Dementia and Alzheimer’s
Brain Health and Memory-Boosting Exercises: Preventing Dementia and Alzheimer’s Naturally
Namaskar! Today, we will focus on a topic that is becoming increasingly important in modern times: dementia and Alzheimer’s, both of which are directly related to the health of our brain neurons. Memory-related problems not only affect the elderly but can also impact anyone exposed to modern environmental challenges.
As we know, the brain is a complex organ, and maintaining its health is crucial for overall well-being. Environmental pollution, chemicals, and even reduced oxygen levels in our surroundings can negatively affect our brain functions over time. The good news is that simple brain exercises can help maintain memory and cognitive abilities, and these exercises are not just for people already suffering from brain-related issues—they are for everyone.
The Importance of Brain Exercises
Brain exercises help strengthen coordination between the mind and body, improve memory power, and support healthy neuronal function. Regular practice of these exercises can serve as a preventive measure against memory decline, dementia, and Alzheimer’s in the long run. Moreover, for students and professionals, maintaining a healthy brain enhances focus, learning, and overall cognitive performance.
Today, we will explore two simple yet effective brain exercises. Practicing these for just 2–3 minutes daily can significantly improve brain function and coordination.
Exercise 1: Finger Coordination
This exercise focuses on hand-eye-brain coordination. Begin by using your hands, either right or left, and repeat the numbers in sequence: “one, two, one, two” with both hands. Start slowly to understand the coordination between your brain and fingers. Once comfortable, increase the speed gradually.
Next, switch the order of your fingers: “two, one, two, one.” This small change challenges the brain to adapt, further strengthening neuronal connections. Even spending just two minutes on this simple exercise can create noticeable improvements in coordination, memory, and mental alertness.
Exercise 2: Advanced Palm Exercise
The second exercise is slightly more challenging and involves the palms. It encourages deeper mind-body coordination and enhances focus. While the instructions for this exercise are more advanced, practicing it regularly can amplify memory improvement and cognitive flexibility.
Benefits Beyond Memory
Brain exercises do more than just improve memory. They enhance overall mind-body harmony and are in line with natural healing principles. Natural remedies and practices work holistically—they improve physical health while also supporting emotional, mental, and spiritual well-being. By integrating these exercises into daily life, we not only protect ourselves from future cognitive decline but also promote a more balanced, healthy lifestyle.
These exercises are suitable for people of all ages and can be shared with family, friends, and even patients. Spending just a few minutes daily can create a “miracle” for your brain health over time.
Brain Exercises for Memory and Cognitive Health: A Natural Approach
Brain health and memory function are essential for overall well-being, yet many people overlook simple practices that can significantly improve cognitive abilities. While reflexology and other specialized techniques exist, there are straightforward exercises that anyone can do to strengthen their brain and memory.
The Third Brain Exercise
Building on previous sessions, today we introduce a third brain exercise. The exercise involves finger coordination patterns, such as:
Sequence: 1, 2, 1, 1, 2, 1, 1, 2, 1, 1, 2, 1, 2, 1, 2
This pattern may seem challenging at first, and it is natural to find it difficult to coordinate your fingers with your brain movements in the beginning. However, regular practice over 10–15 days—or even a month—makes it much easier. With consistent effort, this exercise can be taught to others, helping them improve their own cognitive abilities.
Integrating Brain Exercises into Daily Life
Just as we vary our food for taste and nutrition, it is helpful to rotate these brain exercises. You can practice one exercise one day and another the next. Flexibility and personalization in the practice make it easier to continue consistently. The key is regularity—like any skill, mastery comes only with consistent effort.
Observing Results
Students and practitioners who follow these exercises often notice improvements within 15 days to a month. This is particularly relevant for individuals with chronic conditions who may believe that natural therapies take too long to show results. In reality, when diet, therapy, and problem-specific guidance are followed accurately, naturopathic treatments often show effects rapidly.
Sometimes, the body may exhibit mild side symptoms as it eliminates toxins, but these are not side effects—they are signs that the natural healing process is working. These exercises not only support memory and brain function but also align with the holistic principles of naturopathy, which aim to treat the body, mind, and soul together.
Addressing Modern Memory Challenges
A common issue among young people today is overreliance on gadgets and mobile devices, which can weaken memory and cognitive response over time. Simple exercises like these can counteract such effects, improve focus, and enhance coordination between the brain and body. By incorporating these practices into daily life, students, professionals, and individuals of all ages can maintain sharper mental faculties, improved memory, and better overall brain health.
Memory, Technology, and Dementia: Understanding the Modern Brain
In today’s world, our reliance on technology has dramatically changed the way we use our memory. In the past, before the widespread use of mobile phones, people routinely memorized landline numbers—six to eight digits—without difficulty. We were able to recall many numbers effortlessly because our brains were actively engaged in storing and retrieving information.
However, with the advent of smartphones, AI tools, and technologies like ChatGPT, many of us have become reliant on gadgets to remember information. While advanced technology is beneficial and should be embraced, overdependence on it can reduce the natural capacity of our memory. It is crucial to strike a balance: use technology to assist your productivity, but do not neglect the innate abilities that nature has endowed us with. Failing to do so contributes to the increasing prevalence of memory-related problems worldwide.
Understanding Dementia and Alzheimer’s
To understand memory loss and cognitive decline, it is important to define dementia and Alzheimer’s disease. Dementia is a syndrome characterized by multiple cognitive deficits, including disturbances in memory, but without disturbance of consciousness. Alzheimer’s disease is a type of dementia, distinguished by subtle differences but closely related in its impact on cognitive function.
A recent case from my OPD highlights the complexity of dementia. A 73-year-old patient from Gujarat, who had been healthy for most of his life without the need for medication or suffering from lifestyle diseases, was diagnosed with dementia two years ago. Despite his overall good health, he began experiencing memory lapses severe enough that his family felt he could no longer go out alone.
Factors Contributing to Memory Decline
Upon detailed consultation, several contributing factors were identified:
- Irregular Food Patterns: The patient had a history of inconsistent eating due to his demanding work schedule. He often skipped meals or ate at irregular times, which likely affected his overall brain health.
- Loss of Routine and Purpose: After retiring, the patient had to stop his work activities. A lifetime of hard work and creativity left him suddenly idle, which reduced mental stimulation and may have contributed to cognitive decline.
This case illustrates that dementia is not solely caused by medications, lifestyle diseases, or environmental factors. Even individuals with a healthy past lifestyle can experience memory-related issues due to changes in daily routines, nutrition, and mental engagement.
Lessons for Brain Health
Memory and cognitive function can be preserved and even enhanced through conscious daily practices, including brain exercises, a balanced diet, and maintaining an active lifestyle. Avoiding over-reliance on technology and continuing to challenge the brain naturally is essential. Regular mental activity, purposeful routines, and consistent self-care can help prevent or slow down the onset of dementia and other memory-related disorders.
Understanding Dementia and Alzheimer’s: Types, Causes, and Effects on the Brain
Dementia is a cognitive disorder characterized by disturbances in memory while maintaining full consciousness. Unlike conditions that impair awareness, individuals with dementia remain fully aware of their surroundings and can perform daily routines, but they may frequently forget events or tasks. Sudden dementia can sometimes occur due to psychological pressure or abrupt lifestyle changes, such as when an active person is forced to stop working or significantly alters their daily routine.
What Is Dementia?
Dementia refers to cognitive impairment affecting memory, reasoning, and behavior, but it does not affect consciousness. A person with dementia is fully alert, can communicate, and is aware of their environment; however, they may forget recent events, misplace items, or struggle with day-to-day planning. Dementia has multiple stages and types, each varying according to symptoms, behavioral changes, and internal neurological alterations.
Types of Dementia
Recent research identifies five major types of dementia based on symptoms, behavior, and brain changes. The most common form is Alzheimer’s dementia, accounting for 60–80% of all dementia cases.
1. Alzheimer’s Dementia
Alzheimer’s dementia is caused by the accumulation of amyloid plaques and neurofibrillary tangles in the brain. Amyloid is a protein that forms plaques, disrupting normal neuron function and communication. The primary symptom of Alzheimer’s dementia is difficulty remembering recent events, while memories from the distant past may remain intact.
For example, a patient may forget what they had for lunch an hour ago, yet recall events from ten years prior without difficulty. Early detection of Alzheimer’s dementia can significantly slow progression, while delayed diagnosis makes management more complex. Caring for patients at advanced stages often requires round-the-clock support, placing substantial responsibility on family members.
2. Vascular Dementia
Vascular dementia occurs due to interrupted blood flow or reduced oxygen supply to the brain. It can result from a range of conditions, including stroke, hypertension, or other vascular disorders. Even otherwise healthy individuals can experience transient vascular cognitive issues due to acute stress or sudden emotional trauma, which briefly disrupts normal brain function.
Challenges for Families and Caregivers
Caring for a person with dementia, particularly Alzheimer’s dementia, is often more challenging for family members than for the patient. Patients may forget daily tasks or events, while family members must manage routines, provide reminders, and ensure safety. This type of caregiving requires patience, dedication, and often continuous supervision.
Vascular Dementia: Causes, Symptoms, and Brain Function
Vascular dementia is a type of cognitive impairment caused by interruptions in blood and oxygen flow to the brain. Even brief reductions in cerebral blood supply can cause transient symptoms such as dizziness, momentary darkness in vision, or lightheadedness. While these effects may pass quickly in healthy individuals, prolonged disruption can damage brain tissue and, in severe cases, lead to life-threatening conditions such as coma.
How Blood Flow Affects the Brain
The brain relies on a continuous supply of oxygen and glucose from the blood. Any disruption in the transport system—whether due to blocked arteries, vascular damage, or sudden drops in blood pressure—prevents neurons from receiving adequate nutrients. Over time, this affects the neuron cycle, reduces cognitive function, and can trigger vascular dementia.
Symptoms of vascular dementia depend on the specific area of the brain affected. For example, damage to certain regions may lead to partial paralysis on one side of the body, as seen in many stroke patients. This occurs because the damaged brain area can no longer send proper commands to the corresponding body part, restricting movement.
Protein Deposits and Dementia
Vascular dementia is also linked to abnormal protein deposits in the brain. Specifically, excessive accumulation of alpha-synuclein proteins leads to the formation of Lewy bodies, which interfere with normal brain function. Proteins like alpha-synuclein play critical roles in hormone and neural regulation, but abnormal deposits disrupt neuronal communication, causing cognitive and motor impairments.
Symptoms and Physical Effects
The impact of Lewy body deposition includes:
- Movement and balance issues: Patients may experience stiffness, trembling, and difficulty coordinating movements.
- Loss of stability: Walking can become unpredictable; patients may take several normal steps before suddenly losing balance or falling.
- Cognitive fluctuations: Daily activities, such as watching a movie or engaging in conversation, can become challenging due to inconsistent brain function.
These symptoms highlight the importance of exercises that improve coordination between the brain and body. Such practices can help maintain balance, enhance motor control, and support cognitive health, reducing the severity of vascular dementia symptoms over time.
Advanced Symptoms and Protein-Related Causes of Dementia
Dementia is not only characterized by memory loss and cognitive impairment but also by subtle and complex behavioral and neurological symptoms. Patients may exhibit experiences that are elusive or difficult to describe, such as appearing conscious and responsive while simultaneously experiencing confusion or disorientation.
Elusive Experiences and Daily Life Challenges
Patients with dementia may appear engaged in conversation or daily activities, yet their responses can be inconsistent. For instance, a patient may be drinking tea or interacting with family during the day but may later forget those moments entirely. These experiences reflect the underlying neurological disturbances caused by dementia.
Behavioral symptoms often include:
- Imbalance or difficulty with coordination
- Inconsistent recognition of people or objects
- Fluctuating awareness during different times of the day
These symptoms highlight that dementia is not simply forgetfulness but a complex disorder affecting multiple brain functions simultaneously.
Protein Abnormalities in Dementia
Research shows that abnormal protein deposits are closely associated with different forms of dementia. One significant protein is TDP-43, which has been linked to frontotemporal dementia, impacting behavior, language, and decision-making. Other proteins, such as NP43, are also implicated in neurological dysfunction. These proteins accumulate in the brain, disrupting normal neuronal activity, memory formation, and cognitive coordination.
Protein abnormalities can manifest in diverse ways, such as:
- Trouble recalling words during conversation
- Inability to retrieve specific memories at certain moments
- Erratic or unpredictable behavior, which can be confusing to caregivers
Understanding these protein-related mechanisms is crucial for comprehending why dementia patients may behave inconsistently or experience sudden cognitive lapses.
Implications for Management
Managing dementia requires patience, observation, and tailored care strategies. Because symptoms can vary widely depending on the type of dementia and the specific proteins involved, caregivers must adapt to each patient’s unique needs. Supportive environments, cognitive exercises, and monitoring of daily routines can improve the patient’s quality of life and mitigate the challenges caused by protein-related brain changes.
Dementia as a Degenerative Disease: Managing Progression Naturally
Dementia is classified as a degenerative disease, meaning it progressively damages the brain over time. Unlike acute illnesses, degenerative diseases cannot be fully cured. It is important to avoid using the word “cure” in this context. However, while the damage already done to the neurons cannot be reversed, it is possible to halt or slow further progression through targeted therapies and lifestyle interventions.
Understanding the Nature of Degeneration
In dementia, some neurons are already damaged. For example, if 30 out of 100 neurons are affected, the remaining 70 neurons are still healthy. The goal of treatment is to protect these remaining neurons, preventing further decline. With consistent care—including proper diet, mental stimulation, brain exercises, and natural therapies—the progression can be effectively managed, ensuring that patients maintain quality of life.
This concept is similar to other degenerative conditions, such as arthritis, where damage to joints is permanent, but progression can be slowed or managed with therapies.
Managing Dementia Progression
Though dementia is progressive, several strategies can help control its course:
- Preventive Therapies: Interventions such as cognitive exercises, memory training, and lifestyle adjustments can preserve remaining neuronal function.
- Lifestyle and Vascular Health: Proper blood flow, oxygenation, and management of vascular risk factors are critical, as vascular issues often contribute to the degeneration process.
- Alternative and Natural Therapies: While these therapies may not reverse damage, they can slow progression and improve overall cognitive and physical well-being.
The Positive Outlook
Even though some neuronal damage is irreversible, preventing further loss is entirely possible. Patients and caregivers can focus on protecting healthy neurons, enhancing daily functioning, and maintaining independence for as long as possible.
Risk Factors for Dementia and Neurodegenerative Disorders
Certain lifestyle factors, medical conditions, and long-term habits significantly increase the risk of developing dementia and other neurodegenerative disorders. Understanding these contributing factors is crucial for both prevention and management.

Chronic Health Conditions
Individuals who have suffered from chronic health conditions for over a decade—such as hypertension, heart disease, or other cardiovascular issues—are more prone to memory decline. Many of these patients rely on long-term medications, which, while necessary for managing their conditions, can sometimes impact sleep patterns or cognitive function. Insomnia or poor sleep quality, often treated with sleeping pills, can further contribute to cognitive stress over time, making the brain more vulnerable to degenerative processes.
Toxic Exposure: Alcohol and Drugs
Excessive alcohol consumption and substance abuse are major contributors to brain toxicity. The brain relies on oxygen and glucose transported via the blood to function optimally. Chronic alcohol use introduces toxins that impair blood quality, disrupting the delivery of essential nutrients and increasing neuronal stress.
Similarly, drug abuse—including cocaine and other stimulants—hyperactivates brain pathways temporarily, but over time, it leads to lasting damage. Frequent exposure to these substances overwhelms the brain’s natural regulatory mechanisms, causing neuronal degeneration, impaired coordination, and increased risk of dementia.
Genetic and Chromosomal Factors
Chromosomal variations and genetic predispositions also play a role in neurodegenerative diseases. Proper levels of enzymes, hormones, and neurotransmitters are essential for brain function. Excessive or deficient levels of these substances, influenced by genetics or environmental factors, can contribute to conditions such as dementia or Parkinson’s disease.
Parkinson’s Disease and Brain Tissue Damage
Parkinson’s disease arises when specific areas of the brain lose their ability to receive adequate oxygen and glucose over a prolonged period. This deprivation damages deep brain tissues and cells, impairing movement, coordination, and cognitive functions. Medications are often used to mitigate further damage, but they cannot reverse the damage that has already occurred.
Additional Causes and Clinical Manifestations of Dementia and Alzheimer’s
Dementia and Alzheimer’s disease can result from a variety of neurological, physiological, and environmental factors. Understanding these causes helps in identifying at-risk individuals and providing appropriate interventions.
Role of Parkinson’s Medications and Neuronal Relaxation
Certain Parkinson’s medications, which help control hyperactivity and anxiety in patients, can also provide secondary benefits for Alzheimer’s and dementia. By relaxing neurons and reducing hyperactivation, these medications may contribute to slowing disease progression or alleviating some cognitive symptoms.
Head Trauma and Childhood Injuries
Head trauma is a significant but often overlooked contributor to dementia. Injuries sustained during childhood—such as falls or impacts to the forehead, back of the head, or upper skull—may go undetected at the time due to natural growth, hormonal changes, or lack of immediate symptoms.
Over time, these past injuries can manifest as behavioral changes or memory deficits, potentially contributing to dementia later in life. Ongoing accidents or significant head trauma in adulthood can also damage frontal or posterior regions of the brain, increasing the risk of cognitive decline.
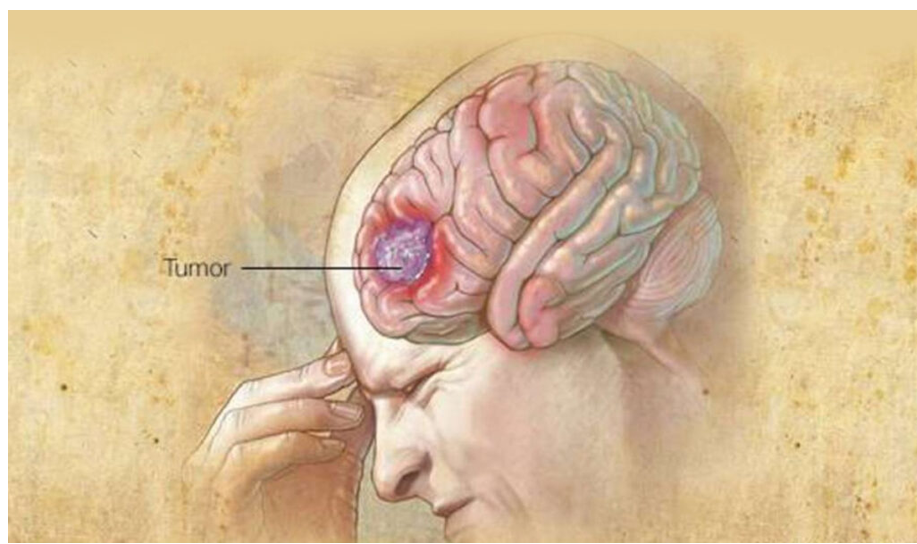
Rare Causes: Brain Tumors
In rare cases, brain tumors may trigger dementia or Alzheimer’s. Tumors located in surgically inaccessible regions can interfere with brain function, creating neurological deficits. While some tumors can be removed surgically, others remain and may progressively affect cognition and memory.
Clinical Manifestations and Symptoms
Recognizing early signs of dementia is essential for timely intervention. Key clinical symptoms include:
- Forgetfulness: The most common and noticeable sign, affecting recent or past memories. Patients may forget events, tasks, or daily routines. Early observation of forgetfulness helps determine the type and stage of dementia.
- Difficulty with Daily Activities: Gradual challenges in performing routine activities, such as managing finances, cooking, or personal care, often accompany memory decline.
- Behavioral Changes: Stress, trauma, or hormonal changes—such as those occurring during menopause—can exacerbate forgetfulness or mimic early dementia symptoms.
It is important to note that not every instance of forgetfulness indicates dementia. Careful assessment of patterns, frequency, and associated cognitive or behavioral changes is required to make an accurate diagnosis.
Impact of Dementia and Alzheimer’s on Daily Activities and Cognitive Function
Dementia and Alzheimer’s disease not only affect memory but also significantly impair an individual’s ability to perform routine daily activities. These challenges create substantial difficulties for both patients and their caregivers.
Challenges with Routine Activities
Patients with dementia often experience confusion during basic activities. For example, they may feel the urge to pass urine or stool but forget the sequence of actions required, leading to accidents. Even after performing these functions, they may be unable to manage hygiene independently, such as washing or cleaning themselves.
Similarly, patients may forget how to eat, use utensils, or carry out personal hygiene tasks such as bathing. These lapses can last from seconds to several minutes, during which the individual may appear “blank” or unresponsive. These disruptions are distressing not only for the patients but also for family members who must provide constant assistance.
Language and Communication Difficulties
Language impairment is a common and gradual symptom in dementia. Patients may:
- Forget specific words while speaking.
- Stop mid-conversation due to an inability to recall the topic.
- Confuse or forget the language they are using, especially if they are multilingual.
- Have difficulty pronouncing words clearly, making it hard to communicate their thoughts.
These language difficulties significantly reduce the patient’s ability to express themselves, leading to frustration and social withdrawal.
Impaired Judgment and Cognitive Awareness
Dementia affects judgment and awareness, creating a gap between consciousness and action. Patients may be aware of their surroundings yet unable to make appropriate decisions or execute tasks correctly. Their conscious and subconscious minds appear to “juggle,” causing inconsistent behavior—knowing what to do one moment but forgetting it the next.
Confusion and Depression
Confusion is a hallmark of dementia, often occurring alongside depression. Even individuals without dementia may experience occasional confusion, but persistent cognitive lapses can lead to chronic stress and negative emotions. When patients are unable to remember tasks, communicate effectively, or maintain independence, feelings of helplessness and frustration may develop, increasing the risk of depression.
As dementia progresses, patients may experience increased white matter in the brain, which impairs their ability to make decisions. Simple choices become overwhelming, leading to prolonged confusion. This inability to act decisively often triggers feelings of depression. When depression sets in, it can worsen the condition by further disrupting brain cells and increasing white matter, which in turn negatively affects memory and cognitive function.
This creates a vicious cycle: confusion leads to depression, depression leads to further brain damage, and brain damage intensifies confusion. Breaking this cycle requires careful, patient care, proper counseling, and continuous support from caregivers and family members.
The Vicious Cycle of Dementia: Confusion, Depression, and Cognitive Decline
Dementia and Alzheimer’s disease often create a self-reinforcing cycle of cognitive decline, emotional instability, and behavioral changes. One of the primary challenges in these conditions is the impact on decision-making and emotional well-being.
Dependence on Caregivers
Patients with advanced dementia or Alzheimer’s often regress to a child-like dependence. They rely entirely on caregivers for daily tasks, requiring constant patience and attentive care. Handling such patients demands calmness, understanding, and a structured routine to maintain their well-being. Proper care and consistent management, though challenging, can lead to noticeable improvements in the patient’s quality of life.
Cognitive and Thinking Challenges
Cognitive functions, particularly thinking and judgment, are severely affected. Patients may remain conscious yet unaware of their actions. They may forget tasks they just completed or struggle to plan their next steps. Some patients develop hyperactive thoughts, while others may appear almost statue-like, sitting for hours without engaging with their surroundings.
Sometimes, persistent recall and deep thinking can yield positive results, allowing patients to remember certain tasks or experiences. However, in many cases, it leads to frustration, irritability, and hyperactivity.
Loss of Interest and Motivation
A common symptom in dementia is a lack of interest in work, hobbies, or previously enjoyable activities. This symptom is not unique to dementia—healthy individuals can feel demotivated after repeated failures—but in dementia, the effect is amplified due to impaired memory and judgment. Patients may lose confidence in their abilities and withdraw from activities, further isolating themselves and contributing to emotional distress.
For example, a normally motivated individual might abandon a project after a few setbacks, opting for a safer alternative. In dementia, this withdrawal occurs more frequently and intensely, often leaving the patient passive and disengaged.
Dementia and Its Impact on Interest, Physical Movement, and Daily Functioning
Dementia affects not only memory but also motivation, physical activity, and daily functioning. One of the key symptoms observed in patients is a loss of interest in work and hobbies. Even activities that once brought joy, such as traveling, dancing, or creative hobbies, may no longer engage the patient. This decline in interest leads to reduced physical activity, which further impacts overall health. Without engagement in stimulating tasks, both the mind and body become less active, creating a cycle of physical and mental stagnation.
Drowsiness and Reduced Energy
Drowsiness and laziness are common in dementia patients. From an Ayurvedic perspective, these symptoms arise when aggravations occur in the body, such as imbalance in the doshas, poor digestion, or inadequate nutrition. The brain requires proper nourishment and energy to function, much like the stomach needs a healthy gut for digestion. Imbalances in the body manifest as fatigue, reduced alertness, and a general sense of lethargy. In non-dementia individuals, detoxification, gut cleansing, and proper nutrition can often alleviate drowsiness.
Impaired Reasoning and Judgment
Cognitive decline also manifests as impaired reasoning and judgment. Patients may struggle to make decisions, perform simple tasks, or give appropriate responses to everyday situations. This symptom gradually worsens over time, beginning with minor forgetfulness and eventually affecting more complex cognitive abilities. Early recognition of these symptoms is critical to effective management.

Diagnostic Evaluation
The cornerstone of diagnosing dementia lies in detailed history-taking and physical examination. Advanced testing is important, but understanding the patient’s history often provides 80% of the necessary information. History-taking includes observing changes in behavior, routine activities, mobility, communication, and social interactions over time.
Physical examination for dementia differs from typical medical exams. Clinicians focus on assessing memory, cognition, and functional abilities rather than standard measures like heart rate or blood pressure. Observing gait, facial expressions, eye contact, and communication patterns provides insight into the patient’s neurological health. For example, patients may avoid eye contact, have a lowered gaze while speaking, or exhibit phobias and confusion during interactions. Additionally, simple observational tests, such as asking how they traveled to the clinic or recalling daily activities, help assess memory and cognitive function.
Diagnostic Evaluation and Advanced Testing for Dementia
Accurate diagnosis of dementia requires a comprehensive evaluation, combining physical examination, mental assessment, and advanced imaging techniques.
Physical Examination
Physical examination for dementia involves observing the patient’s motor coordination and functional abilities. For example, a clinician may ask the patient to lift one hand or leg, balance on their toes for several seconds, or perform simple coordinated movements. These tests help assess muscle strength, balance, and neurological function, providing insight into the stage and severity of dementia.
Mental Status Examination (MSE)
The Mental Status Examination (MSE) is a more advanced evaluation, often performed by a psychologist or psychiatrist. It involves detailed questioning to assess memory, cognition, and orientation. Patients may be asked about:
- Their birth date and recent birthdays
- Past trips or travel experiences
- Daily routines and significant recent events
Additionally, the examiner may present tasks requiring attention, observation, and categorization, such as identifying colored objects or following multi-step instructions. Performance on these tasks helps identify cognitive deficits and specific neurological impairments.
Imaging Techniques
If clinical evaluation suggests abnormalities, imaging studies are used to detect structural issues in the brain:
- CT Scan: Helps identify tumors, clots, or major brain abnormalities.
- MRI Scan: Provides detailed images of brain structures and vascular pathways, revealing issues such as arterial blockages, tissue damage, or other internal imbalances.
These imaging tools allow physicians to confirm or rule out physical causes of cognitive decline.
Neuropsychological Testing and Daily Living Assessment
For deeper evaluation, neuropsychological tests assess memory, cognition, motor skills, and emotional responses. Psychologists, psychiatrists, or neurologists use specialized tools to:
- Evaluate response to stimuli
- Test problem-solving and reasoning
- Assess daily living capabilities
Blood tests may also be conducted to check for abnormal protein levels or other biomarkers linked to dementia. These assessments are advanced and require specialist expertise; naturopaths may assist with initial examinations or basic tests, but prescriptions and in-depth diagnostic tests are performed only by qualified medical professionals.
Management and Therapeutic Approaches for Dementia and Alzheimer’s Disease
Once the clinical manifestations of dementia or Alzheimer’s are identified, the primary goal of treatment is to slow disease progression and improve quality of life. While the damage already present in the brain cannot be reversed, interventions can help prevent further deterioration and manage behavioral symptoms.
Pharmacological Interventions
Doctors often prescribe medications based on the patient’s stage and symptom severity:
- Antipsychotic drugs are commonly used to calm patients and regulate hyperactive behavior.
- Antidepressants and anti-anxiety medications may be indicated when patients exhibit high anxiety or agitation.
- Medication doses and combinations are tailored individually, taking into account natural surroundings, lifestyle, and behavioral tendencies.
These pharmacological interventions aim to reduce hyperactivity, anxiety, and confusion, ensuring the patient remains as calm and stable as possible.
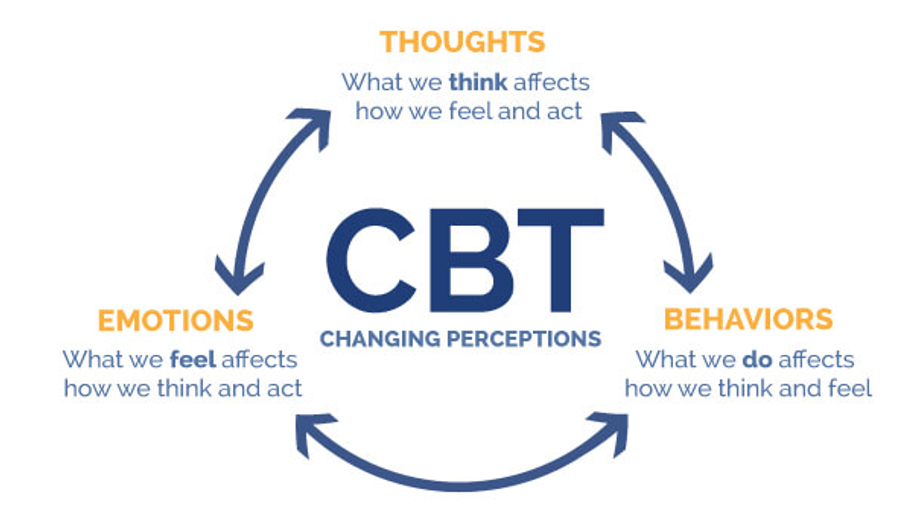
Cognitive and Behavioral Therapy
One of the most effective non-pharmacological treatments is Cognitive Behavioral Therapy (CBT). This therapy helps patients manage anxiety, fear, and phobias, particularly in challenging situations such as crowded or noisy environments.
Patients with dementia or Alzheimer’s may experience sudden panic or confusion in such situations, imagining threats that do not exist and reacting in self-preservation. CBT gradually exposes patients to these triggers in a controlled manner, helping them:
- Stay calm under stressful circumstances
- Rebuild trust and feel supported
- Reduce impulsive or potentially harmful reactions
Successful cognitive therapy requires patience, consistency, and strong family or caregiver support. Sessions may take time, but with proper guidance, patients can regain a sense of security and stability, leading to meaningful improvements in behavior and daily functioning.
Integration with Alternative Therapies
Even in the context of alternative or naturopathic care, cognitive therapy is considered a cornerstone intervention, as it directly addresses the patient’s mental and emotional regulation. Complementary therapies, lifestyle adjustments, and supportive care all enhance the effectiveness of CBT.
Alzheimer’s Disease Overview
Alzheimer’s disease is a chronic neurological disorder and represents a progressive form of dementia. While pharmacological and cognitive therapies cannot fully reverse the condition, they can significantly slow progression, improve daily functioning, and reduce the burden on patients and caregivers. Early recognition and intervention remain critical to optimizing outcomes.
Alzheimer’s Disease: Causes, Pathophysiology, and Clinical Manifestations
Alzheimer’s disease is a progressive degenerative neurological disorder characterized by a gradual loss of cognitive function and disturbances in behavior. Patients retain consciousness and awareness, but their ability to process, remember, and respond to information is increasingly impaired. The disease progresses slowly from its earliest stages, and early detection is critical to managing symptoms and maintaining a functional quality of life.
Etiological Factors
Alzheimer’s disease has multiple contributing factors, some of which are beyond human control:
- Genetic Predisposition:
Genetic coding abnormalities in DNA can increase susceptibility. Hereditary factors play a significant role in the early onset and progression of the disease. - Head Injuries:
Traumatic brain injuries, whether in childhood or adulthood, can predispose individuals to Alzheimer’s by damaging brain tissues and affecting neural networks. - Neurotransmitter Disturbances:
Reduced synthesis of acetylcholine, a key neurotransmitter, disrupts communication between neurons, contributing to cognitive decline and memory loss. - Neuropathological Changes:
- Neurofibrillary Tangles: Abnormal fibrous structures within neurons that interfere with cell function.
- Neuritic (Amyloid) Plaques: Deposits of amyloid proteins that accumulate between neurons, further impairing neural function.
Both tangles and plaques act as pathological triggers, exacerbating neuronal damage and disease progression.

Clinical Manifestations
Alzheimer’s disease presents with a distinct clinical profile compared to other forms of dementia:
- Memory Loss:
Unlike general forgetfulness seen in dementia, memory loss in Alzheimer’s is profound. Patients often fail to recall recent events, learned knowledge, or even personal information, and memory deterioration is usually irreversible. - Difficulty with Daily Activities:
Patients struggle with routine tasks such as dressing, bathing, and eating. Even simple activities may become overwhelming, reflecting the loss of procedural memory. - Social Impairment:
Recognition of family members and close acquaintances becomes difficult. Patients may forget names, relationships, or even the faces of loved ones, leading to social withdrawal and isolation. - Impaired Learning and Recall:
Retention of newly acquired knowledge and previously learned information is significantly compromised. Educational or work-related skills, previously mastered tasks, and learned behaviors are progressively lost.
Alzheimer’s disease is a chronic and progressive condition, meaning that early detection and intervention are vital to slow its progression and support patients’ cognitive and functional abilities. Understanding the underlying causes and clinical manifestations helps caregivers, families, and medical professionals design appropriate therapeutic and supportive strategies.
Progression and Advanced Clinical Features of Alzheimer’s Disease
As Alzheimer’s disease advances, the cognitive decline becomes more profound, affecting not only memory but also previously acquired knowledge and routine skills. Individuals who once had high levels of education or professional expertise may lose the ability to recall learned information. Essentially, the “data” stored in their brains becomes corrupted, similar to how a computer virus can disrupt digital information. This corruption of neural data leads to deepening confusion, where patients make repeated attempts to recall information but fail, creating frustration and mental strain.
Sleep and Circadian Disruption
Alzheimer’s patients often experience sleep disturbances, including insomnia and irregular sleep patterns. The circadian rhythm, which regulates natural sleep-wake cycles, is severely disrupted. As a result, patients may struggle to sleep at night, remain drowsy during the day, or show no consistent sleeping schedule. This disruption contributes further to orientation problems, memory deficits, and overall cognitive instability.
Progressive Loss of Functional Skills
In advanced stages, Alzheimer’s affects multiple aspects of daily functioning:
- Orientation and Recognition: Patients may be unable to recognize familiar people, places, or objects.
- Speech and Communication: Speaking skills deteriorate, making it difficult to express needs or thoughts.
- Agitation and Anxiety: Heightened confusion often leads to agitation, paranoia, and anxiety, particularly in unfamiliar or overstimulating environments.
- Dependency on Caretakers: As the disease progresses, patients become completely dependent on caregivers for daily activities. In the final stages, individuals may lose voluntary control over movements and function almost entirely as passive recipients of care.
The Final Stage
In the late stages of Alzheimer’s, patients may appear like automatons, requiring total assistance for basic needs such as feeding, hygiene, and mobility. Their awareness of self diminishes, and they lose all connection to prior knowledge, preferences, or personal identity. While rare, these cases represent the extreme progression of the disease, illustrating the irreversible nature of severe Alzheimer’s.
Globally, ethical considerations such as mercy killing or euthanasia may arise in such cases, though this remains legally restricted in countries like India. Nevertheless, understanding the trajectory of Alzheimer’s helps caregivers, families, and healthcare professionals provide compassionate, patient-centered care throughout the disease progression.
Advanced Stages of Alzheimer’s and the Role of Natural Therapy
In the final stages of Alzheimer’s disease, patients often lose the ability to perform even the simplest tasks independently. Imagine for a few minutes experiencing complete memory loss: forgetting where you are, what to do, or how to move your body. For these patients, even basic movements like walking, eating, or personal hygiene become impossible without assistance. Their condition may progress to immobility, where the body can no longer respond to the brain, leaving the individual entirely dependent on caregivers.
In many parts of the world, mercy death or euthanasia is legally considered for patients in such conditions. This remains a topic of ethical debate. While some view it as a humane solution to prevent prolonged suffering, others consider it a morally challenging decision. For families, particularly in middle-class settings with limited resources, managing 24-hour care, medications, and medical bills can be overwhelming. The emotional and financial burden of caregiving in such cases is significant, making Alzheimer’s not only a personal but also a societal challenge.
Diagnosis and Modern Medical Management
Diagnosis of Alzheimer’s involves a combination of history-taking, neurological assessment, and advanced investigations, including:
- EEG (Electroencephalography) to assess brain activity
- CBC and blood chemistry profiles
- CT scan and MRI to detect structural changes or abnormalities in the brain
- CSF (Cerebrospinal Fluid) analysis
Once the disease stage is determined, treatment focuses on slowing progression and managing symptoms. This may include:
- Cholinesterase inhibitors to improve neurotransmitter function
- Behavioral and cognitive therapies administered by psychologists or psychiatrists to reduce anxiety and agitation
- Psychological therapy to help patients relearn essential tasks and restore a sense of normalcy
Behavioral therapy can be transformative, providing patients with structured guidance to relearn daily activities and maintain mental engagement, sometimes offering a ray of positivity even in advanced stages.

Role of Natural and Alternative Therapies
While conventional medicine plays a critical role, natural or alternative therapies can also provide significant benefits. These therapies do not rely on medications or injections but instead focus on supporting overall health, reducing medication side effects, and improving quality of life. Many Alzheimer’s patients take multiple medications for coexisting conditions, and long-term drug use can contribute to additional complications, including worsening cognitive decline.
Natural therapy helps by:
- Cleansing the system and improving metabolic balance
- Lowering the side effects of long-term medications
- Supporting brain and body function to maintain residual abilities
- Creating a supportive and calming environment that reduces stress and hyperactivity
When applied consistently, natural therapy can complement medical treatment, helping patients achieve a better quality of life and potentially slowing disease progression. Caregivers and therapists play a crucial role in this holistic approach, offering patience, structured routines, and therapeutic interventions that address both physical and psychological needs.
Natural Approaches to Supporting Brain Health in Alzheimer’s and Dementia
Managing Alzheimer’s disease and dementia requires a combination of medical intervention, behavioral therapy, and lifestyle adjustments. While medications and cognitive therapies are essential, natural therapies and nutrition can play a remarkable role in slowing disease progression, reducing symptoms, and supporting overall brain function.
Memory-Enhancing Herbs
Certain herbs gifted by nature have been shown to support cognitive function and memory. Knowledge of these herbs allows them to be used almost like natural medicines. Among the most effective are:
- Wheatgrass
- Alfalfa
- Ashwagandha
- Brahmi (Bacopa monnieri)
These herbs are particularly effective because their pH levels are compatible with human blood, allowing for easy absorption and delivery of nutrients to the brain. They can support patients at any stage—whether acute, chronic, or in early forgetfulness—by enhancing memory and overall brain function.
Dietary Support for Brain Health
Nutrition plays a crucial role in maintaining cognitive health. A balanced diet with easy-to-digest, alkaline, and fiber-rich foods is recommended. Foods rich in vitamins B6, B9, and B12 act as natural brain boosters and memory enhancers:
- Vitamin B6: Potatoes, sweet potatoes, bananas, mangoes, cereals, and for non-vegetarians, chicken and tuna.
- Vitamin B9 (Folate): Green leafy vegetables such as spinach, fenugreek, amaranth, and seasonal regional greens. Legumes, eggs, sunflower seeds, broccoli, avocado, beetroot, and bananas also contribute.
- Vitamin B12: Primarily found in animal-based products for non-vegetarians, but vegetarians can focus on fortified foods.
It is important to adhere to dietary habits that the patient is accustomed to. Vegetarians, for instance, do not need to switch to non-vegetarian foods, as plant-based proteins are sufficient for maintaining health. Seasonal and regional foods are preferable, ensuring affordability and ease of access while still meeting nutritional needs. Even including two or three key sources of B6 or B9 daily can be effective for supporting cognitive function.
Lifestyle Practices
In addition to herbs and diet, yoga, meditation, and mindfulness practices can help reduce stress, improve focus, and enhance overall mental wellbeing. These practices complement dietary and herbal interventions, supporting patients both physically and psychologically.
Essential Nutrients and Foods to Support Brain Health
Maintaining brain health, particularly in conditions like Alzheimer’s and dementia, requires a combination of proper nutrition, supplementation, and lifestyle adjustments. Certain vitamins, minerals, and foods have a direct impact on cognitive function, memory, and overall neurological wellbeing.
Vitamin B12 and D3
Vitamin B12 is essential for brain function and neuron health, while Vitamin D3 supports bone health, improves circulation, and regulates hormone and enzyme secretion. Deficiency in these vitamins is common—studies show that 1 in 5 people may have B12 and D3 deficiencies—making supplementation or dietary inclusion crucial.
- Sources of B12:
- Non-vegetarians: Beef, liver, and oysters.
- Vegetarians: Dairy products and fermented foods.
- Indian cuisine: Traditional fermented foods such as idli, dosa, Gujarati dhokla, homemade pickles, and cow ghee are excellent sources of B12.
- Sources of Vitamin D3: Sunlight is the most natural and freely available source. Those living in sunny regions, such as much of Asia, can easily benefit from daily sun exposure.
Incorporating these foods into daily meals can improve nutrient absorption, enhance brain function, and support overall physical health without causing digestive discomfort.
Polyunsaturated Fats and Nuts
Walnuts are highly recommended for cognitive health. They are rich in polyunsaturated fatty acids, essential for brain function. Interestingly, walnuts resemble the human brain in shape, and their nutrient profile supports neural development and maintenance. Best practices include:
- Soak 4–5 walnuts for 5–7 hours before consumption.
- Consume them during mid-afternoon (4–6 p.m.), which is considered an optimal “snacking” window for digestion and energy.
Other beneficial nuts and seeds include:
- Flax seeds: Rich in omega-3 and omega-6 fatty acids and dietary fiber; 1–2 tablespoons of roasted seeds daily is recommended.
Starchy and Whole Grains
Certain starchy foods and grains can also support brain health and provide sustained energy:
- Corn: Opt for whole corn or freshly made corn flour for chapatis. Avoid white refined corn flour as it lacks fiber and essential nutrients.
- Other starchy vegetables: Potatoes, sweet potatoes, and legumes provide energy while being rich in essential nutrients.
Regional and Seasonal Considerations
It is important to select foods that are seasonal and locally available. For example:
- Avocado is highly beneficial if consumed in regions where it is naturally grown.
- For vegetarians, diverse options like green leafy vegetables, legumes, and dairy products can provide sufficient protein and micronutrients without needing to switch to non-vegetarian sources.
Yoga, Mudras, and Natural Therapies for Cognitive Health
Maintaining cognitive health and supporting patients with Alzheimer’s, dementia, or memory-related issues requires a holistic approach that combines physical exercise, brain activation techniques, yoga, mudras, and natural therapies. These practices not only improve memory and neuronal function but also enhance overall well-being.
Physical Exercise and Brain Activation
Regular physical exercise and brain activation exercises are fundamental. Gentle movement, stretching, and activities that stimulate coordination help improve blood circulation, oxygenation of the brain, and overall neurological function.
Yoga Asanas
Certain yoga postures (asanas) are particularly effective in improving digestion, metabolism, and gut health, which are closely linked to brain function:
- Vajarasana (Thunderbolt Pose):
- This asana is unique as it can be performed after meals, such as lunch or dinner.
- Sitting in Vajarasana for 3–5 minutes improves digestion and gut health.
- For those unable to sit on the floor, a pillow or bed can be used for support.
- Proper guidance is recommended for beginners, as this pose involves working against gravity.
- Paschimottanasana (Seated Forward Bend):
- This posture enhances flexibility, stimulates circulation, and aids in relaxation.
These asanas, when practiced regularly, provide profound benefits for both physical and cognitive health.
Mudras and Shirodhara
- Yi Mudra: A simple hand gesture that promotes mental clarity and relaxation.
- Shirodhara Therapy: A traditional Ayurvedic practice in which a steady stream of warm oil flows over the Sahasrara chakra (crown chakra) for 45–50 minutes. This therapy:
- Stimulates memory and neuron activity
- Promotes deep relaxation
- Balances the body’s energy systems
Massage and Water Therapy
- Gentle Massage: A monthly massage can enhance circulation, aid in detoxification, and provide deep relaxation.
- Water Therapy: Techniques include drinking water for hydration, enema, jet sprays, tub baths, and periodic liquid diets. Water therapy helps cleanse the system, detoxify the body, and support overall wellness.
- Steam Baths: Regular steam therapy aids in toxin elimination and rejuvenation.
Understanding Neuropathological Factors
For those interested in technical details, neurofibrillary tangles are misfolded protein formations in the brain that disrupt neurotransmitter cycles and can contribute to clotting or blockages. These tangles interfere with normal neuronal function and are often observed in conditions like Alzheimer’s disease. Addressing these requires a combination of lifestyle, dietary, and medical interventions.
Naturopathy Management of Dementia: Treatments, Therapies, and Practical Guidance
The management of dementia and memory-related disorders in naturopathy involves a combination of herbal supplements, dietary guidance, behavioral therapies, and supportive care. This holistic approach not only addresses the symptoms but also aims to improve the patient’s overall quality of life.

Herbal and Natural Interventions
One of the commonly recommended interventions is the use of Ashwagandha, a natural adaptogen known for its neuroprotective properties.
- Duration of Use:
- Initially, Ashwagandha should be administered for a minimum of 60 days.
- Based on symptom improvement, it can be continued for longer periods—even up to a year.
- Dosage and combination of herbs may be adjusted over time to maximize benefits without causing harm.
Other memory-enhancing herbs and supplements, including omega-3 oils, wheatgrass, and alfalfa, are also commonly integrated into treatment plans. These help improve neuronal function and support brain health, particularly when used consistently.
Behavioral Therapy
Cognitive Behavioral Therapy (CBT) plays a central role in the management of dementia. Key objectives include:
- Teaching patients how to manage their daily routines and perform regular activities.
- Guiding them to relearn tasks, similar to the approach used with children during early learning stages.
- Engaging patients in structured conversations and activities that stimulate memory and cognitive function.
Behavioral therapy requires patience, consistency, and emotional support from caretakers. The therapist works closely with the patient to gradually improve their functional independence and reduce anxiety.
Patient-Centered Management
Effective dementia management goes beyond a single therapy. It requires:
- Understanding the patient’s symptoms, age, and coexisting health issues.
- Making gradual adjustments to behavior, diet, and daily routines.
- Incorporating natural therapies, herbs, and supportive care.
- Providing constant support and monitoring, akin to a caretaker role.
Success depends largely on patience, consistency, and empathy, rather than attempting to treat the patient as a passive recipient of care.
Internship and Practical Exposure
For students pursuing naturopathy, gaining practical experience in reputable hospitals can be valuable. Many hospitals, including large chains, maintain alternative or naturopathy departments as part of government regulations.
- Students may have the opportunity to intern in these departments once they receive their valid qualifications.
- Guidance and links to hospitals offering internships are provided by the institute after certification.
- Internships provide hands-on experience in patient care, behavioral therapy implementation, and naturopathy interventions.
This approach emphasizes a holistic, patient-centered, and evidence-informed methodology, combining natural remedies, behavioral therapies, and structured care to manage dementia effectively.
Accessing Dementia Treatment Materials and Follow-Up Guidance
During the lecture on dementia management and naturopathy interventions, several students requested access to the presentation slides and supporting materials for further study. The instructor clarified the process for obtaining these resources and additional patient experiences.
Slide Access and Online Resources
Students can access the presentation slides and recorded lecture videos through the institute’s online portal. The portal includes:
- Patient experiences: Documented cases of various diseases, including dementia, highlighting real-life management outcomes.
- Lecture recordings: Videos are uploaded within 2–3 days of the live session, allowing students who missed the live lecture to review the content at their convenience.
- Official links: All necessary links to videos and resources are shared in the chat during the lecture and are also available via email if needed.
Students are encouraged to regularly check the portal to stay updated with the latest presentations and supporting materials.
Additional Support and Queries
For any remaining questions or clarifications:
- Students can email the instructor at the official institute email ID.
- The administrative team can be contacted directly for scheduling concerns, such as requests for weekend classes or personal accommodations, as lecture platforms focus solely on educational content.
The instructor emphasized that while lecture-related queries can be addressed immediately, administrative and scheduling decisions are handled separately by the support team.
Conclusion
In today’s modern and fast-paced lifestyle, dementia and Alzheimer’s disease are becoming increasingly common and are no longer limited to the elderly population. Continuous exposure to environmental pollution, chemical toxins, mental stress, unhealthy dietary habits, lack of physical activity, and excessive dependence on digital devices has a gradual yet harmful impact on brain health. These factors silently weaken brain neurons over time, leading to memory loss, reduced concentration, confusion, and cognitive decline. Therefore, maintaining brain health is not an option but a necessity for individuals of all age groups.
The brain is a highly sensitive and complex organ that requires adequate oxygen, proper nutrition, mental stimulation, and emotional balance for optimal functioning. When the brain does not receive these essential requirements, neuronal communication becomes weak, increasing the risk of neurodegenerative disorders such as dementia and Alzheimer’s. However, the human brain has an incredible capacity for adaptation and healing through neuroplasticity. This ability allows the brain to form new neural connections and strengthen existing ones when stimulated through regular mental and physical activities.
Brain health and memory-boosting exercises play a crucial role in preventing cognitive decline naturally. Simple practices such as memory recall exercises, reading, writing, learning new skills, problem-solving tasks, meditation, pranayama, and physical exercise help improve blood circulation to the brain and enhance oxygen supply. These activities nourish brain cells, support nerve communication, and slow down age-related memory deterioration. Importantly, such exercises are beneficial not only for individuals suffering from memory problems but also for healthy individuals who wish to maintain mental sharpness and prevent future disorders.
A natural and holistic lifestyle significantly contributes to brain health. Consuming a balanced diet rich in natural nutrients, staying well-hydrated, maintaining proper sleep cycles, and reducing exposure to toxins support overall neurological function. Emotional well-being and stress management are equally important, as chronic stress negatively affects memory and learning abilities. Social interaction, positive thinking, and mental relaxation techniques help maintain emotional stability and prevent isolation, which is a known risk factor for dementia.
From a naturopathic perspective, prevention is always better than cure. Dementia and Alzheimer’s are not unavoidable consequences of aging but are strongly influenced by long-term lifestyle patterns. Early awareness, disciplined daily routines, and consistent brain-stimulating practices can delay or even prevent the onset of these conditions. By integrating natural therapies, physical activity, and mental exercises into everyday life, individuals can protect their cognitive abilities and maintain independence in later years.
In conclusion, caring for the brain is a lifelong process that requires conscious effort and holistic living. By adopting natural preventive measures and maintaining mental activity, we can preserve memory, enhance cognitive function, and improve quality of life. A healthy brain ensures clarity of thought, emotional balance, and graceful aging, making brain health a fundamental pillar of overall well-being.