
- Cold Packs and Sun Bathing:
Cold packs applied to the stomach for 30 minutes can provide relief and aid in ulcer management. Additionally, exposure to sunlight for 10 to 15 minutes during the early morning hours can improve metabolism, boost immunity, and enhance overall well-being. Sunbathing also helps increase vitamin D levels, which is beneficial for ulcer healing.
- Herbal Remedies:
Several herbs have therapeutic properties that can support ulcer healing. Consider incorporating the following into your treatment plan:
- Coriander and Fennel Juice: Rich in alkaline properties, Hawaiian coriander and fennel juice can soothe ulcers and aid digestion. Consuming 100 ml of this juice daily, preferably on an empty stomach, can be beneficial.
- Ash Gourd Juice: Known for its cooling properties, ash gourd juice can alleviate acidity and promote ulcer healing. Consuming 200 ml of fresh ash gourd juice daily can provide relief.
- Sugarcane Juice and Lemon Water: Sugarcane juice and lemon water, consumed in quantities of 200 ml per day, can help in ulcer management. These beverages provide essential nutrients and promote healing.
- Fenugreek Seeds: Soaking one tablespoon of fenugreek seeds overnight in 100 ml of water and consuming the strained water in the morning can aid in ulcer management.
- Coconut Water: Coconut water is a natural remedy that can promote ulcer healing. However, it should be avoided if bloating or reflux occurs after consumption.
- Wheat Grass Juice and Neem Leaves:
Fresh wheat grass juice is highly beneficial for ulcer healing and can be consumed in quantities of 100 ml per day. Alternatively, wheat grass powder or tablets can be used as supplements. Neem leaves, when consumed regularly for 30 to 60 days, can also alleviate ulcer symptoms and promote healing.
- Aloe Vera:
Fresh aloe vera juice, if available, can provide relief from ulcer symptoms. Consuming aloe vera juice daily for 30 to 60 days can aid in ulcer healing and symptom relief.
Incorporating these naturopathic treatments into your ulcer management plan can complement conventional therapies and promote natural healing. However, it’s essential to consult with a healthcare professional before starting any new treatment regimen.
Alongside these remedies, it’s vital to ensure open communication with your healthcare provider and stay informed about the latest developments in ulcer treatment. Remember to prioritize your health and well-being as you navigate your healing journey.
In conclusion, naturopathic treatments offer promising avenues for ulcer healing and symptom management. From mud therapy to herbal remedies like coriander and fennel juice, there are numerous natural options available to support healing and alleviate discomfort.
However, it’s crucial to approach these remedies with caution and consult with a healthcare professional before incorporating them into your treatment plan. By combining natural remedies with conventional therapies and maintaining open communication with your healthcare provider, you can optimize your ulcer healing journey.
Remember, healing takes time, patience, and a holistic approach. By prioritizing your health, adopting healthy lifestyle habits, and exploring natural remedies, you can empower yourself on the path to ulcer recovery.
Stay informed, stay proactive, and above all, prioritize your well-being as you embark on your journey to optimal health.