Parkinsonism/Parkinson’s Disease
Parkinsonism/Parkinson’sDisease
Parkinson’s disease in Ayurveda: Understanding the Vata Perspective
Parkinson’s disease, a neurological disorder affecting movement, is viewed through an Ayurvedic lens as a Vata-aggravated disease. Ayurveda, an ancient Indian system of medicine, recognizes three doshas—Vata, Pitta, and Kapha—as the fundamental energies that govern physiological functions. Any imbalance in these doshas is believed to lead to disease.
In Parkinson’s, the aggravation of Vata dosha plays a significant role. This condition is characterized by symptoms such as tremors, stiffness, and impaired balance. While modern science has yet to pinpoint the exact cause, a combination of genetic and environmental factors is suspected.
Ayurvedic treatment for Parkinson’s focuses on balancing Vata dosha. This approach includes dietary modifications, lifestyle adjustments, herbal remedies, and specific therapies. Warm, cooked foods that are easy to digest are recommended, while cold, dry, and processed foods should be avoided. Herbs like Ashwagandha, Brahmi, and Guggulu are used to support the nervous system and balance the doshas.
Ayurvedic therapies such as Abhyanga (oil massage), Shirodhara (pouring warm oil on the forehead), and Panchakarma (detoxification therapies) are also employed to restore balance and promote overall health.
Ayurveda offers a holistic approach to Parkinson’s disease by addressing the root cause through dosha balancing. By integrating these principles, Ayurveda aims to improve the quality of life for individuals living with Parkinson’s.
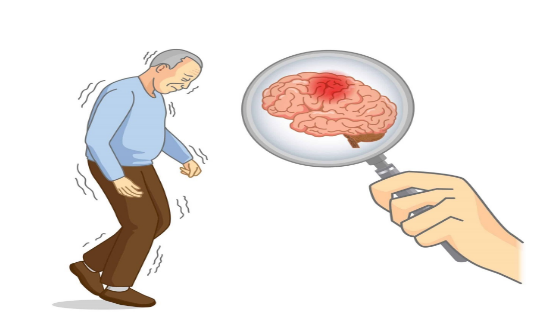
Understanding Parkinson’s disease: A Neurological Perspective
Parkinson’s disease is a chronic, progressive neurological disorder that affects the brain and the nervous system. It disrupts the normal functioning of neurotransmitters in the brain, which are responsible for controlling our body’s movements and senses.
This disease is characterized by its impact on muscle control, mood, and balance. Individuals with Parkinson’s often experience tremors, stiffness, and difficulty with balance and coordination. As the disease progresses, these symptoms can worsen, leading to significant challenges in daily life.
Early intervention and proper treatment can help manage Parkinson’s disease effectively. With appropriate care, the symptoms can be controlled, and the progression of the disease can be slowed down. However, if left untreated, Parkinson’s can become increasingly severe, affecting a person’s ability to perform even basic tasks.
In conclusion, Parkinson’s disease is a complex neurological disorder that requires comprehensive care and management. By understanding its nature and symptoms, we can better support individuals living with Parkinson’s and improve their quality of life.
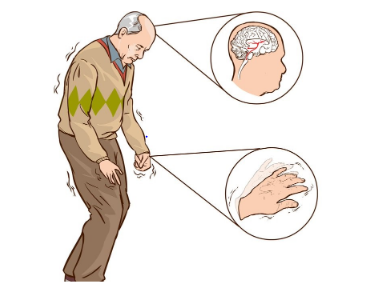
Characteristics of Parkinson’s disease:
Parkinson’s disease is characterized by several key symptoms, including muscle rigidity, tremors, and bradykinesia (slowness of movement). These symptoms significantly impact a person’s motor function and can affect their ability to perform daily activities.
Muscle Rigidity: This refers to the stiffness and tightness of muscles, which can make movement difficult and uncomfortable. It often affects the arms, legs, and neck.

Tremors: Tremors are involuntary shaking movements that commonly occur in the hands, arms, legs, jaw, or head. These tremors can be subtle or pronounced and may worsen with stress or excitement.
Bradykinesia: Bradykinesia is a slowness of movement, making simple tasks like walking or getting up from a chair challenging. Movements may become hesitant and require more effort than usual.
These symptoms can vary in severity and progression from person to person. Early detection and management of Parkinson’s disease are crucial in improving quality of life and slowing the progression of the disease.
Causes of Parkinson’s disease:
Parkinson’s disease is a complex condition with various factors contributing to its development. Understanding these causes is crucial for effective management and prevention strategies. Here are the key factors associated with Parkinson’s:
- Decreased Dopamine Levels: Parkinson’s is often characterized by a decrease in dopamine, a neurotransmitter responsible for regulating mood, happiness, and movement. This reduction in dopamine levels can lead to the motor symptoms associated with Parkinson’s.
- Family History: Individuals with a family history of Parkinson’s are at a higher risk of developing the disease. While genetic factors play a role, environmental factors may also contribute.
- Viral Infections: Certain viral infections have been linked to an increased risk of Parkinson’s disease. These infections can cause inflammation in the brain, potentially triggering the development of Parkinson’s.
- Anti-psychotic Drugs: Long-term use of certain anti-psychotic medications can increase the risk of developing Parkinson’s disease. These drugs may alter dopamine levels in the brain, leading to neurological changes over time.
- Genetic Factors: While specific genetic factors contributing to Parkinson’s are still being researched, certain genes have been associated with an increased risk of developing the disease. These genetic factors may manifest at any age, including childhood or later in life.
6. Head Trauma: Traumatic brain injuries, such as those resulting from accidents or sports injuries, can damage neurons in the brain. This damage may contribute to the development of Parkinson’s disease later in life.
7. Environmental Factors: Exposure to certain environmental factors, such as pesticides or certain metals, has been linked to an increased risk of Parkinson’s disease. Individuals working in industries or environments with high pesticide or metal exposure may be at a higher risk.
Understanding these causes can help individuals take preventive measures and adopt healthier lifestyles to reduce their risk of developing Parkinson’s disease. Regular exercise, a balanced diet, and avoiding exposure to harmful substances are important steps in maintaining brain health and overall well-being.
Symptoms of Parkinson’s disease:
Parkinson’s disease is characterized by a range of symptoms that can affect various aspects of a person’s physical and mental health. Here are some common symptoms associated with Parkinson’s:
- Muscle Rigidity: Stiffness or inflexibility in the muscles, which can affect movement and posture.

2. Tremors: Involuntary shaking or trembling, usually starting in the hands or fingers.
3. Bradykinesia: Slowness of movement, making simple tasks more difficult and time-consuming.
4. Postural Instability: Difficulty maintaining balance and coordination, leading to an increased risk of falls.
5. Changes in Posture: A stooped or hunched-over posture, often with a tendency to lean forward.
6. Freezing: A sudden, temporary inability to move, often occurring when starting to walk.
7. Micrographia: Small, cramped handwriting that becomes difficult to read.
8. Masked Face: A reduced range of facial expressions, giving the face a fixed or mask-like appearance.
9. Speech Changes: Soft, slurred, or monotone speech, often with a hesitant or stuttering quality.
10. Swallowing Difficulties: Trouble swallowing food or liquids, which can lead to choking or aspiration pneumonia.
11. Drooling: Increased saliva production and difficulty swallowing, leading to drooling.
12. Sleep Disturbances: Difficulty falling asleep or staying asleep, often due to physical discomfort or medication side effects.
13. Constipation: Slowed digestion and reduced bowel movements, leading to difficulty passing stools.
14. Depression and Anxiety: Feelings of sadness, hopelessness, or worry, which can be exacerbated by the challenges of living with Parkinson’s.
15. Cognitive Changes: Problems with memory, attention, and executive function, which can affect daily tasks and decision-making.
16. Dementia: In later stages of the disease, some individuals may develop dementia, characterized by severe memory loss and cognitive decline.
17. Sexual Dysfunction: Erectile dysfunction or other sexual problems may occur in men with Parkinson’s disease.
It’s important to note that not everyone with Parkinson’s will experience all of these symptoms, and the severity and progression of symptoms can vary widely among individuals. Treatment and management strategies, including medications, therapy, and lifestyle changes, can help alleviate symptoms and improve quality of life for people with Parkinson’s disease.
Forms and types of Parkinson’s disease:
Top of Form
Parkinson’s disease manifests in various symptoms and can be classified into different types and forms. Here’s a summary of what you shared:
- Tremor Dominant Parkinson’s Disease: This is the most common form, affecting around 75% of people with Parkinson’s. It typically occurs between the ages of 45 to 55. Symptoms include tremors in hands, legs, chin, and jaw, as well as problems with balance, speech, and a shuffling gait.
- Partial Instability Gait Difficulty: Partial instability and gait difficulty are common in Parkinson’s disease. This can manifest as a shuffling gait, difficulty balancing, and a tendency to fall, which can progress rapidly. Gait difficulty refers to the way a person stands and moves, affecting their posture and overall movement.
- Juvenile Parkinson’s disease: This form occurs during childhood.
- Young Onset Parkinson’s Disease: This form generally occurs between the ages of 20 to 35.
- Late Onset Parkinson’s Disease: This is the most common form in individuals over 60 years old, occurring after the onset of tremors.
It’s crucial to diagnose the specific type and form of Parkinson’s disease to tailor treatment effectively. Early detection can sometimes lead to better outcomes in managing the disease.
Parkinson’s disease: Diagnosis and Clinical Tests
Diagnosing Parkinson’s disease involves a series of clinical tests and evaluations to understand the patient’s symptoms, medical history, and physical condition. While there is no definitive test for Parkinson’s disease, a combination of tests and assessments helps in reaching a diagnosis.
- Family History: Doctors often inquire about the patient’s family history to identify any genetic predisposition to Parkinson’s disease. A positive family history can be an important indicator for diagnosis and treatment planning.
- Physical Examination: A thorough physical examination is crucial for assessing motor symptoms associated with Parkinson’s disease. Doctors look for signs such as tremors, stiffness, bradykinesia (slowed movement), and postural instability. These symptoms, especially tremors and their characteristics (resting or action tremors), help in diagnosing Parkinson’s disease.
- Neurological Examinations: Neurological assessments are conducted to evaluate the patient’s mental status, memory, and overall brain function. These examinations help in understanding the extent of neurological damage caused by Parkinson’s disease.
- Imaging Tests: Imaging tests like CT scans and MRI scans provide detailed images of the brain, allowing doctors to identify any abnormalities or changes associated with Parkinson’s disease. These tests help in ruling out other conditions with similar symptoms and confirming a Parkinson’s diagnosis.
- CSF Culture Tests: Cerebrospinal fluid (CSF) culture tests may be performed in certain cases where other tests are inconclusive. These tests help in identifying any viral infections or other factors that may be contributing to the development of Parkinson’s disease.
- Other Clinical Tests: Additional clinical tests, such as blood tests, may be conducted to rule out other conditions and to assess overall health status.
Overall, a comprehensive approach involving a combination of clinical tests and evaluations is essential for diagnosing Parkinson’s disease. Early diagnosis allows for timely intervention and management of symptoms, improving the quality of life for individuals affected by this condition.
After a diagnosis of Parkinson’s disease, the treatment approach aims to improve the patient’s quality of life and manage their symptoms, as there is no specific cure for the condition. Here are some ways in which patients can receive help:
- Improving Quality of Life: The primary goal of treatment is to enhance the patient’s quality of life. This includes managing symptoms such as depression, anxiety, and stress through counselling and alternative therapies.
- Symptom Management: Naturopathy and other alternative therapies can help manage symptoms such as tremors, stiffness, and bradycinesia. These therapies focus on improving circulation, managing neurological disorders, and enhancing mood through hormone-balancing foods.

3. Counselling: Patients may benefit from counselling to address psychosomatic issues associated with Parkinson’s disease. Counselling can help patients express their feelings and concerns openly, leading to improved mental well-being.
4. Alternative Therapies: Naturopathy and other alternative therapies can complement traditional treatments, helping to minimize side effects of medications and improve overall health.
5. Medication Management: While medications are often necessary to manage Parkinson’s symptoms, alternative therapies can help reduce the dosage over time, minimizing side effects and improving overall health.
6. Herbal Supplements: Certain natural herbs and supplements may help minimize side effects and manage symptoms. However, it’s essential to consult with a healthcare provider before starting any herbal supplements to ensure they are safe and effective for individual use.
By focusing on improving quality of life, managing symptoms, and minimizing side effects, patients with Parkinson’s disease can lead a more comfortable and fulfilling life.
In the management of Parkinson’s disease, several medications are commonly prescribed. These medications aim to alleviate symptoms and improve the patient’s quality of life. It’s important to note that only healthcare professionals are qualified to prescribe these medications. Here are some common medications used in the treatment of Parkinson’s disease:
- Levodopa and Carbidopa: These are among the most commonly prescribed medications for Parkinson’s disease, especially in the early stages. Levodopa is converted into dopamine in the brain, helping to replenish the reduced levels of dopamine responsible for Parkinson’s symptoms. Carbidopa is often combined with levodopa to enhance its effectiveness and reduce side effects.
- Dopamine Agonists: These medications mimic the effects of dopamine in the brain. They are often prescribed when levodopa alone is not sufficient or to delay the need for levodopa. Examples include Bromocriptine Mesylate.
- Anticholinergic Drugs: These medications can help control tremors and muscle stiffness by blocking the action of acetylcholine, a neurotransmitter in the brain. Benzotropine is an example of an anticholinergic drug used in Parkinson’s disease.
- Antiviral Drugs: In cases where Parkinson’s disease is believed to be triggered by a viral infection, antiviral medications may be prescribed. However, the role of antiviral drugs in treating Parkinson’s disease is still under research and not widely used.
- Physiotherapy: While not a medication, physiotherapy plays a crucial role in managing Parkinson’s disease. It can help improve mobility, balance, and muscle strength, as well as reduce the risk of falls.
It’s important for patients to work closely with their healthcare providers to develop a treatment plan that suits their individual needs and to monitor for any side effects or interactions with other medications.
Exercise plays a crucial role in managing Parkinson’s disease, often complementing medication. Here’s a summary of the key points regarding exercise in Parkinson’s disease:

- Significance of Exercise: Exercise is essential in managing Parkinson’s disease, with 60 to 70% of improvement attributed to it. While medications help suppress tremors and manage symptoms, exercise helps improve and manage symptoms effectively.
- Types of Recommended Exercises: Various types of exercises are recommended for Parkinson’s disease, including aerobic fitness, strength training, stretching, and agility exercises. These exercises should be performed for a minimum of 30 minutes daily.
- Changing Exercises: It’s important to change exercises regularly to prevent muscle rigidity and to ensure that patients don’t become accustomed to specific movements. Every day, a different set of exercises should be practiced.
- Age Consideration: Exercise routines should be tailored according to the age of the patient. Younger patients may be able to perform more intense exercises compared to older patients. Agility exercises should be selected based on the individual’s age and physical condition to minimize the risk of injuries.
- Gradual Progression: Exercise routines should be gradually increased based on the patient’s progress and response. The duration and intensity of exercises can be increased gradually to improve the effectiveness of the exercise regimen.
- Risk Factors: Care should be taken to avoid exercises that may increase the risk of injuries, especially in older patients. For example, suggesting high-intensity aerobic fitness exercises to patients over 60 may increase the risk of bone brittleness and muscular dystrophies.
- Consultation and Monitoring: It’s important for patients to consult with healthcare professionals before starting any exercise regimen. Healthcare providers can recommend suitable exercises based on the patient’s condition and monitor their progress to ensure safety and effectiveness.
Exercise is crucial in Parkinson’s disease as it can repair the damaged dopamine system or prevent further damage. Here are the key points regarding the importance of exercise in managing Parkinson’s:
- Repair and Prevention: Exercise can repair the damaged dopamine system, which is responsible for muscle movements. It can also prevent the progression of Parkinson’s by balancing dopamine levels.
- Severity of Symptoms: Regular exercise can help prevent the symptoms of Parkinson’s disease from becoming as severe as they might be without exercise.
- Positive Outlook: Exercise helps patients maintain a positive outlook. Group exercises, where patients can interact with others facing similar challenges, can be particularly beneficial as they provide a sense of community and positive reinforcement.
- Physical and Mental Health: Exercise not only benefits physical health but also mental health. It can help reduce depression and anxiety commonly associated with Parkinson’s disease.
- Progress and Benefits: While the progress and benefits of exercise may vary from person to person, regular exercise can lead to noticeable improvements in symptoms and overall well-being.
- Professional Guidance: It’s important for patients to consult with healthcare professionals before starting an exercise regimen to ensure it is safe and appropriate for their condition.
In summary, exercise is a powerful tool in managing Parkinson’s disease, offering physical, mental, and emotional benefits that can significantly improve quality of life for patients.
Yoga can be incredibly beneficial for Parkinson’s disease patients, helping to manage symptoms and improve overall well-being. Here’s how yoga can help:
- Reducing Shaking: Yoga poses and practices can help divert the patient’s attention, reducing the severity of shaking. By engaging in activities that require focus, such as talking or participating in activities, patients can experience a decrease in shaking.
- Facial Expression: Specific yoga poses, like the Lion Pose, can help improve facial expressions and reduce tremors around the jawline and face.

3. Eye Exercises: Yoga includes eye exercises that can help reduce rigidity in the facial and eye muscles. Practices like focusing on a point without blinking or moving the eyeballs right and left can help relax these muscles.
4. Breathing Exercises: Rhythm exercises in yoga, such as Anulom Vilom (alternate nostril breathing) and Savasana (Corpse Pose), can help activate different energy channels and relax the mind and body. These practices can directly affect the brain and improve overall well-being.
5. Muscle Stretching: While yoga does not involve intense stretching, it can help improve muscle flexibility and reduce muscle rigidity, common symptoms of Parkinson’s disease.
6. Personal Attention: It’s important for patients to receive personal attention when practicing yoga, as not all movements may be possible initially. Gradual progress can be made with effort and practice.
Yoga offers a holistic approach to managing Parkinson’s disease, focusing on both physical and mental well-being. It can be tailored to suit the individual needs of each patient, making it a valuable addition to their treatment plan.
It’s important to tailor yoga exercises to the individual’s capabilities and needs, especially for patients with Parkinson’s disease. Here’s a summary of the recommended yoga poses:
- Tadasana (Mountain Pose): This pose is helpful for improving posture imbalance. It involves standing tall with feet together, aligning the body from head to toe.
- Ekapadasana (One-Legged Pose): This pose can also help with posture imbalance. It involves balancing on one leg while the other is raised behind, holding onto a support if needed.
- Forward and Backward Bending: These movements can help improve flexibility and range of motion. They include forward bends (Hastapadasana), backward bends (Bhujangasana), and lateral bends (Konasana).
- Parvatasana (Mountain Pose): This pose involves stretching the arms overhead while standing or seated, helping to improve posture and stretch the spine.
- Sarvangasana (Shoulder Stand): This pose can improve circulation and reduce stiffness in the neck and shoulders.
- Vakrasana (Twisted Pose): This pose involves twisting the spine while sitting or standing, which can improve spinal mobility and digestion.
- Bhujangasana (Cobra Pose): This pose can help strengthen the back muscles and improve posture.
- Konasana (Angle Pose): This seated pose helps stretch the inner thighs and groin area, promoting flexibility.
It’s important to start with gentle movements and gradually increase intensity and duration as tolerated. Each person’s ability to perform these poses will vary, so it’s essential to listen to the body and not push beyond comfortable limits. Providing support, such as using props or assistance from a caregiver, can help ensure safety and proper alignment.
It’s essential to consider dietary recommendations for patients with Parkinson’s disease, focusing on omega-rich foods, specific fruits, vegetables, and alternative grains like millets. Here’s a summary:
- Omega-Rich Foods: Include flax seeds, walnuts, almonds, pumpkin seeds, tuna, and salmon in the diet. These foods are rich in omega fatty acids, which are beneficial for brain health.
- Fruits: Mangoes are rich in vitamin B, which supports memory neurons. Pineapples help in serotonin secretion. Other fruits like grapes and seeds are also beneficial.
- Vegetables: Carrots, beetroot, cabbage, and capsicum are recommended for their rich nutrient content and fiber, which can help with constipation.
- Grains: Instead of wheat or rice, consider oats, ragi, and millets. Millets like proso, barnyard, little, kodo, and foxtail millets are easy to digest and nutritious.
- Amino Acid Rich Foods: Include Brazil nuts, sesame seeds, lentils, and chickpeas, which are rich in phenylalanine, an essential amino acid for brain health.
- Calcium-Rich Foods: Broccoli, spinach, and alfalfa are good sources of calcium. Alfalfa can be consumed as sprouts, juice, powder, or tablets.
It’s important to incorporate these foods into the diet regularly and in appropriate quantities based on individual health conditions and dietary preferences.
Naturopathy offers several treatments that can help manage Parkinson’s disease symptoms. Here’s a summary of the key points:
- Massage Therapy: Massage is considered one of the best and essential therapies for Parkinson’s disease. It can be done on specific body parts or the entire body. Regular massage can be beneficial for patients of all ages, regardless of other health conditions or medical history.
- Enema: Enemas, particularly warm water with lemon, can be used to relieve constipation, a common issue in Parkinson’s patients.
- Sun Bath: Sunbathing can help increase vitamin D levels, which is beneficial for the body and brain.
- Surya Namaskar: This yoga practice, consisting of 12 different asanas, can be done along with proper breathing techniques to improve overall health.
- Mud Therapy: Applying mud to specific parts of the body can help with constipation and muscle rigidity.
- Shirodhara: A therapy where a continuous flow of herbal oil is poured over the forehead can be beneficial for memory-related problems, depression, insomnia, and dementia.
- Acupressure and Acupuncture: These therapies can be effective in managing symptoms if done by someone with a good knowledge of the pressure points and techniques.
These naturopathic treatments can complement conventional medical treatments and lifestyle modifications to improve the quality of life for Parkinson’s disease patients.
Here’s a summary of the herbs mentioned for managing Parkinson’s disease:
- Ashwagandha: It is considered a basic herb that can be beneficial for patients undergoing alternative therapies or other medications. It is known for its positive effects and is easily available in powdered or syrup form. Consuming one tablespoon of Ashwagandha churna with ghee or milk daily can be beneficial.
- Bala (Sida Cardifolia Linn): Also known as Sida Cardifolia Linn, Bala is another herb that can be helpful in managing Parkinson’s disease symptoms.
- Brahmi: Known for its brain-boosting properties, Brahmi can be beneficial for cognitive function.
- Tulsi: Known for its antiseptic and antibacterial properties, Tulsi can help clean the blood system.
- Trifala: A combination of three fruits – Harde, Bela, and Awla, Trifala can help with constipation, stomach cleansing, and digestion.
- Ginger, Pepper, and Cinnamon: These herbs can also be used for managing Parkinson’s disease.
It’s important to consult with a healthcare professional before incorporating these herbs into your treatment plan, especially if you are already taking medications or undergoing other therapies.
In conclusion, naturopathy offers a holistic approach to managing Parkinson’s disease, focusing on natural therapies and lifestyle modifications. Massage therapy, particularly whole-body massage or targeted massages, can be beneficial at all stages of the disease. Other therapies like Shirodhara, mud application, and sunbathing can help improve circulation, detoxify the body, and provide essential vitamin D.
Naturopathy also emphasizes the use of herbs like Ashwagandha, Bala, Brahmi, Tulsi, Trifala, ginger, pepper, and cinnamon, which are known for their beneficial properties in managing Parkinson’s symptoms. These herbs can be consumed in various forms like powders, syrups, or as part of a balanced diet.
Overall, naturopathy aims to enhance the body’s natural healing abilities and promote overall well-being, offering a complementary approach to conventional treatments for Parkinson’s disease.