CORONARY ARTERY DISEASE (CAD)
Understanding Heart Health: Why Prevention Matters More Than Ever
Welcome to Saffron Educational and Medical Foundation — an opportunity to become your own doctor.
Due to unexpected medical emergencies, Dr. Tanja could not conduct today’s lecture. On her behalf, I will be continuing the session. We sincerely apologize for the inconvenience caused last week due to the sudden cancellation and postponement of the lecture. Thank you all for your patience, understanding, and cooperation.
The Importance of Heart Health
The heart is one of the most vital organs of the human body. While we often associate the word “heartbreak” with emotional experiences, actual heart problems arise when there is an imbalance or disease affecting the heart muscles, arteries, or blood flow. Conditions such as high cholesterol, elevated triglyceride levels, arterial blockages, and heart muscle weakness can significantly impact overall heart health.
Heart health requires serious attention because in many cases, symptoms do not appear until the condition becomes severe. This makes awareness and preventive efforts extremely important.

A Growing Concern: Sudden Cardiac Arrest in Young Adults
In recent years, there has been an alarming rise in sudden cardiac arrest among young individuals, including celebrities between the ages of 30 and 40. Many of these incidents occur without any prior symptoms, leading to sudden collapse or even death.
This trend is influenced by various factors such as stress, unhealthy lifestyle habits, poor dietary choices, lack of physical activity, and undiagnosed underlying conditions. While some cardiac events may be unpredictable, preventive measures still play a vital role in reducing risks.
Why Students Must Understand Heart Diseases
Due to the increasing number of coronary artery disease (CAD) cases, the topic of heart health—particularly atherosclerosis—has been included at the bachelor’s level. Previously, this lecture was mainly reserved for master’s students. However, considering the present scenario and the growing number of young patients, it has become necessary for bachelor students as well.
Future practitioners and upcoming doctors must understand the risk factors, disease mechanisms, early signs, and preventive care related to heart disorders. With coronary artery disease cases rising rapidly, this knowledge is essential for providing effective guidance and support to patients.
Understanding Coronary Artery Disease (CAD) and Heart Structure
In recent years, the number of people suffering from heart problems is increasing day by day, especially among young individuals. To address this issue, it is important to understand what coronary artery disease (CAD) is, why it occurs, and what the root causes are. Naturopathy offers highly effective solutions and often achieves excellent results in improving heart health.
The Heart: Anatomy and Physiology
To understand heart-related problems, it is essential to first understand the structure and functioning of the heart. While this falls under basic anatomy and physiology, a brief review is helpful for building a clear foundation.
The heart is a hollow muscular organ responsible for pumping blood throughout the circulatory system. Its constant pumping action ensures that oxygen and nutrients reach every part of the body.
Many people are familiar with the heart symbol, often used to represent love. However, the actual human heart does not resemble this iconic shape. The symbolic heart is a representation, not an accurate depiction of the organ’s structure.
Size and Weight of the Heart
Despite its vital role, the heart is relatively small. The average length of the heart is about 10 cm. Its weight differs slightly between genders, with the female heart weighing approximately 225 grams and the male heart around 310 grams.
Even though the heart is small in size, its importance cannot be overstated. If the heart stops pumping for even 2 to 3 seconds, the body immediately suffers consequences due to the interruption of blood flow. This demonstrates the crucial role of the heart in sustaining life.
Heart Location and Structure: Understanding Its Anatomy
The heart is not only vital for pumping blood but also for maintaining the proper functioning of the entire body. If the heart stops functioning correctly, it can damage the brain, disrupt the body’s systems, impair breathing, and lead to serious health consequences.
Location of the Heart
The heart is located in the thoracic cavity, within the mediastinum — the space between the two lungs. While many people think the heart is slightly to the left, it is actually positioned in the middle of the chest cavity, with a small portion extending slightly to the right. This placement explains why, during heart-related discomfort or pain, sensations often radiate slightly to the right side of the chest rather than being exactly central.
Layers of the Heart Wall
The heart’s structure is a marvel of natural engineering. To protect this most sensitive organ, nature has designed it with three distinct layers:
- Pericardium – the outermost protective layer.
- Myocardium – the thick middle layer composed of cardiac muscle, responsible for the heart’s pumping action.
- Endocardium – the innermo st layer lining the heart chambers.
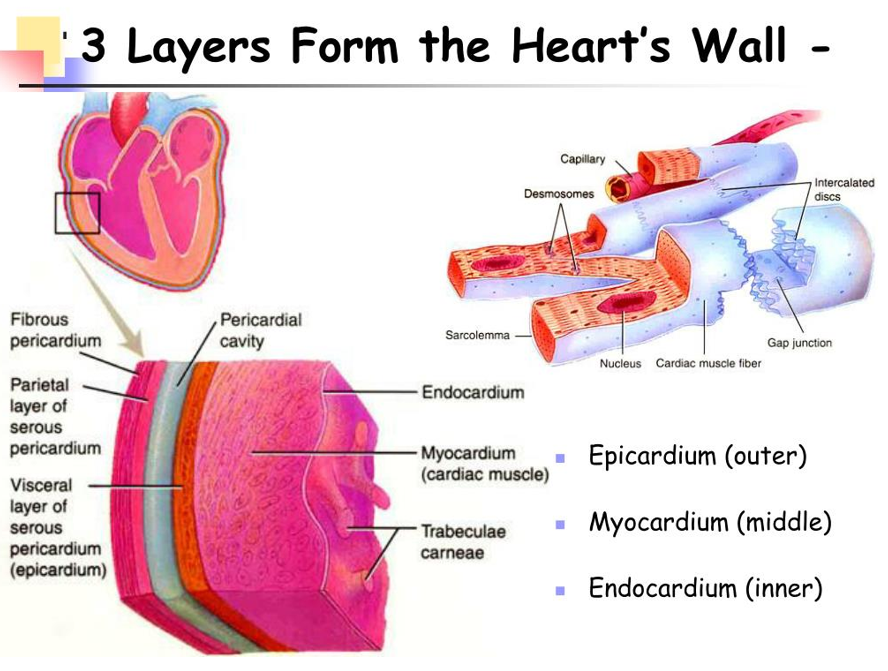
Understanding these layers is crucial for anyone studying heart health. When discussing cardiac conditions with patients or colleagues, these terms are often used to pinpoint the exact location of a problem. For example, if an issue is identified in the pericardium, it indicates that the outer layer of the heart is affected.
The human heart is a complex muscular organ responsible for maintaining systemic and pulmonary circulation, ensuring that oxygen-rich blood reaches every tissue and organ of the body. It is essential for students and medical enthusiasts to understand the anatomical structure and functional organization of the heart, especially when interpreting diagnostic reports or understanding pathological conditions. The heart is composed of four chambers: two atria (right and left) and two ventricles (right and left). These chambers are not exactly equal in size; the atria are relatively smaller, thin-walled structures designed primarily for receiving blood, while the ventricles have thicker walls and are responsible for pumping blood with sufficient force to reach the lungs and the systemic circulation.
The heart is further supported by three distinct layers, each with specific functional significance. The outermost layer, the epicardium, serves as a protective covering; the middle muscular layer, the myocardium, is responsible for the contractile function of the heart; and the innermost layer, the endocardium, lines the chambers and valves, ensuring smooth blood flow and preventing clot formation. Knowledge of these layers, particularly the myocardium and endocardium, is critical because pathological changes in these layers, such as ischemia, hypertrophy, or inflammation, often determine the clinical presentation and management of cardiac diseases.
To facilitate efficient blood circulation, the heart is supported by several walls and structures. The ventricular walls, including the interventricular septum, separate the right and left ventricles and prevent the mixing of oxygen-rich and oxygen-poor blood. The atrial walls separate the right and left atria. Each wall has specific clinical significance because most diagnostic reports, such as echocardiograms or cardiac MRI, mention precise locations like the anterolateral wall, inferior wall, septal wall, and posterior wall. This terminology is essential for identifying the site of infarction, wall motion abnormalities, or areas affected by structural heart disease.
The blood vessels associated with the heart play a crucial role in maintaining circulation. The superior and inferior venae cavae bring oxygen-poor blood from the systemic circulation into the right atrium. Blood then passes through the tricuspid valve into the right ventricle, which contracts to propel blood through the pulmonary valve into the pulmonary artery. In the lungs, carbon dioxide is exchanged for oxygen, and oxygen-rich blood returns to the left atrium via the pulmonary veins. From the left atrium, blood passes through the mitral valve into the left ventricle, which pumps oxygen-rich blood through the aortic valve into the aorta, supplying the entire body with oxygenated blood.
The circulation of oxygen-rich and oxygen-poor blood is essential for maintaining organ function, particularly in the brain. The brain relies exclusively on oxygen and glucose supplied by the blood for neuronal activity and overall cognitive function. If the oxygen content or quality of blood is insufficient, symptoms such as dizziness, fatigue, memory deficits, or drowsiness may occur. Thus, the heart’s efficiency in pumping oxygenated blood and maintaining proper circulation is critical for sustaining life and optimal organ function.
The interconnected nature of the heart and vascular system demonstrates the complexity of the human circulatory system. Each chamber, wall, valve, and vessel has a specific role in maintaining unidirectional blood flow and preventing mixing of oxygenated and deoxygenated blood. The pulmonary circulation, involving the right ventricle, pulmonary artery, lungs, and pulmonary veins, ensures oxygenation of blood, while the systemic circulation, starting from the left ventricle and aorta, distributes oxygen-rich blood to every tissue and organ. Proper understanding of these anatomical and functional aspects, including the myocardium, endocardium, and ventricular septum, is essential for interpreting cardiac pathologies, planning interventions, and comprehending how the heart sustains the entire body’s physiological needs.
The human circulatory system is an intricate and highly efficient transportation network that ensures every tissue and organ in the body receives an adequate supply of oxygen-rich blood, often referred to as “live blood.” Even in the case of a minor injury, such as a single scratch, blood immediately comes to the surface, demonstrating the efficiency and responsiveness of this system. This remarkable phenomenon is possible because the cardiovascular system functions as the body’s largest transportation network, capable of delivering nutrient-rich and oxygenated blood to all tissues while simultaneously removing deoxygenated blood and metabolic waste products. The oxygen-poor or deoxygenated blood is transported from the right ventricle into the pulmonary artery, which carries it to the lungs. In the lungs, oxygen diffuses into the blood while carbon dioxide and other metabolic waste products are removed. This process effectively purifies the blood, converting it from oxygen-poor to oxygen-rich, which is then returned to the left atrium via the pulmonary veins for systemic circulation.
One of the major pathological conditions affecting the cardiovascular system is atherosclerosis, defined as the abnormal accumulation of lipid substances—commonly referred to as fatty deposits—within the arterial walls. Under normal physiological conditions, the lining of blood vessels, particularly the arteries, appears uniform and free of obstruction. Healthy arteries, when observed microscopically, show a consistent red coloration, indicating unobstructed blood flow. However, in atherosclerosis, yellowish deposits of lipids accumulate within the endothelial lining of the arterial walls. This accumulation leads to narrowing of the arterial lumen, obstructing blood flow and reducing oxygen delivery to the myocardium, which is the contractile muscular layer of the heart. These terms, such as myocardium and endothelium, are crucial for understanding the localization and severity of circulatory issues, and they frequently appear in medical reports and diagnostic imaging.
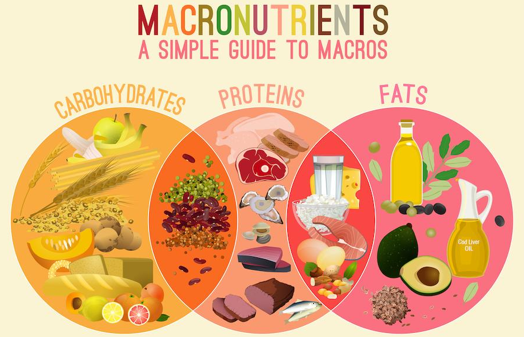
It is a common misconception that lipid accumulation occurs solely due to excessive consumption of ghee, oils, or fatty foods. While dietary intake may influence lipid levels, the process is multifactorial, involving genetic predisposition, metabolic activity, lifestyle, and overall systemic health. In fact, moderate consumption of natural fats, such as ghee or cold-pressed oils, is necessary to maintain the structural integrity of blood vessel walls and to act as a lubricant for joint and tissue function. Completely eliminating fats from the diet can lead to tissue dryness and increased stiffness, not only in the skin but also within vascular walls, which can impair circulation. Hence, the presence of a small proportion of dietary fats is essential for maintaining vascular flexibility and ensuring unobstructed blood flow throughout the body.
As lipid deposits accumulate and arterial lumens narrow, blood flow is impeded, resulting in decreased oxygen delivery to various organs and tissues. The myocardium, in particular, is highly sensitive to reduced blood flow because it requires continuous oxygen and nutrient supply for effective contraction and cardiac output. When blood flow is compromised due to atherosclerotic narrowing, the transport system of the body is affected, leading to slower circulation and insufficient delivery of oxygen and glucose to vital organs. Over time, this can result in progressive cardiovascular complications, including ischemia, myocardial infarction, and systemic circulatory abnormalities. The initial detection of such conditions is often through a lipid profile test, which measures the concentration of total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides in the blood.
Several risk factors contribute to the development of atherosclerosis and related cardiovascular diseases. While some factors may be genetically predetermined, a significant proportion of cardiovascular problems—approximately 90%—are self-inflicted due to lifestyle choices, lack of awareness, or incomplete understanding of dietary and health practices. Social influences, media trends, and widespread adoption of fad diets, such as zero-oil or strictly vegan diets, often lead individuals to unknowingly compromise essential nutrient intake. Without proper supplementation or guidance, these practices can induce deficiencies in critical fatty acids and other nutrients necessary for maintaining vascular health, leading to stiffness, reduced elasticity, and impaired blood circulation.
It is therefore critical to approach dietary and lifestyle changes with comprehensive knowledge of both their benefits and potential side effects. Partial understanding or misinformation can be detrimental, particularly when addressing complex systems such as the cardiovascular network. Maintaining traditional dietary habits that are aligned with one’s regional, seasonal, and cultural practices has been consistently associated with better cardiovascular outcomes. While exploring diverse cuisines is acceptable, adhering to a diet that provides balanced fats, adequate nutrients, and appropriate caloric intake ensures optimal heart and vascular function, and supports the body’s intricate transport system for oxygen and nutrients to every tissue and organ.
The risk factors contributing to cardiovascular diseases can be broadly categorized into two primary groups: modifiable risk factors and non-modifiable risk factors. Modifiable risk factors are those that can be influenced, controlled, or reversed through conscious lifestyle choices, dietary modifications, and health interventions. These factors are often the result of human behavior, lack of awareness, or insufficient knowledge regarding proper health practices. By addressing these modifiable factors, individuals can significantly reduce their susceptibility to conditions such as atherosclerosis and coronary artery disease.
One of the most significant modifiable risk factors is elevated blood cholesterol levels. Cholesterol is a lipid molecule that is essential for the normal functioning of the body; however, excessive cholesterol in the bloodstream can lead to pathological accumulation in the arterial walls, resulting in narrowing and obstruction of blood vessels. In clinical practice, the initial assessment of abnormal cholesterol levels is typically performed through a lipid profile test, which measures total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglyceride concentrations. For adults, a total cholesterol level in the range of 200 to 250 mg/dL is generally considered within the borderline limit. Levels above 200 mg/dL require careful monitoring and lifestyle management, while levels exceeding 250 mg/dL indicate a higher risk for the development of cardiovascular complications.

Symptoms associated with high cholesterol levels often manifest subtly at first. Individuals may experience mild breathlessness, heaviness in the chest, dizziness, or occasional fatigue. These early warning signs should not be ignored, as they indicate that the myocardial blood flow may be compromised due to partial obstruction in the coronary arteries. If high cholesterol is not managed effectively, it can progress to severe conditions such as myocardial ischemia, angina pectoris, or even acute coronary syndromes. Importantly, elevated cholesterol levels can often be controlled naturally through lifestyle interventions, including a balanced diet, regular physical activity, stress management, and targeted naturopathic therapies. With consistent adherence to these modifications, improvements in total cholesterol, triglyceride levels, and the HDL-to-LDL ratio can generally be observed within approximately 60 days.
Another critical modifiable risk factor is cigarette smoking, which remains one of the leading causes of preventable cardiovascular disease globally. Tobacco smoke contains a complex mixture of chemicals, including nicotine, carbon monoxide, and reactive oxidative species, which collectively contribute to endothelial dysfunction, vascular inflammation, and accelerated atherosclerotic plaque formation. The chemical constituents of tobacco not only impair arterial elasticity but also promote narrowing of the ventricular and arterial lumens, thereby obstructing normal blood flow and increasing the workload on the myocardium. Prolonged exposure to cigarette smoke significantly elevates the risk of coronary artery disease, myocardial infarction, and other vascular complications, making cessation of smoking one of the most impactful preventive measures for maintaining heart health.
Management of these modifiable risk factors emphasizes the importance of early detection and proactive intervention. Routine medical tests, such as lipid profiles or other pathology reports, should be performed in response to noticeable symptoms rather than indiscriminately at fixed intervals. Informed decision-making based on accurate diagnostic data, combined with lifestyle adjustments, can often prevent the progression of chronic cardiovascular conditions without immediate reliance on pharmacological interventions. Awareness of bodily signals, adherence to a nutrient-rich diet, avoidance of harmful habits such as smoking, and engagement in regular physical activity collectively constitute a comprehensive approach for mitigating the effects of elevated cholesterol levels and tobacco exposure on cardiovascular health.
Cigarette smoking represents a major modifiable risk factor for cardiovascular disease due to its direct impact on the lungs and the circulatory system. During the act of inhalation, the lungs expand to their maximal capacity, and with each exhalation, the lungs contract, creating a cycle of expansion and relaxation. However, when a person smokes, this process introduces a significant amount of harmful substances, including carbon monoxide, tar, and other chemical compounds, into the pulmonary system. These substances impair the efficiency of oxygen exchange within the alveoli, reduce oxygen saturation in the bloodstream, and contribute to endothelial dysfunction, which promotes the formation of atherosclerotic plaques. The accumulation of these toxic compounds obstructs normal blood circulation, increases arterial blockages, and decreases the oxygen content of blood, thereby imposing additional strain on the myocardium. For habitual smokers, immediate cessation is often challenging; therefore, a gradual reduction in cigarette consumption is recommended. For example, individuals who consume ten cigarettes per day may initially reduce their intake to two or three cigarettes, progressively working toward complete cessation over time. Support systems, including rehabilitation centers, counseling, and family encouragement, play a crucial role in assisting individuals to discontinue smoking and restore cardiovascular health.
Similarly, alcohol consumption is another significant modifiable risk factor for heart disease. Alcohol has a deleterious effect on the cardiovascular system, contributing to hypertension, arrhythmias, and myocardial damage. While some misconceptions persist regarding the cardioprotective effects of red wine, it is important to clarify that no form of alcohol is inherently beneficial for heart health. Gradual reduction of alcohol intake, and, if necessary, substituting more harmful alcoholic beverages with red wine temporarily, can reduce cardiovascular risk. Long-term cessation or significant reduction of alcohol consumption relies on individual willpower, patience, and external support from healthcare providers and family members.
Hypertension, dyslipidemia, and uncontrolled blood glucose levels are widely recognized as the “silent killers” of modern cardiovascular health. These conditions, often categorized as lifestyle-related diseases, are prevalent from young adulthood through older age, and continue to impact individuals even post-menopause in females. Elevated blood pressure, high cholesterol levels, and poorly controlled diabetes represent the principal modifiable risk factors that significantly increase the likelihood of developing coronary artery disease, myocardial infarction, and other cardiovascular complications. Management of these conditions begins with early detection and active monitoring. While pharmacological interventions such as antihypertensive medications, lipid-lowering agents, and antidiabetic drugs may be necessary in certain cases, lifestyle modification remains a cornerstone of prevention and reversal.
For patients with early-stage hypertension, for instance, physicians often prescribe low-dose medications such as 5 mg to 10 mg of antihypertensive drugs. However, without concurrent lifestyle adjustments, including dietary management, regular physical activity, and stress reduction, the underlying cardiovascular risk may continue to progress. Similarly, uncontrolled blood glucose levels, reflected in HbA1c readings exceeding 7–8%, indicate impaired pancreatic insulin secretion and poor glycemic control, which exacerbates endothelial damage and accelerates atherosclerosis. These metabolic imbalances frequently coexist with elevated lipid profiles, highlighting the interconnected nature of these conditions. Effective management of any one of these risk factors requires simultaneous attention to the others, as they collectively determine the overall health of the cardiovascular system.
In clinical practice, the interrelationship between blood pressure, lipid levels, and blood glucose is particularly critical when surgical interventions are considered. Cardiovascular surgeons often emphasize the need to normalize blood pressure and glycemic control prior to performing procedures, as uncontrolled hypertension or hyperglycemia significantly increases perioperative risk and impairs healing. Therefore, comprehensive management of these primary modifiable risk factors—smoking, alcohol consumption, hypertension, dyslipidemia, and hyperglycemia—is essential not only for the prevention of cardiovascular disease but also for the optimization of outcomes in cases where invasive interventions may be required.
Another significant modifiable risk factor for cardiovascular disease is stress, which is universally present in all individuals to varying degrees. Stress, in its optimal form, can be beneficial, as it promotes alertness, focus, and creativity. It encourages problem-solving, goal achievement, and innovative thinking. Mild to moderate stress stimulates the autonomic nervous system and supports adaptive physiological responses, thereby enhancing productivity and cognitive performance. However, when stress becomes chronic or excessive, it overwhelms the body’s capacity for adaptation, leading to detrimental effects on the cardiovascular system. Prolonged exposure to high stress levels increases sympathetic nervous system activity, elevates circulating catecholamines, and results in sustained hypertension, endothelial dysfunction, and increased risk of atherosclerotic plaque formation.
Effective management of stress requires the ability to recognize its onset and implement personalized coping strategies. Since individuals have different stress thresholds and responses, stress management techniques must be tailored to each person’s preferences and lifestyle. Recreational activities such as dancing or listening to music can serve as effective mechanisms to divert and reduce excessive stress. Engaging in these activities for 25 to 30 minutes has been shown to induce relaxation, decrease sympathetic nervous system overactivation, and restore homeostasis. Similarly, social interactions, spending time with family, and other pleasurable activities, including moderate shopping or massage therapies, can act as natural stress mitigators by promoting parasympathetic activation and muscular relaxation.
It is crucial to heed the physiological signals of stress and fatigue. Ignoring signs such as prolonged exhaustion, sleep deprivation, or persistent muscle tension may increase the risk of acute cardiovascular events, including myocardial infarction. Awareness of one’s physical and mental state, and timely interventions to alleviate stress, constitute essential preventive measures for maintaining cardiac health.
Another modifiable risk factor is obesity, which significantly impacts both physical and mental health. Excess adiposity, particularly central or visceral obesity, is strongly associated with hypertension, dyslipidemia, insulin resistance, and systemic inflammation—all of which are key contributors to cardiovascular disease. Obesity imposes additional workload on the myocardium, leading to increased cardiac output requirements, left ventricular hypertrophy, and higher risk of heart failure over time. In addition to its physiological effects, obesity negatively affects psychological well-being. Individuals, especially adolescents and young adults, may experience decreased self-esteem, social stigmatization, and lowered confidence levels, which can exacerbate stress and further contribute to metabolic dysregulation.
Management of obesity involves a combination of dietary modification, regular physical activity, and behavioral interventions. Weight reduction, even by a modest percentage of total body weight, can significantly improve lipid profiles, reduce blood pressure, enhance insulin sensitivity, and lower systemic inflammation. Simultaneously, improving body composition positively affects mental health by boosting confidence, reducing anxiety, and enhancing overall quality of life. Therefore, obesity represents a critical modifiable risk factor whose management is essential for comprehensive cardiovascular disease prevention.
Obesity and Weight Management as Modifiable Risk Factors for Cardiovascular Health
Excessive weight gain serves as a critical early warning sign of potential health complications and must be recognized as an alert from the body indicating the need for intervention. Gradual accumulation of body fat, if left unaddressed, can become entrenched and particularly difficult to reduce over time. Many individuals, despite awareness of their overweight status, delay initiating corrective measures, resulting in long-term retention of adipose tissue, which is metabolically active and contributes to increased cardiovascular risk. Stubborn fat deposits, once established, pose significant challenges to weight reduction, even with strict dietary regimens, pharmacological interventions, or regular physical activity. Observations from clinical naturopathy indicate that delayed intervention often results in repeated cycles of ineffective weight management, reinforcing the importance of early recognition and consistent action.
Obesity affects both physical and mental health. Physiologically, excess adiposity is associated with increased myocardial workload, elevated blood pressure, dyslipidemia, insulin resistance, and systemic inflammation, all of which contribute to the development of cardiovascular disease. Psychologically, obesity can negatively impact self-esteem, confidence, and social interactions, particularly among adolescents and young adults. These combined effects exacerbate the challenges of sustained weight management, as mental and physical health are deeply interconnected.
Effective weight management begins with awareness and early intervention. Individuals must monitor body weight regularly and implement corrective strategies as soon as an upward trend is detected. Neglecting early signs often results in the progression of obesity to a stage where fat reduction becomes significantly more challenging. Strategies for intervention include identifying the root cause of weight gain, whether it is related to dietary habits, physical inactivity, metabolic disorders, or other health conditions, and addressing these factors specifically. Targeted interventions may include structured exercise programs, dietary modification, stress management, and correction of underlying medical conditions that contribute to weight gain.
Maintaining weight loss is frequently more challenging than achieving initial reduction. Clinical experience over eighteen years in naturopathic practice demonstrates that individuals who achieve successful weight loss often experience weight regain if they fail to sustain lifestyle modifications over time. Long-term maintenance requires adherence to dietary consistency, regular physical activity, and ongoing monitoring of body weight and metabolic parameters. It is imperative to prioritize health alongside professional and financial responsibilities, as optimal physical health forms the foundation for all other aspects of life. Financial resources, professional success, and social status cannot compensate for compromised physiological function. The human body, as a complex biological structure, requires consistent care and attention to preserve systemic homeostasis.
Even brief daily interventions, such as 20 to 25 minutes dedicated to physical activity, deep breathing exercises, or mindful observation of physiological signals, can significantly enhance cardiovascular and overall health. These practices support circulatory efficiency, enhance metabolic function, and contribute to mental well-being. Sedentary behavior, often justified by occupational demands or busy lifestyles, is a major contributor to obesity and cardiovascular risk. Physical inactivity exacerbates metabolic dysfunction, including reduced insulin sensitivity and impaired lipid metabolism, further increasing the risk of atherosclerosis and related complications.
In addition, deficiencies in essential nutrients, such as vitamin D and vitamin B12, are increasingly observed even in regions with abundant sunlight, such as parts of Asia. Despite consistent solar exposure, modern lifestyle factors, including limited outdoor activity, protective clothing, and indoor-centric routines, contribute to inadequate synthesis and absorption of these critical nutrients. Vitamin D deficiency negatively impacts calcium metabolism, bone health, and immune function, while vitamin B12 deficiency can impair red blood cell formation and contribute to neurological dysfunction. These nutritional deficiencies further compound the physiological challenges associated with obesity and cardiovascular disease, emphasizing the importance of holistic lifestyle management, including adequate sun exposure, balanced nutrition, and targeted supplementation when necessary.
Non-Modifiable Risk Factors for Cardiovascular Disease
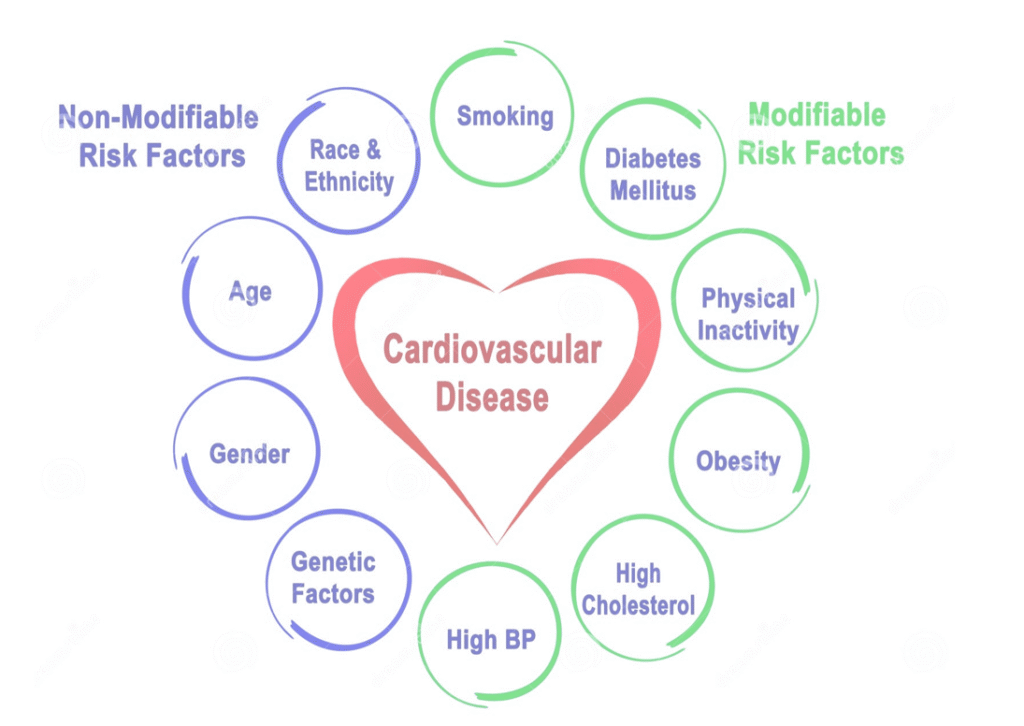
In addition to modifiable risk factors such as obesity, sedentary lifestyle, stress, smoking, and dietary imbalances, there exist several non-modifiable risk factors that inherently influence cardiovascular health and cannot be directly altered through lifestyle changes or naturopathic interventions. Understanding these factors is crucial for risk assessment, early detection, and preventive strategies aimed at mitigating long-term cardiac complications.
One of the most significant non-modifiable risk factors is family history of cardiovascular disease. Epidemiological data indicate that genetic predisposition plays a substantial role in determining individual susceptibility to coronary artery disease, myocardial infarction, and other heart-related disorders. Studies have shown that in approximately 90% of cases, cardiovascular conditions are observed to recur across successive generations within families. Individuals with a positive family history are at a heightened risk of developing similar conditions. While genetic predisposition cannot be altered, awareness of familial health patterns allows for targeted preventive strategies. Early interventions, such as regular monitoring of lipid profiles, blood pressure, and glucose levels, coupled with proactive lifestyle modifications, may reduce the likelihood of disease manifestation in both the individual and future generations. In the context of pre-marital health assessments, particularly in arranged marriages, obtaining detailed family health histories and current medical evaluations can guide precautionary measures and inform lifestyle adjustments to minimize hereditary risk without restricting personal or social choices.
Aging represents another prominent non-modifiable risk factor. Chronological age is intrinsically associated with progressive structural and functional changes in the cardiovascular system, including arterial stiffening, reduced endothelial function, and decreased myocardial compliance. However, the negative impact of aging can be mitigated through lifelong engagement in physical activity, maintenance of muscular strength, and adherence to a balanced diet. Numerous examples, including senior athletes participating in competitive events well into their 60s, 70s, and even 90s, demonstrate that consistent lifestyle practices can preserve cardiovascular function and overall physiological resilience. Aging, therefore, should be recognized as an inevitable chronological process, but its functional consequences can be substantially delayed through awareness and proactive health management.
Gender also influences cardiovascular risk profiles. Epidemiological evidence consistently indicates that men are at higher risk of developing coronary artery disease and experiencing acute myocardial events at earlier ages compared to premenopausal women. This disparity is partially attributed to the cardioprotective effects of female sex hormones, including estrogen and progesterone, which enhance endothelial function, improve lipid metabolism, and provide anti-inflammatory benefits. Postmenopausal women, typically over the age of 45–50 years, experience a decline in these protective hormones, resulting in increased vulnerability to cardiovascular disease. Hormonal changes during the perimenopausal and postmenopausal periods, including reduced estrogen levels, contribute to vascular stiffness, altered lipid profiles, and calcium metabolism disturbances, further elevating cardiovascular risk. Consequently, postmenopausal women require heightened vigilance, including routine cardiovascular monitoring, dietary adjustments, and lifestyle interventions to mitigate these age- and hormone-related risks.
Sex-specific variations in cardiovascular disease manifestation are further influenced by behavioral, cultural, and physiological factors. While men may exhibit higher prevalence of early-onset heart disease, women, particularly after menopause, experience a gradual convergence in risk levels due to the decline of endogenous hormonal protection. These differences underscore the importance of personalized preventive strategies based on age, gender, and individual health history, emphasizing proactive measures even in the presence of non-modifiable risk factors.
Overall, while non-modifiable factors such as family history, aging, and gender cannot be changed, awareness of these determinants enables targeted risk reduction through lifestyle modifications, early screening, and preventive interventions. Individuals equipped with this knowledge can implement adaptive strategies to reduce cardiovascular burden and improve long-term health outcomes, demonstrating that while certain risks are inherent, their physiological impact can be mitigated through informed and proactive management.
Advanced Insights into Heart Health: Mind-Body-Food Connection, Silent Symptoms, and Clinical Indicators
Modern scientific research has increasingly demonstrated the intricate connections between the mind, body, and nutrition, emphasizing that emotional and psychological states can significantly influence cardiovascular health. While it is not compulsory to actively manage every emotional response, practices such as emotional release—through crying, meditation, or relaxation techniques—can help reduce psychological burden, alleviate stress, and indirectly contribute to improved heart function. These practices exemplify the broader principle that the autonomic nervous system, stress hormone regulation, and emotional well-being are intricately linked with cardiac health.
Certain autoimmune and degenerative disorders also contribute to non-modifiable cardiovascular risks. Common autoimmune conditions, including rheumatoid arthritis, systemic lupus erythematosus, and autoimmune-related osteoporosis, may induce chronic systemic inflammation, which over time can adversely affect vascular integrity, myocardial function, and overall circulatory efficiency. Similarly, chronic DNA imbalances or genetic mutations, while inherently unmodifiable, may predispose individuals to cardiac anomalies. Awareness of these conditions and early monitoring may provide opportunities for preventive interventions, although complete reversal is beyond current clinical capabilities.
Silent symptoms of cardiovascular disease present a unique challenge in early detection. Many manifestations are subclinical and may not be immediately detectable through standard diagnostic tests such as lipid profiling, glucose assessment, or blood pressure measurements. Individuals who maintain regular health checkups may still experience acute events, such as sudden cardiac arrest or angina, due to underlying molecular, genetic, or stress-related imbalances not measured by conventional tools. Therefore, subjective bodily signals must be recognized and interpreted carefully, as the body often communicates early warnings of cardiovascular compromise through subtle indicators.
One significant clinical manifestation is myocardial ischemia, defined as an inadequate blood supply to the heart muscle. This condition may present during physical exertion or stress as transient stiffness or discomfort in the chest, shoulders, or jaw. These episodes, although brief, indicate localized hypoperfusion of the myocardium and warrant further evaluation. Notably, chest pain and angina symptoms are not exclusively cardiac in origin. Clinical studies have shown that approximately 20–30% of chest pain cases may result from gastrointestinal disturbances, such as severe constipation or dyspepsia, rather than true cardiac ischemia. Hence, differential diagnosis is critical to accurately identify the underlying cause.
Dyspnea, or difficulty in breathing, represents another important early warning symptom of cardiovascular compromise. Even in the absence of overt exertion, individuals experiencing irregular or labored breathing may be demonstrating signs of inadequate cardiac output, requiring immediate assessment. Similarly, arrhythmias, characterized by irregular or abnormal heart rhythms, can indicate disturbances in myocardial electrical conduction. Patients may experience tachycardia, bradycardia, or intermittent palpitations, all of which are detectable through electrocardiography (ECG). The ECG remains a pivotal diagnostic tool, allowing clinicians to identify deviations in cardiac electrical activity that may signal underlying structural or functional abnormalities.

n addition to functional assessments, biochemical markers such as elevated cardiac enzymes serve as critical indicators of myocardial stress or injury. Enzymes including troponins and creatine kinase-MB are released during myocardial damage, providing quantifiable evidence of cardiac dysfunction. Abnormal elevations of these enzymes, while essential for protective and repair mechanisms, can also reflect pathological stress on the heart when chronically elevated.
Another clinical manifestation, diaphoresis, or excessive sweating, may occur as a result of autonomic dysregulation, medication side effects, or acute cardiac stress. Persistent or unexplained diaphoresis, particularly when accompanied by chest discomfort or dyspnea, may signify a cardiovascular event requiring immediate medical evaluation.
Understanding these physiological and biochemical indicators, along with recognition of silent symptoms and lifestyle-related risk factors, is essential for comprehensive cardiovascular risk assessment. Awareness of the mind-body-food nexus, the impact of chronic autoimmune conditions, and the interpretation of early clinical signs enables proactive management of heart health, improving both short-term function and long-term outcomes.
Clinical Manifestations, Risk Awareness, and Preventive Measures in Cardiovascular Health
Diaphoresis—excessive sweating—is an important clinical manifestation that may indicate underlying cardiovascular stress or dysfunction. For instance, an individual may experience sudden profuse sweating even while sitting in an air-conditioned room, with complete saturation of clothing. Diaphoresis can occur naturally under certain physiological conditions or as a side effect of specific pharmacological agents, including cardiovascular medications. While it is a symptom rather than a direct cause, its presence can provide critical diagnostic clues for identifying potential cardiac compromise.
Chest pain, commonly referred to as angina, represents a hallmark symptom of myocardial ischemia. Angina is characterized by transient discomfort or pressure in the chest, often radiating to the shoulder, jaw, or arm, and results from insufficient myocardial perfusion. It is important to differentiate true angina from musculoskeletal or gastrointestinal causes, as studies indicate that approximately 20–30% of patients presenting with chest discomfort may be experiencing symptoms secondary to digestive disturbances, such as constipation or dyspepsia, rather than cardiac ischemia. Accurate clinical assessment and diagnostic evaluation are therefore essential to determine the etiology of chest pain.

Complications associated with inadequate myocardial perfusion include acute coronary syndromes, heart failure, and sudden cardiac death. Insufficient oxygenated blood supply can precipitate irreversible myocardial injury, resulting in severe pain, respiratory difficulty, and impaired mobility during acute episodes. In high-profile cases, such as sudden collapses during physical activity or exercise, immediate cardiovascular failure can occur due to an acute mismatch between myocardial oxygen demand and supply. While emergency intervention may be lifesaving if timely, sudden cardiac death often occurs without prior detectable warning signs, even in physically active and ostensibly healthy individuals. This unpredictability underscores the necessity of proactive monitoring and preventive strategies.
Self-assessment and physical examination remain critical initial steps for cardiovascular risk management. Individuals exhibiting obesity or overweight conditions should recognize the associated systemic burden, as excessive adipose tissue can impede circulatory efficiency, compromise vascular function, and strain cardiac workload. Weight management, including reduction of excess fat and promotion of lean muscle mass, is therefore integral to mitigating cardiovascular risk.
Exercise and physical activity are fundamental components of preventive cardiac health. Even in fast-paced modern lifestyles, allocating a minimum of 20 minutes daily for structured exercise is essential for maintaining circulatory and muscular integrity. Walking, while beneficial, must be performed with mindful concentration on both steps and respiratory rhythm to achieve optimal cardiovascular engagement. Merely performing incidental walking during routine activities, such as grocery shopping, does not suffice for physiological conditioning. Proper footwear, posture, and focused engagement enhance the effectiveness of walking as a cardiovascular exercise.
Comprehensive muscular engagement cannot be achieved through walking alone. The human body comprises numerous small muscle groups, including core and distal muscles in the fingers and joints, which require targeted activity for sustained strength and flexibility. Although it may not be feasible to exercise every muscle group daily due to age, comorbidities, or physical limitations, integrating diverse forms of exercise and deep breathing techniques ensures holistic stimulation of the musculoskeletal and circulatory systems. These activities support not only cardiovascular efficiency but also overall physical resilience.
In summary, recognition of clinical manifestations such as diaphoresis and angina, combined with proactive lifestyle modifications—including structured exercise, weight management, and conscious engagement of muscular and respiratory systems—forms a critical foundation for maintaining cardiovascular health and preventing acute and chronic complications. Early awareness and consistent preventive measures significantly enhance the body’s capacity to adapt to physiological stressors and reduce the risk of sudden cardiac events.
Self-Examination, Diagnostic Evaluation, and Lifestyle-Based Naturopathic Management of Cardiovascular Health
Establishing consistent daily habits aimed at maintaining cardiovascular health is essential for both prevention and management of heart disease. Gradual incorporation of positive lifestyle modifications, such as reduction of cigarette smoking or alcohol consumption, can significantly lower cardiovascular risk. For individuals who continue to smoke, a stepwise reduction strategy is recommended, while those with excessive alcohol intake should progressively limit their consumption to minimal or moderate levels. Regular monitoring of physiological parameters, such as
respiratory efficiency and blood pressure, constitutes an important component of self-examination and early detection.
Respiratory self-assessment can provide critical insights into cardiovascular and pulmonary function. Irregular breathing patterns, including a disproportionate duration of inspiration relative to expiration, may indicate compromised cardiac output or pulmonary inefficiency. Balanced respiratory timing, as achieved through controlled breathing exercises, particularly box breathing techniques, enhances oxygen delivery, reduces cardiac workload, and promotes autonomic nervous system equilibrium.
Family history assessment is a fundamental component of cardiovascular risk stratification. Hereditary predispositions for heart disease, passed from one generation to the next, necessitate heightened vigilance. Comprehensive evaluation of family health histories allows for the identification of genetic risk factors, enabling early intervention and preventive strategies, particularly prior to critical life events, such as marriage or family planning. Awareness of familial patterns facilitates informed lifestyle choices that may reduce the likelihood of inherited cardiovascular complications.
Upon identification of potential risk factors or the manifestation of symptoms, clinical evaluation is initiated through standard diagnostic tests. Initial laboratory investigations typically include complete blood count (CBC), creatine kinase myocardial band (CK-MB), lipid profile, blood glucose levels, HbA1c, and C-reactive protein (CRP) assessments. Lipid profiling detects dyslipidemia, including elevated low-density lipoprotein (LDL) and triglycerides, as well as low high-density lipoprotein (HDL), while HbA1c measurement provides an indication of long-term glycemic control and pancreatic beta-cell function. Elevated CRP levels may signal systemic inflammation, including cardiovascular inflammation, which can contribute to atherosclerosis.
Following laboratory evaluation, cardiac functional assessment is typically performed through electrocardiogram (ECG) testing to detect arrhythmias, myocardial ischemia, or conduction abnormalities. Advanced imaging modalities, including echocardiography, coronary angiography, stress testing, positron emission tomography (PET), magnetic resonance imaging (MRI), and Doppler ultrasonography, provide detailed insights into myocardial structure, perfusion, and vascular integrity. While certain diagnostic procedures, such as blood tests and ECG, may be facilitated under naturopathic supervision, imaging and invasive investigations require specialist oversight.
Naturopathic intervention in cardiovascular management focuses on addressing contributory lifestyle and systemic factors prior to direct cardiac therapy. Primary targets include normalization of blood pressure, glycemic control, and lipid profile optimization. Therapeutic strategies are designed to lower LDL cholesterol, regulate triglyceride levels, and improve HDL concentrations. For patients presenting with obesity, structured exercise programs and dietary modifications are prescribed to achieve gradual weight reduction, thereby reducing vascular strain and improving metabolic efficiency.
Clinical observations indicate that effective management of these systemic factors can alleviate approximately 50% of the cardiac workload, reducing arterial stress and normalizing hemodynamic parameters. Consequently, common cardiovascular symptoms, such as dyspnea, insomnia, and episodic chest discomfort, frequently demonstrate marked improvement once underlying lifestyle-related conditions are addressed.
Lifestyle modifications constitute the cornerstone of preventive and therapeutic strategies in naturopathy. These encompass the adoption of consistent daily routines, sleep hygiene, punctuality, and structured scheduling. Excessive screen time, a prevalent modern risk factor, contributes to sleep disturbances, particularly insomnia, through interference with natural circadian rhythms and perturbation of electrolytic balance. It is therefore recommended to limit exposure to electronic devices at least thirty minutes prior to sleep to mitigate adverse effects on cardiac and neurological function.
By integrating self-monitoring, structured diagnostic evaluation, and targeted lifestyle modifications, naturopathic interventions aim to restore systemic balance, reduce cardiovascular risk, and enhance overall physiological resilience. The emphasis on early detection, habitual regulation, and individualized intervention underscores the proactive and preventive orientation of naturopathic cardiovascular care.
Lifestyle, Nutrition, and Naturopathic Interventions for Cardiovascular and Systemic Health
In contemporary society, lifestyle patterns exert a profound influence on cardiovascular health, metabolic balance, and overall systemic well-being. Excessive exposure to electronic devices, including computers, laptops, and mobile phones, particularly during late hours, has been identified as a significant factor contributing to sleep disturbances, circadian rhythm dysregulation, and heightened stress levels. Therefore, it is recommended to discontinue the use of all electronic gadgets at least thirty minutes prior to bedtime. Establishing fixed sleep and wake-up times, as well as regulated meal schedules, constitutes the foundation of lifestyle modification, which has been consistently demonstrated to have a more substantial impact on health outcomes than pharmacological interventions alone.
Nutritional practices play a critical role in maintaining cardiovascular and metabolic health. Modern dietary patterns often include a wide variety of international cuisines, such as Japanese, Korean, and Chinese foods. While occasional consumption for taste enhancement is acceptable, habitual incorporation of non-traditional foods may disrupt digestive function and metabolic efficiency, particularly when consumed in excess or when inconsistent with an individual’s physiological constitution. It is therefore advisable to prioritize traditional, region-specific, and seasonal foods, which align with the natural climatic conditions, soil composition, and local agricultural produce. For example, in northern regions of India, heavier meals are appropriate due to the colder climate, whereas southern diets are rich in rice and coconut to match the warmer, humid environment. Seasonal fruits, leafy vegetables, and root vegetables, which are abundant during specific periods of the year, should form the primary dietary intake to optimize nutrient absorption, digestive function, and overall health.
Macronutrient balance is equally crucial. High-protein dietary regimens, often promoted in gym and fitness cultures, should respect individual dietary habits. Vegetarians can obtain adequate protein from plant-based sources without introducing non-vegetarian foods, which may disrupt digestion and metabolic processes. Conversely, non-vegetarians should adhere to protein sources compatible with their digestive capabilities to maintain homeostasis.
Physical activity and relaxation practices are integral components of naturopathic health management. Regular engagement in yoga, pranayama, aerobic exercise, and walking enhances cardiovascular function, muscular strength, and stress resilience. Adequate sleep, typically six to eight hours per night, serves as a natural stress regulator by promoting the secretion of neurotransmitters such as dopamine and serotonin, which are essential for maintaining mood stability, cognitive function, and systemic homeostasis. Disruption of the circadian rhythm through irregular sleep patterns impairs physiological repair mechanisms and increases susceptibility to cardiovascular and metabolic disorders.
Naturopathic therapeutic interventions focus on enhancing circulation, eliminating toxins, and optimizing organ function. Hot and cold hydrotherapy applied to the feet for ten minutes each stimulates reverse circulation through the venous and capillary networks, thereby supporting efficient blood flow and oxygen delivery throughout the body. Enema therapy, administered with warm water over three to five days monthly, facilitates detoxification by promoting bowel clearance, enhancing digestive efficiency, and maintaining optimal metabolic function, while avoiding excessive frequency to preserve normal peristaltic activity.
Massage therapy, excluding the chest area, is recommended every fifteen to twenty days to promote muscular contraction and relaxation, improve circulation, and reduce systemic stress. Post-massage steam therapy further facilitates the elimination of metabolic waste through sweating, thereby alleviating renal and hepatic burdens, enhancing detoxification pathways, and supporting overall organ function. These interventions collectively restore systemic equilibrium, optimize cardiovascular performance, and reduce the cumulative stress load on critical organs.
By integrating structured lifestyle adjustments, regionally and seasonally appropriate nutrition, consistent physical activity, and targeted naturopathic therapies, individuals can achieve measurable improvements in cardiovascular health, metabolic regulation, and general physiological resilience.
Naturopathic Approaches for Cardiovascular, Renal, and Systemic Health Management
The liver is recognized as the principal chemical factory of the human body, responsible for the synthesis and regulation of multiple enzymes and hormones, as well as the production of bile, which plays a critical role in lipid digestion and metabolic detoxification. Naturopathic interventions, including therapeutic massage, serve to enhance the functional activity of the liver and other organ systems by promoting circulatory efficiency and stimulating enzymatic secretions. Specifically, massage applied to the extremities can influence systemic organ activation, thereby supporting overall metabolic homeostasis.
A traditional therapeutic approach, magnet therapy of the feet, has been historically practiced in domestic settings and is incorporated in naturopathic protocols at centers such as Saffron. This therapy involves the application of magnetic energy through a carrier medium, commonly clarified butter or ghee, applied to the soles of the feet. Ghee facilitates the conduction of magnetic energy and provides nourishment to the skin and underlying tissues. Daily application, for approximately five minutes per foot prior to bedtime, can optimize autonomic function, enhance circulation, and stimulate systemic detoxification processes. The night-time period represents the critical window for endogenous repair, regeneration, and detoxification, during which autonomic organs continue physiological activity even while voluntary muscles are at rest. Regular foot massage during this period can improve energy levels upon awakening, enhance vascular perfusion, prevent constipation and digestive irregularities, and contribute to the maintenance of restorative sleep cycles.
Herbal interventions play a complementary role in cardiovascular and systemic health. Terminalia arjuna (commonly referred to as Arjun chal) is a well-documented cardiotonic herb that strengthens myocardial function, supports arterial health, and aids in the management of elevated cholesterol and angina. The herb can be administered as a decoction prepared by boiling fresh bark or as a powder soaked overnight in water and consumed on an empty stomach in the morning. Regular administration of Arjuna has been shown to improve myocardial contractility, enhance coronary circulation, and reduce oxidative stress within cardiac tissues.
Tinospora cordifolia (Amrita or Giloy) is utilized for its immunomodulatory and hematopoietic properties, serving as a blood purifier and supporting overall immune resilience. Wheatgrass (Triticum aestivum), rich in chlorophyll and micronutrients, provides antioxidative and detoxifying effects, contributing to the maintenance of systemic metabolic balance and cardiovascular protection. The recommended daily intake of fresh wheatgrass juice is approximately 40 grams, though powdered and tablet forms are available when fresh sources are inaccessible.
Medicago sativa (Alfalfa or Alpha-alpha) is another nutrient-dense herb, abundant in calcium, vitamins, and trace minerals, supporting bone health, cardiovascular function, and metabolic homeostasis. Butea superba (Puna nava) promotes cellular regeneration and tissue repair, providing additional support to cardiovascular and systemic integrity. A combination of two to three herbs may be prescribed simultaneously, tailored to individual age, symptomatology, and comorbid conditions, with observed synergistic effects when combined with lifestyle modifications, exercise, and dietary management.
In cases of patients presenting with comorbid conditions, such as diabetes, cardiovascular disease, and pulmonary fluid retention, naturopathic protocols emphasize integrative management. Initial objectives include glycemic control and pulmonary health optimization, which involves reducing fluid accumulation in the lungs and improving respiratory efficiency. Herbs such as Arjuna, wheatgrass, Alpha-alpha, and Giloy can be employed concurrently to enhance cardiac function, support renal health, and improve systemic oxygenation.

Patients receiving concurrent diuretic therapy may exhibit polyuria, lower extremity edema, and elevated creatinine levels, indicative of compromised nephron function. In such scenarios, herbal interventions must be carefully monitored to avoid exacerbating fluid imbalance while supporting renal and cardiovascular function. Naturopathic management focuses on optimizing systemic circulation, maintaining electrolyte balance, reducing vascular load, and supporting detoxification pathways through a combination of diet, herbal supplementation, and physical therapies.
Through systematic application of these naturopathic interventions—comprising foot magnet therapy, herbal cardiotonics, detoxifying herbs, dietary modulation, and lifestyle optimization—patients demonstrate measurable improvements in cardiac efficiency, renal function, circulatory health, and overall physiological resilience, providing a comprehensive framework for integrative management of complex cardiovascular and systemic conditions.
Naturopathic Strategies for Cardiovascular, Renal, and Gastrointestinal Health Management
In the management of patients with cardiovascular and renal complications, it is critical to recognize that initial pharmacological interventions, such as diuretics and laxatives, cannot be discontinued abruptly. These medications are often prescribed to manage excessive fluid retention and systemic inflammation, conditions which impose a substantial burden on both cardiac and renal systems. Naturopathic interventions, however, can provide complementary support aimed at gradually reducing reliance on these pharmacological agents. For instance, the administration of Puna nava in conjunction with wheatgrass has demonstrated potential to enhance renal function, support diuresis naturally, and reduce cardiovascular stress, thereby contributing to the potential tapering of diuretic therapy under medical supervision.
At Saffron, a variety of formulations of these herbs are available, including fresh, powdered, and tablet forms, allowing for flexibility in therapeutic application based on patient preference and clinical requirements. The typical dosage for powdered herbal preparations, including Puna nava, Amrita (Giloy), and Arjuna (Arjun chal), ranges from one to two tablespoons twice daily, administered with hot water or as decoctions, depending on the specific herb and patient tolerance. For Arjuna chal, it is recommended that the powder be soaked overnight and consumed in the morning on an empty stomach to maximize myocardial protective effects. Alpha-alpha (alfalfa) can be consumed directly or prepared as a decoction for enhanced nutrient bioavailability.
In patients with coexisting diabetes, lifestyle modifications targeting pancreatic function are essential. Optimizing glycemic control through dietary regulation, physical activity, and stress management not only improves metabolic homeostasis but also reduces the systemic burden on the cardiovascular system. By addressing the primary metabolic disorder, secondary complications such as hypertension, dyslipidemia, and cardiac strain can be mitigated, thus enhancing overall therapeutic outcomes.
Gastrointestinal health forms a foundational component of naturopathic therapy, as effective digestion, elimination, and detoxification are prerequisites for systemic recovery. For patients experiencing constipation or digestive dysfunction, the priority of treatment is to restore bowel regularity and cleanse the gastrointestinal tract. Enema therapy is a highly effective intervention for this purpose, facilitating the removal of accumulated toxins and improving bowel motility. In instances where patients cannot adhere to fasting protocols or extended liquid diets, dietary modifications including increased fiber intake, adequate hydration, and the inclusion of easily digestible, nutrient-dense foods are recommended. Mono diets or specialized liquid diets may also be employed for diabetic patients to support controlled detoxification without compromising glycemic stability.
Herbal therapies further support gastrointestinal and systemic detoxification. Puna nava promotes cellular regeneration and supports renal clearance, while wheatgrass contributes to blood purification and antioxidative activity. Amrita (Giloy) enhances immune resilience and supports hepatic detoxification. These herbs, when administered according to individualized treatment plans, work synergistically with lifestyle modifications to restore homeostasis in cardiovascular, renal, and gastrointestinal systems.
The sequencing of interventions is critical in naturopathic practice. Priority is always given to the organ systems most burdened or at risk, often beginning with gastrointestinal cleansing, followed by the stabilization of metabolic parameters such as blood glucose, lipid profile, and blood pressure. Once these foundational systems are optimized, supportive therapies targeting cardiovascular efficiency, renal function, and systemic detoxification can be implemented more effectively. Such a structured approach ensures that therapeutic outcomes are maximized while minimizing potential adverse interactions with ongoing pharmacological treatments.
Naturopathic Approaches to Detoxification and Cardiovascular Health Management
Detoxification forms a fundamental component of naturopathic treatment, particularly for patients with cardiovascular, renal, digestive, or metabolic imbalances. Detox waters and herbal infusions are commonly prescribed based on the patient’s age, physiological sensitivity, and underlying conditions. For example, Amrita (Giloy) juice and Aloe vera juice are effective for general detoxification, supporting liver and renal function while improving immunity. In diabetic patients, carefully formulated detox waters can help maintain glycemic balance, whereas for individuals with thyroid or hormonal imbalances, herbal waters such as coriander and cumin infusion provide systemic detoxification and aid in regulating metabolic function. For patients unable to prepare these herbal waters, alternatives such as tender coconut water or fresh fruit juices can be provided, offering hydration and mild detoxification support.
While fluid intake through such beverages contributes to detoxification primarily via urinary excretion, complete detoxification necessitates gastrointestinal cleansing, as elimination through bowel movements ensures comprehensive removal of accumulated toxins. Insufficient hydration can compromise mucosal integrity in the gastrointestinal tract, impairing enzymatic activity and reducing the effectiveness of digestive secretions, thereby contributing to constipation and other digestive disorders. Addressing these root causes with appropriate fluids and herbal interventions restores optimal gastrointestinal function and enhances systemic detoxification.
In naturopathic practice, the use of specialized formulations such as SD powder (Stomach Disorder powder) is recommended prior to initiating any therapeutic regimen. This authentic powder facilitates normalization of digestive secretions and supports bowel regularity without inducing habitual dependence or pharmacological side effects. When administered appropriately, SD powder enhances appetite, improves enzymatic function, and optimizes nutrient absorption, providing a strong foundation for subsequent naturopathic therapies.
Alongside herbal supplementation, lifestyle adjustments—including controlled fluid intake, dietary modifications, and regular physical activity—remain central to effective cardiovascular and metabolic health management. These interventions collectively reduce the systemic burden on the heart, kidneys, and liver, mitigate inflammation, and support overall homeostasis.
Conclusion:
Cardiovascular health is influenced by a complex interplay of modifiable and non-modifiable risk factors, including genetic predispositions, autoimmune conditions, DNA imbalances, lifestyle choices, and dietary habits. Silent manifestations such as angina, arrhythmia, inadequate blood supply (ischemia), dyspnea, and elevated cardiac enzymes often precede clinically significant events like myocardial infarction or sudden cardiac death. Early recognition of these symptoms, combined with regular self-monitoring of blood pressure, breathing patterns, and family history, enables timely intervention and risk mitigation.
Diagnostic assessments, including blood tests (CBC, lipid profile, HBA1C, CRP, CK-MB), electrocardiograms, echocardiography, stress tests, coronary angiography, PET scans, and Doppler ultrasonography, are critical for accurately evaluating the extent of cardiovascular compromise. However, alongside these diagnostic tools, naturopathic interventions focus on addressing the root causes of cardiovascular dysfunction by targeting associated metabolic disorders such as hypertension, diabetes, dyslipidemia, obesity, and digestive irregularities.
Lifestyle modification remains the cornerstone of prevention and management, encompassing structured exercise regimens, mindful walking, strength and core training, deep breathing practices such as box breathing, stress management, adequate sleep, and adherence to regionally and seasonally appropriate dietary habits. Proper sleep hygiene, limited screen exposure, and avoidance of smoking and excessive alcohol consumption further optimize systemic homeostasis.
Naturopathic therapies, including herbal interventions (Arjuna, Amrita/Giloy, Wheatgrass, Alpha-Alfa, Puna Nawa), foot magnet therapy with ghee, hydrotherapy (hot and cold foot baths), massages, steam therapy, enema-based detoxification, and specialized digestive powders such as SD powder, facilitate detoxification, improve circulation, enhance enzymatic and hormonal functions, and support organ regeneration. These therapies synergistically reduce systemic inflammation, relieve cardiac and renal burden, improve gastrointestinal clearance, and strengthen cardiac musculature.
By integrating these interventions with careful monitoring, individualized dosage adjustments, and progressive lifestyle changes, patients can achieve significant improvement in cardiovascular function, prevent further complications, and restore overall physiological balance. Naturopathic approaches emphasize not only the treatment of symptoms but also the proactive restoration of health at cellular, organ, and systemic levels, providing a holistic framework for long-term wellness and prevention of coronary, renal, and metabolic disorders.