Chronic Kidney Disease
Chronic Kidney Disease: A Naturopathic Perspective
Introduction
Kidney disease is a significant health concern that manifests primarily in two forms: chronic kidney disease (CKD) and chronic kidney failure. These conditions represent severe stages of kidney malfunction. From a naturopathic viewpoint, early detection and treatment of kidney disease are crucial in preventing its progression to a chronic state. This article delves into the nature of CKD, its progression, and how naturopathy can help manage and prevent it.
Types of Kidney Disease
Kidney disease can present itself as either acute or chronic. Acute kidney disease, when detected early, is highly reversible and treatable. Naturopathy boasts a 100% success rate in treating acute kidney conditions when addressed promptly. However, if the symptoms of acute kidney disease are neglected, the condition can gradually worsen and transition into chronic kidney disease.
The Progression to Chronic Kidney Disease
Most diseases, including kidney disease, progress gradually through various stages. It is rare for chronic kidney disease to develop suddenly; typically, the condition evolves over time. Early signs and symptoms of kidney dysfunction serve as indicators that something is amiss. Ignoring these symptoms and failing to seek timely treatment can result in the disease becoming chronic.
The Role of Naturopathy in Managing Kidney Disease
Naturopathy emphasizes the body’s innate ability to heal itself through natural means. For acute kidney conditions, naturopathy offers effective treatments that promote kidney health and prevent the progression to CKD. This approach includes dietary modifications, herbal remedies, and lifestyle changes designed to support kidney function and overall well-being.
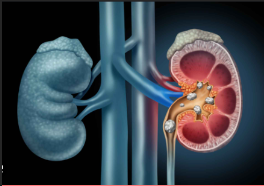
Understanding the Kidneys
Every human is naturally endowed with two kidneys, located on either side of the spine. Each person has a right kidney and a left kidney, which can vary in size. It is important to note that the size and weight of both kidneys are never identical in any individual. This natural asymmetry does not typically affect kidney function.
Chronic Kidney Disease: An Overview
Chronic kidney disease is characterized by a gradual loss of kidney function over time. Damaged kidneys are unable to filter blood effectively, leading to the accumulation of waste products in the body. This can result in various health complications, including hypertension, anemia, weak bones, and nerve damage.
Conclusion
Chronic kidney disease is a serious and often irreversible condition. However, early detection and intervention can prevent its progression. Naturopathy provides a holistic and natural approach to managing kidney health, emphasizing the importance of addressing symptoms promptly to avoid chronic kidney issues. By understanding and respecting the principles of naturopathy, individuals can take proactive steps to maintain kidney health and prevent disease progression.
The Vital Role of Kidneys: Nature's Gift and Their Functionality

Introduction
The kidneys are vital organs responsible for filtering waste products and excess substances from the blood to produce urine. They play a crucial role in maintaining the body’s overall health and well-being. This article explores the unique nature of kidneys, their functionality, and the importance of timely intervention in preventing chronic kidney disease.
Uniqueness of Kidneys
At birth, every individual is endowed with two kidneys, situated on either side of the spine. These kidneys are not identical in size or weight; there is always a difference between the two. This natural asymmetry is a unique feature of our anatomy. Remarkably, if one kidney becomes damaged or dysfunctional, the other kidney can sustain the body’s filtration needs, allowing the person to survive with just one kidney.
Understanding Kidney Functionality
The kidneys act as the body’s primary filtration system, akin to a strainer. Just as we strain coffee or juice to remove impurities, the kidneys filter out waste products, fibers, and excess substances from the blood. If the strainer is damaged, it cannot perform its function effectively. Similarly, if the kidneys are damaged, they may not be able to filter the blood properly, leading to a buildup of toxins and waste products in the body.
Nephrons: The Key Players in Kidney Function
Nephrons are tiny structures in the kidneys that play a crucial role in filtration. These structures filter the blood, remove waste products, and reabsorb essential substances, such as water and electrolytes, back into the bloodstream. Damage to the nephrons can impair kidney function, leading to various health issues.
The Risk of Chronic Kidney Disease
Chronic kidney disease (CKD) occurs when the kidneys are damaged and cannot filter blood properly over a prolonged period. Neglecting initial signs of kidney damage can result in the progression to CKD. While one kidney can often compensate for the other, both kidneys can be affected in certain cases, highlighting the importance of early detection and intervention.
Conclusion
The kidneys are a remarkable gift from nature, enabling our bodies to filter waste and maintain overall health. Understanding the kidneys’ function and the importance of their proper functioning is crucial in preventing chronic kidney disease. By recognizing the early signs of kidney damage and taking proactive steps to preserve kidney health, individuals can ensure the continued well-being of this vital organ system.
The Essential Functions of Kidneys: A Detailed Overview
Introduction
The kidneys play a pivotal role in maintaining the body’s overall health by filtering waste products and excess substances from the blood. This article explores the primary functions of the kidneys, emphasizing the importance of proper kidney function in eliminating toxins and maintaining overall well-being.
The Role of Filtration
The kidneys’ primary function is filtration, whereby they remove toxic products such as urea and creatinine from the blood. Failure to eliminate these waste products can lead to their accumulation in the body, placing a burden on other organs and potentially causing serious health issues.
Elimination of Unnecessary Fluids
In addition to filtering waste products, the kidneys also regulate the body’s fluid balance. Excessive water retention in tissues can lead to edema, causing discomfort and potentially affecting kidney function. Proper hydration is essential, but unnecessary fluids must be expelled to prevent strain on the kidneys and other organs.
Vitamin D3 Production and Absorption
One lesser-known function of the kidneys is their role in producing and absorbing vitamin D3. Vitamin D3 deficiency is a common health issue, particularly in regions like India and Asia, despite abundant sunlight. Vitamin D3 is crucial for various bodily functions, including bone health and immune system function. Proper kidney function is essential for maintaining adequate levels of this vital vitamin.
Conclusion
The kidneys are integral to the body’s filtration system, removing waste products and excess fluids to maintain overall health. Understanding the kidneys’ functions underscores the importance of maintaining their health and preventing kidney disease. Proper hydration, balanced nutrition, and regular check-ups are key to supporting kidney function and overall well-being.
The Interconnection of Vitamin D3, Kidney Health, and Digestive System

Introduction
Vitamin D3 plays a crucial role in our health, particularly in its relationship with kidney function and the digestive system. This article explores the significance of vitamin D3 absorption and production in the kidneys, its role in maintaining overall health, and how kidney problems can impact these processes.
The Role of Kidneys in Vitamin D3 Absorption
The kidneys are responsible for producing and absorbing vitamin D3, a vital nutrient that supports various bodily functions. Proper absorption of vitamin D3 is crucial for maintaining overall health, as it plays a role in bone health, immune function, and mood regulation.
Erythropoietin Production and Kidney Health
Additionally, the kidneys play a key role in producing erythropoietin, a hormone that stimulates the production of red blood cells in the bone marrow. Erythropoietin is essential for maintaining proper oxygen levels in the body and ensuring overall health and well-being.
Chronic Kidney Disease and its Impact
Chronic Kidney Disease (CKD) is a progressive and irreversible condition characterized by reduced kidney function or kidney damage. Once the kidneys are damaged, they are unable to function properly, leading to a gradual decline in kidney function. CKD is continuously progressive and not reversible. In advanced stages, dialysis may be required to filter waste products from the blood.
Preventing Kidney Damage with Naturopathy
Naturopathy can play a significant role in preventing kidney damage. By focusing on reducing kidney damage and supporting kidney function, naturopathy can help slow down the progression of CKD and improve overall kidney health. This approach may involve dietary changes, herbal remedies, and lifestyle modifications to support kidney function.
Conclusion
Understanding the interconnection between vitamin D3, kidney health, and the digestive system is crucial for maintaining overall health. Proper absorption and production of vitamin D3 by the kidneys are essential for various bodily functions. By prioritizing kidney health and ensuring adequate levels of vitamin D3, individuals can support their overall well-being and prevent complications associated with kidney disease.
Understanding the Stages of Chronic Kidney Disease (CKD) and Treatment Approaches

Introduction
Naturalists play a crucial role in understanding and treating different stages of chronic kidney disease (CKD). Diagnosis and treatment are based on the prognosis of CKD, categorized by glomerular filtration rate (GFR) and albuminuria. This article explores the stages of CKD and the corresponding treatment approaches.
Diagnosis and Prognosis of CKD
The stages of CKD are determined by GFR and albuminuria levels, as categorized in 2012. Naturalists use these indicators to assess the patient’s condition and tailor treatment accordingly. The primary goal is to halt the progression of kidney damage and preserve kidney function.
The Six Stages of CKD
- Stage G1 (GFR ≥ 90 ml/min): This stage indicates normal or slightly elevated GFR levels. With proper treatment, this stage is often reversible or curable within a certain period.
- Stage G2 (GFR 60-89 ml/min): GFR levels are mildly decreased at this stage, indicating the early stages of kidney damage.
- Stage G3 (GFR 30-59 ml/min): This stage is divided into G3a (GFR 45-59 ml/min) and G3b (GFR 30-44 ml/min). Despite the decreased GFR levels, there are still opportunities to protect kidney function. Dialysis or transplant is not necessary at this stage, as proper medication, diet, and treatment can manage the condition effectively.
- Stage G4 (GFR 15-29 ml/min): GFR levels are significantly decreased, indicating advanced kidney damage. At this stage, patients may require more intensive treatment and close monitoring.
- Stage G5 (GFR < 15 ml/min): This stage is also known as end-stage renal disease (ESRD), where kidney function is severely impaired. Dialysis or kidney transplant is often necessary at this stage to maintain proper kidney function.
- Stage G5D (Dialysis-dependent): This stage indicates that the patient is dependent on dialysis for kidney function. Kidney transplant may be considered as a long-term solution.
Conclusion
Understanding the stages of CKD is essential for naturalists to provide appropriate treatment and support to patients. By diagnosing CKD early and implementing proper treatment strategies, naturalists can help patients manage the condition effectively and preserve kidney function for as long as possible.
Comprehensive Overview of Chronic Kidney Disease (CKD) Stages and Treatment Strategies for Adults
Chronic kidney disease (CKD) is a progressive condition that can have serious implications for adult patients if not managed properly. Understanding the stages of CKD, as determined by glomerular filtration rate (GFR) and albuminuria levels, is crucial for guiding treatment decisions and improving patient outcomes. This article provides a detailed overview of the stages of CKD and the corresponding treatment strategies for adults.
Stages of CKD Based on GFR Levels
- Stage G1 (GFR ≥ 90 ml/min): This stage indicates normal or slightly elevated GFR levels, which can often be reversible with proper treatment. Patients in this stage may require lifestyle modifications, such as dietary changes and increased physical activity, to manage their condition effectively. 2
- Stage G2 (GFR 60-89 ml/min): GFR levels are mildly decreased at this stage, indicating early kidney damage. Treatment focuses on slowing the progression of CKD through medication and lifestyle changes.
- Stage G3 (GFR 30-59 ml/min): Stage G3 is divided into G3a (GFR 45-59 ml/min) and G3b (GFR 30-44 ml/min). At this stage, there are opportunities to protect kidney function and prevent further damage. Treatment may include medication to control blood pressure and manage underlying conditions such as diabetes.
- Stage G4 (GFR 15-29 ml/min): GFR levels are significantly decreased at this stage, indicating advanced kidney damage. Treatment aims to prevent complications and prepare for renal replacement therapy, such as dialysis or transplant.
- Stage G5 (GFR < 15 ml/min): This stage is also known as end-stage renal disease (ESRD), where kidney function is severely impaired. Treatment options include dialysis or kidney transplant to maintain proper kidney function and improve quality of life.
Albuminuria Levels and CKD Progression
Albuminuria levels, categorized as A1 (mildly increased), A2 (moderately increased), and A3 (severely increased), play a role in determining the severity of CKD. The combination of GFR and albuminuria levels helps classify the stage of CKD and guide treatment decisions.
Treatment Considerations Based on Staging
- Acute vs. Chronic: In the early stages (G1-G3, A1-A2), CKD is often acute and reversible with proper treatment. However, in the later stages (G4-G5, A3), CKD becomes chronic and may require dialysis or transplant.
- Dialysis and Transplant: Stage G5 with A3 albuminuria represents the most severe form of CKD, requiring dialysis or kidney transplant. These treatments aim to replace the lost kidney function and improve the patient’s quality of life.
Conclusion
Managing CKD requires a comprehensive approach that considers the stage of the disease, GFR levels, albuminuria levels, and the patient’s overall health. Early diagnosis and intervention are key to slowing the progression of CKD and improving patient outcomes. By understanding the stages of CKD and the corresponding treatment strategies, healthcare providers can provide optimal care for adult patients with CKD.
Understanding Chronic Kidney Disease (CKD): Root Causes and Naturopathic Approaches to Treatment

Chronic kidney disease (CKD) is a complex condition that requires a comprehensive approach to treatment. Understanding the root causes of CKD and implementing naturopathic strategies can help manage the condition effectively. This article explores the common root causes of CKD and naturopathic approaches to treatment based on the stages of the disease.
Importance of Staging in CKD Treatment
When a patient is diagnosed with CKD, the stage of the disease is determined based on glomerular filtration rate (GFR) and albuminuria levels. This staging is crucial for deciding the appropriate treatment approach. Naturopaths use this information to recommend dietary changes and other lifestyle modifications that can help manage the condition.
Dietary Recommendations Based on CKD Stage
- Stages G1-G3: Patients in these stages are encouraged to have a higher fluid intake to maintain kidney function. Naturopaths may recommend a diet rich in fruits, vegetables, and whole grains to support overall kidney health.
- Stages G4-G5 and A3: Patients in these stages are advised to limit their fluid intake to less than 1 liter per day. A diet low in protein and phosphorus may be recommended to reduce the workload on the kidneys.
Common Root Causes of CKD
- Diabetic Neuropathy: Approximately 90% of CKD patients have diabetic neuropathy. Prolonged high sugar levels in diabetic patients can lead to kidney damage over time. Patients with a long history of diabetes are at a higher risk of developing CKD.
- Glomerulonephritis: Glomerulonephritis is another common cause of CKD. This condition involves inflammation of the glomeruli, the tiny filters in the kidneys that help remove waste from the blood.
- Hypertension: High blood pressure is closely associated with CKD. Managing hypertension through lifestyle changes and medication can help prevent further kidney damage.
Lifestyle Diseases and CKD
Diabetes, hypertension, and high cholesterol are considered lifestyle diseases and are major risk factors for CKD. Patients with these conditions need to manage their health carefully to prevent the progression of CKD.
Naturopathic Approaches to CKD Treatment
Naturopaths focus on addressing the root causes of CKD through dietary changes, herbal remedies, and lifestyle modifications. By targeting these underlying issues, naturopaths aim to slow down the progression of CKD and improve the overall health and well-being of patients.
Conclusion
CKD is a complex condition that requires a comprehensive treatment approach. By understanding the root causes of CKD and implementing naturopathic strategies, patients can manage the condition effectively and improve their quality of life. Regular monitoring and follow-up with a healthcare provider are essential for managing CKD and preventing complications.
Understanding Hypertension and Other Risk Factors for CKD: Clinical Manifestations and Naturopathic Perspectives
Chronic kidney disease (CKD) is influenced by various factors, including hypertension, genetic predisposition, and recurrent kidney stones. Understanding these risk factors and their clinical manifestations is crucial for effective management. This article explores the relationship between hypertension, genetic factors, kidney stones, and CKD, along with naturopathic perspectives on prevention and treatment.
Hypertension and Vascular Health
Hypertension is a common risk factor for CKD, affecting vascular and ischemic kidney disease. The increased burden on the kidneys due to hypertension can lead to the accumulation of toxic products in the body, impacting kidney function. Naturopathic approaches to managing hypertension focus on dietary changes, lifestyle modifications, and herbal remedies to improve vascular health and reduce kidney burden.
Autosomal Dominant Polycystic Kidney Disease (ADPKD)
ADPKD is a genetic condition that can lead to CKD. Individuals with a family history of CKD, including their parents and siblings, are at higher risk. Naturopathic interventions for ADPKD focus on slowing disease progression and improving kidney function through holistic approaches.
Recurrent Kidney Stones
Recurrent kidney stones can increase the risk of CKD, especially if the stones are large and frequent. Naturopathic treatments aim to prevent stone formation through dietary modifications, hydration, and herbal remedies. Managing recurrent kidney stones can help reduce the risk of CKD development.
Clinical Manifestations of CKD
Clinical manifestations of CKD include fatigue, weakness, swelling in the legs, and changes in urination patterns. Naturopathic practitioners focus on addressing these symptoms through lifestyle changes, dietary modifications, and herbal therapies. Early detection and intervention are crucial in managing CKD and improving quality of life.
Naturopathic Perspectives on CKD Prevention and Treatment
Naturopathic approaches to CKD prevention and treatment emphasize the importance of holistic care. By addressing underlying risk factors, such as hypertension and genetic predisposition, and promoting kidney health through natural interventions, naturopaths aim to slow disease progression and improve patient outcomes.
Conclusion
CKD is a complex condition influenced by various factors. Understanding the role of hypertension, genetic predisposition, and recurrent kidney stones in CKD development is essential for effective management. Naturopathic interventions focus on addressing these risk factors and promoting kidney health through holistic approaches, ultimately improving patient quality of life. Regular monitoring and collaboration with healthcare providers are key in managing CKD and reducing its complications.
Understanding Dyselectrolytemia and its Impact on Kidney Function
Dyselectrolytemia refers to an imbalance of electrolytes in the body, including sodium, potassium, and calcium. These electrolytes play a crucial role in various bodily functions, especially kidney function. Understanding the normal ranges of these electrolytes and their implications for kidney health is essential for maintaining overall well-being.
Sodium (Na+)
Sodium is a key electrolyte that helps maintain fluid balance in the body. The normal range of sodium in adults is 135 to 145 mEq /L. When sodium levels are elevated, a condition known as hypernatremia occurs. This can be caused by decreased excretion by the glomeruli. Conversely, hyponatremia, or low sodium levels, can lead to fluid retention and tissue swelling, ultimately affecting glomerular filtration rate (GFR) and damaging nephrons.
Potassium (K+)
Potassium is essential for muscle function, nerve transmission, and maintaining fluid balance. The normal range of potassium is 3.5 to 5.0 mmol/L. Hyperkalemia, or high potassium levels, can result from decreased excretion by the glomeruli, use of potassium-sparing diuretics, or metabolic acidosis. On the other hand, hypokalemia, or low potassium levels, can occur due to decreased intake of potassium or the use of diuretics.
Calcium (Ca2+)
Calcium plays a vital role in muscle function, nerve transmission, and bone health. The normal range of calcium is 8.5 to 10.2 mg/dL. Hypocalcemia, or low calcium levels, can result from decreased vitamin D activation in the kidneys or decreased absorption of calcium by the gastrointestinal tract. Hypercalcemia, or high calcium levels, can be caused by hyperparathyroidism or nephrogenic diabetes insipidus.
Impact on Kidney Function
Dyselectrolytemia can have a significant impact on kidney function. Imbalances in electrolytes can affect the glomerular filtration rate and the overall health of the nephrons. It is essential to maintain electrolyte balance through proper diet, hydration, and monitoring of electrolyte levels to prevent complications and maintain kidney health.
Conclusion
Maintaining electrolyte balance is crucial for kidney health and overall well-being. Understanding the normal ranges of sodium, potassium, and calcium, and their impact on kidney function, can help individuals take proactive steps to maintain proper electrolyte balance and prevent complications associated with dyselectrolytemia. Regular monitoring of electrolyte levels and consulting with healthcare providers can help ensure optimal kidney health.
Impact of Dyselectrolytemia on the Cardiovascular and Nervous Systems

Dyselectrolytemia, characterized by an imbalance of electrolytes such as sodium, potassium, and calcium, can have profound effects on various systems in the body, including the cardiovascular and nervous systems. Understanding these manifestations is crucial for managing chronic kidney disease (CKD) and its associated complications.
Cardiovascular System
One of the primary manifestations of dyselectrolytemia in the cardiovascular system is hypertension, which is common in CKD patients. Hypertension can lead to complications such as pericarditis, a condition characterized by inflammation of the pericardium, the sac around the heart. Additionally, dyselectrolytemia can contribute to ischemic heart disease, which affects blood flow to the heart muscle.
Central Nervous System
Dyselectrolytemia can also affect the central nervous system, leading to seizures and uremic encephalopathy. Seizures may occur due to electrolyte imbalances, while uremic encephalopathy is a condition characterized by the accumulation of toxins in the body, affecting brain function.
Peripheral Nervous System
The peripheral nervous system can be affected by dyselectrolytemia, leading to peripheral neuropathy and myopathy. Peripheral neuropathy is a common complication characterized by nerve damage, while myopathy refers to muscle weakness or disease. Uremic toxins can contribute to the development of these conditions.
Bone Health
Dyselectrolytemia can also impact bone health, leading to conditions such as osteitis fibrosa cystica and renal osteomalacia. Osteitis fibrosa cystica is characterized by chronic inflammation and changes in bone structure, while renal osteomalacia involves mineralization issues and vitamin D deficiency.
Conclusion
Dyselectrolytemia can have far-reaching effects on the body, impacting not only the cardiovascular and nervous systems but also bone health. Managing electrolyte imbalances through diet, hydration, and proper medical treatment is crucial in preventing these complications and maintaining overall health. Regular monitoring of electrolyte levels and collaboration with healthcare providers are essential in managing dyselectrolytemia and its associated manifestations.
Adynamic Bone Disease and Anemia in Chronic Kidney Disease
Adynamic Bone Disease and Anemia in Chronic Kidney Disease
Adynamic bone disease and anemia are common complications of chronic kidney disease (CKD), often associated with vitamin D deficiency and decreased red blood cell production. Understanding these complications is crucial for effective management and treatment of CKD patients.
Adynamic Bone Disease
- Vitamin D3 Deficiency: CKD patients with vitamin D3 deficiency may require supplements to maintain optimal levels. However, excessive vitamin D supplementation can lead to toxemia and contribute to adynamic bone disease.
- Treatment Duration: Doctors may prescribe vitamin D supplements for one to two months, but some patients may require them for up to six months. Prolonged supplementation should be monitored to avoid toxemia.
- Adynamic Bone Disease: Excessive vitamin D intake can lead to adynamic bone disease, characterized by weakened bones and increased risk of fractures. This condition is a result of disrupted bone remodeling due to excessive vitamin D levels.
Anemia in CKD
- Low Hemoglobin Levels: Anemia is common in CKD patients due to decreased red blood cell production. Vitamin B12 and folic acid deficiency can also contribute to anemia.
- Treatment: Folic acid supplements are often prescribed to maintain hemoglobin levels. Severe cases may require blood transfusions to restore hemoglobin levels.
- Hyperparathyroidism and Blood Loss: Hyperparathyroidism and excessive blood loss can also contribute to low hemoglobin levels in CKD patients.
Diagnosis and Management
- Blood Tests: Blood tests are used to monitor hemoglobin levels, vitamin D levels, and other markers of kidney function.
- Urine Tests: Urine tests can detect proteinuria, which is common in CKD patients and can indicate kidney damage.
- Imaging: Imaging tests like X-rays and bone scans can help assess bone health and detect abnormalities associated with adynamic bone disease.
Conclusion
Adynamic bone disease and anemia are significant complications of CKD that require careful management. Monitoring vitamin D levels, hemoglobin levels, and kidney function through regular blood and urine tests is essential. Collaboration between patients, healthcare providers, and specialists is crucial for effectively managing these complications and improving the quality of life for CKD patients.
Renal Function Tests and Diagnostic Criteria for Kidney Disease
When diagnosing and treating kidney disease, healthcare providers rely on a variety of tests to assess kidney function and overall health. Understanding these tests and their results is crucial for proper management and treatment of kidney disease.
Blood Tests
- Renal Function Test (RFT): This test evaluates kidney function by measuring levels of various substances in the blood.
- S. Uric Acid: Normal range is 3.5 to 7.2 mg/dL.
- BUN (Blood Urea Nitrogen): Normal range is 7 to 20 mg/dL.
- eGFR (Estimated Glomerular Filtration Rate): Normal level is 90 ml/min or higher.
- S. Creatinine: Normal range is 0.7 to 1.3 mg/dL.
- S. Albumin: Normal range is 3.5 to 5.0 mg/dL.
Urine Tests
- Urine Analysis: Provides information on glucose and protein levels in the urine, which can indicate kidney damage.
- Tubular Function Test: Assesses specific gravity and urine dilution, helping to evaluate kidney function and health.
Treatment Considerations
- Precautions and Therapy: There is no specific therapy for kidney disease. Treatment depends on understanding the underlying causes and clinical manifestations.
- Clinical Manifestations: Understanding the deficiencies and imbalances that contribute to kidney disease is essential for effective treatment.
- Comprehensive Approach: Treatment should address all aspects of kidney disease, including cardiovascular health and electrolyte balance, to ensure optimal outcomes.
Conclusion
Proper diagnosis and treatment of kidney disease require a thorough understanding of the patient’s clinical manifestations and test results. A comprehensive approach that addresses all aspects of kidney health is crucial for improving patient outcomes and quality of life.
Importance of Manifestations in CKD Treatment and Naturopathic Approach

Chronic Kidney Disease (CKD) is a complex condition that requires a comprehensive approach to treatment. Understanding the manifestations of CKD is crucial for developing an effective treatment plan. While CKD is irreversible, naturopathy can help slow down the progression of the disease and improve quality of life.
Importance of Manifestations in Treatment
- No Direct Therapy: Therapy for CKD may not directly work if the patient has low hemoglobin levels or other underlying issues. Understanding the manifestations helps tailor treatment to address these specific concerns.
- Addressing Root Causes: Naturopathy focuses on addressing the root causes of CKD. For example, if CKD is associated with obesity, the first step is to manage weight to reduce burden on the kidneys.
- Blood Pressure and Sugar Control: For overweight individuals with CKD, controlling blood pressure and high sugar levels is crucial. This can help reduce strain on the kidneys and slow down disease progression.
Naturopathic Approach
- Reducing Uric Acid Levels: High uric acid levels can lead to increased creatinine levels. Naturopathy aims to reduce uric acid levels through dietary changes and natural remedies.
- Targeting Root Causes: Naturopathy targets the root causes of CKD to slow down disease progression. This includes addressing obesity, high blood pressure, and other contributing factors.
- Improving Blood Health: Naturopathy emphasizes the importance of maintaining healthy hemoglobin levels and treating underlying issues that affect red blood cell function.
Conclusion
Understanding the manifestations of CKD is essential for developing an effective treatment plan. Naturopathy offers a holistic approach to managing CKD by addressing root causes, improving blood health, and slowing down disease progression. By targeting the root causes and symptoms, naturopathy can help improve the quality of life for individuals with CKD.
Importance of Diet in CKD Management

Diet plays a crucial role in managing Chronic Kidney Disease (CKD). Patients are advised to reduce protein intake as it takes longer to digest and can burden the kidneys. Without the help of other fibers and vitamins, protein digestion may be incomplete, leading to acidic byproducts that strain the kidneys. Naturopaths often recommend reducing or stopping protein intake to ease this burden and minimize fluid retention.
Minimizing Fluid Intake
In CKD, damaged nephrons reduce the kidney’s ability to filter fluids properly. Excessive fluid intake can lead to fluid retention and inflammation in the body, noticeable as puffiness under the eyes and swelling in the legs. To prevent this, patients are advised to minimize fluid intake. For those with a creatinine level of 6 or 6.5, limiting fluid intake to 1 liter per day is often recommended, including fluids from tea or coffee.
Low Carbohydrate and Low Sodium Diet
A low-carbohydrate and low-sodium diet is beneficial for managing CKD, especially if hypertension is present. High sodium intake can strain the kidneys, leading to further damage. By reducing salt intake, nephrons can rest, allowing for better kidney function. Diuretics may be prescribed in severe cases, but it’s preferable to focus on dietary adjustments to manage fluid retention and inflammation.
Conclusion
Dietary changes are crucial in managing CKD. Reducing protein intake, minimizing fluid intake, and adopting a low-carbohydrate, low-sodium diet can help ease the burden on the kidneys and improve overall kidney function. Naturopaths emphasize these dietary modifications to manage CKD effectively and improve the quality of life for patients.
Naturopathic Approaches to CKD Management
Chronic Kidney Disease (CKD) requires a holistic approach to treatment, including dietary changes and natural remedies. Naturopaths focus on reducing the burden on the kidneys by advocating for a low-carbohydrate diet, which allows other organs to rest and promotes the body’s natural regenerative capacity.
Dietary Recommendations
- Low Carbohydrate Diet: A low-carb diet is easier to digest, giving the body’s organs, especially the kidneys, a chance to recover. This approach allows damaged organs to heal on their own and reduces the workload on the kidneys.
- Fruits and Vegetables: Including a variety of fruits and green leafy vegetables in the diet provides essential nutrients and supports overall health. These foods are rich in vitamins, minerals, and antioxidants, which can help protect the kidneys from further damage.
- Fluid Intake: Coconut water and barley water are excellent remedies for maintaining hydration and supporting kidney function. These beverages are natural diuretics, helping to flush out toxins from the body and reduce the workload on the kidneys.
Home Remedies
- Coriander and Jeera Tea: This herbal tea helps lower uric acid levels, beneficial for individuals with hypertension and high cholesterol. Coriander and cumin seeds are known for their diuretic properties, which can help reduce fluid retention and support kidney function.
- Cabbage and Fenugreek Juice: Juices made from cabbage and fenugreek leaves, when mixed with water, are beneficial for CKD patients. These juices are rich in antioxidants and anti-inflammatory compounds, which can help reduce inflammation in the kidneys and improve kidney function.
Natural Supplements
- Tulsi Sudha: Tulsi (holy basil) is a natural diuretic that can help reactivate nephrons, making it a valuable supplement for CKD patients. Tulsi is also known for its antioxidant and anti-inflammatory properties, which can help protect the kidneys from further damage.
- Other Supplements: Omega-3 fatty acids, probiotics, and vitamin D supplements may also be beneficial for CKD patients. Omega-3 fatty acids have anti-inflammatory properties, which can help reduce inflammation in the kidneys. Probiotics can help maintain gut health, which is important for overall health and immune function. Vitamin D is important for bone health and may help reduce the risk of complications associated with CKD.
Other Therapies
- Hot and Cold Tub Bath: Alternating between 10 minutes of hot and cold baths or using a GH pack can help manage CKD symptoms. Hot and cold therapies can help improve blood circulation and reduce inflammation, which can help alleviate pain and discomfort associated with CKD.
Conclusion
Naturopathic therapies for CKD focus on dietary modifications, herbal remedies, and natural supplements to support kidney function and overall health. These approaches aim to reduce the burden on the kidneys and promote the body’s natural healing processes, enhancing the quality of life for CKD patients.
Additional Therapies for Managing CKD
In addition to dietary changes and natural remedies, certain therapies can help manage Chronic Kidney Disease (CKD) by reducing creatinine levels and improving overall well-being. These therapies focus on promoting detoxification, improving circulation, and supporting kidney function.
Deep Breathing Exercises
Regular deep breathing exercises help increase oxygen flow in the body, which is essential for clearing toxins and repairing damaged cells. Deep breathing can be practiced daily for improved kidney function and overall health.
Anima Therapy
Anima therapy involves the use of enemas to cleanse the colon and remove toxins from the body. This therapy is beneficial for patients experiencing symptoms like indigestion, bloating, low appetite, and overweight. Anima therapy can be performed for 4-5 days under the guidance of a healthcare professional.
Massage Therapy
Regular massages, done once or twice a month, can improve blood circulation and provide relaxation to CKD patients. However, massage should be avoided if the body is inflamed or swollen.
Steam Bath
Steam baths, lasting 3-5 minutes, help eliminate toxins from the body through sweating. This therapy is beneficial for patients with controlled blood pressure and cholesterol levels, who are not on any medications or treatments that could interfere with the steam bath.
Conclusion
These additional therapies can complement the naturopathic approach to managing CKD by promoting detoxification, improving circulation, and supporting overall kidney health. However, it is important to consult with a healthcare professional before starting any new therapy, especially for individuals with underlying health conditions or those on medications.
Herbal Remedies for Managing CKD
Chronic Kidney Disease (CKD) can be managed and symptoms alleviated with the help of various herbs known for their beneficial effects on kidney function. These herbs can be consumed in different forms, such as powders, tablets, or fresh juice, depending on individual preferences and health conditions.
Wheatgrass: A Potent Herbal Remedy
Wheatgrass is renowned for its diverse health benefits, ranging from improving digestion to enhancing kidney function. It is rich in essential nutrients and antioxidants, making it an effective remedy for managing CKD. While fresh wheatgrass juice is highly recommended, CKD patients with fluid restrictions can opt for wheatgrass powder or tablets to reap its benefits.
Punarnava, Gokshru, and Kasni: Nature’s Diuretics
Punarnava, Gokshru, and Kasni are herbs known for their diuretic properties, which can help in reducing water retention and inflammation in the kidneys. These herbs are particularly beneficial for CKD patients, aiding in improving kidney function and reducing creatinine levels.
Neem and Peepal Tree Bark: Natural Kidney Tonics
The barks of neem and peepal trees have been used traditionally as kidney tonics. Boiling these barks in water to create a decoction can be an effective remedy for managing CKD symptoms. This decoction is believed to improve kidney function and reduce creatinine levels when consumed regularly.
Incorporating Herbal Remedies Safely
It’s important to note that while these herbal remedies can be beneficial, they should be used cautiously and under the guidance of a healthcare professional. Some herbs may interact with medications or other treatments, so it’s crucial to seek advice before starting any herbal regimen, especially for individuals with CKD.
Herbal Remedies for Chronic Kidney Disease (CKD)
Managing CKD involves a holistic approach that includes dietary changes, lifestyle modifications, and herbal remedies. Several herbs have shown promise in supporting kidney health and reducing symptoms associated with CKD.
Guduchi (Giloy) and Moringa: Nutrient-Rich Herbal Supplements
Guduchi, also known as Giloy, and Moringa are rich in nutrients, including protein and calcium, making them excellent supplements for CKD patients. While fresh leaves can be used in salads or cooked dishes, powdered forms or tablets are convenient alternatives when fresh options are not available.
Integrating Herbs into the Diet
Herbal supplements can play a crucial role in managing CKD symptoms and supporting kidney function. However, it’s important to consult with a healthcare professional before starting any herbal regimen, especially if you have CKD or are taking medications.
Dietary Considerations for CKD Patients
For CKD patients with diabetes, dietary restrictions become more stringent. A diet low in carbohydrates, protein, and sodium is often recommended. Additionally, limiting fluid intake and customizing the diet according to individual health conditions can further support kidney health.
Conclusion: Supporting Kidney Health Naturally
Incorporating herbal remedies into the management of CKD can be beneficial, but it’s essential to do so under the guidance of a healthcare provider. By following a comprehensive treatment plan that includes herbal supplements, dietary modifications, and lifestyle changes, CKD patients can better manage their condition and improve their overall quality of life.







