Epilepsy
Epilepsy

Understanding Epilepsy: A Brief Overview
Epilepsy, derived from the Greek word “seizure,” is a neurological disorder characterised by recurrent and unprovoked seizures. In India, it is estimated that more than 10 million people (about half the population of New York) are affected by epilepsy, with approximately 1% of the population at risk of developing the condition. Interestingly, the prevalence of epilepsy is higher in rural areas compared to urban regions, highlighting the need for increased awareness and access to healthcare in rural communities.
Epilepsy is the fourth most common neurological problem globally, affecting people of all ages. Fortunately, approximately 70% of individuals with epilepsy respond well to treatment, which often involves the use of antiepileptic medications.
The Brain and Seizures
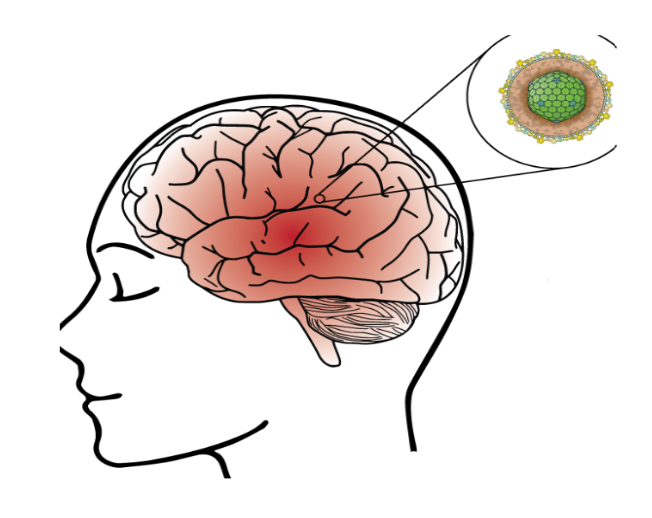
The brain serves as the control center for all voluntary and involuntary responses in the body. It is composed of nerve cells that communicate with each other through electrical activity. A seizure occurs when there is a sudden, uncontrolled electrical disturbance in the brain, leading to changes in behavior, movements, feelings, and levels of consciousness.
If a person experiences two or more seizures or tends to have recurrent seizures, they are diagnosed with epilepsy. Most seizures last from 30 seconds to 2 minutes, but a seizure that lasts longer than 5 minutes is considered a medical emergency and requires immediate attention.
Epilepsy is a neurological disorder characterized by recurrent unprovoked seizures, which are sudden, Abnormal changes in the Brain’s electrical activity leading to various symptoms such as convulsions, a loss of Consciousness, and sensory disturbances.

SEIZURE is a Paroxysmal motor, sensory, or autonomic event. It is a sudden uncontrolled obstacle, it might be Emotions of Action. When a Seizure is Abnormal or excessive, Synchronous Electrical discharge for 5 minutes is a status epilepticus, “Convulsion “ which means motor Seizure.
Epilepsy is a chronic disease of the Brain with recurrent, Unprovoked Seizures, 2 or more unprovoked Seizures. Separate by at least 24 hours.
Epilepsy is not contagious; it is not a mental illness or a cognitive disability. The neurological dysfunction seen in epilepsy can Begin at Birth, Childhood, adolescence, or even adulthood. It can happen anytime.
In Epilepsy Hotspot is damage in your brain, if a Seizure Hotspot is in the Motor nerve, then the factors will be seen through symptoms, if it is in Language then it will be seen through the person’s language, and if it is in eyes, then it will be seen through person’s eyes. Epilepsy measures Symptoms are fear of light, Blinking of the Eyes, and they can’t do an Eye Contact. This leads to disturbances in the electric functions of the brain causing neurological conditions, Characterized by recurrent seizures.
Epilepsy Symptoms; Loss of Consciousness, Anxiety, Starring, weakness, Muscle and contraction Epilepsy is a disorder marked by a Disturbance of Electrical Rhythms in the Central Nervous System
What are the Causes of Epilepsy`
1. Stroke
2. Brain Tumor
3. Infections A such as meningitis or encephalitis
4. Traumatic brain or Head Injury
5. Loss of oxygen to the brain
6. Certain Genetic Conditions
7. Other Neurological Conditions
8. Alcoholism or Alcohol withdrawal

What to do spot the stroke
Symptoms to spot a Stroke
1. Face Drooping
2. Arm Weakness
3. Speech Difficulty
Time to see medical attention.
stroke come we have heard that there is a blockage in the heart so there is a chance of blockage in the Brain too

Signs of Autism
It can be seen in children that they are not able to learn things properly, they are shy, Ignore the danger, and avoid Eye contact. Early Warnings Signs of Cognitive Impairment
- No reaction to play
- Delayed milestones (crawling, talking)
- Baby doesn’t seem to recognize your face or voice
- Little Laughing or crying
This is the Cause of Epilepsy

- Symptoms of Mild Cognitive Impairment
· Missing appointments or important Events
· Overwhelmed by decision-making or Planning activities
· Forgetting words or feeling they are on the tip of the tongue
· Forgetting Conversations or losing a train of thoughts
Meningitis Symptoms
- Fever
- Sleepless
- Light sensitivity
- Vomiting
- Joints pain
1. Fever: Meningitis often causes a high fever, which is the body’s natural response to infection. It can occur suddenly and may be accompanied by chills.
2. Sleeplessness: Meningitis can disrupt sleep patterns due to the discomfort and pain it causes. Patients may find it difficult to sleep or experience frequent awakenings.
3. Light sensitivity: Also known as photophobia, this symptom is common in meningitis. Patients may find bright lights uncomfortable and may prefer dimly lit environments.
4. Vomiting: Nausea and vomiting are common symptoms of meningitis, often occurring due to the body’s inflammatory response and increased intracranial pressure.
5. Joint pain: Meningitis can cause generalized body aches, including joint pain. This symptom is often described as a dull, constant ache in the affected joints.
If you or someone you know is experiencing these symptoms, it’s crucial to seek medical attention promptly for an accurate diagnosis and appropriate treatment.
Complications of Encephalitis
1. Learning Challenges: Encephalitis can impact cognitive functions, including memory, attention, and problem-solving, leading to learning difficulties. These challenges can vary in severity and may require educational support.
2. Cognitive Decline: Some individuals may experience long-term cognitive decline after encephalitis, which can affect their ability to think, reason, and remember information. This decline can be gradual and may require ongoing support.
3. Weakness or Coordination Difficulties: Encephalitis can cause damage to the brain, leading to muscle weakness, poor coordination, or balance problems. Physical therapy may be needed to improve these symptoms.
4. Vision Changes: Encephalitis can affect the optic nerve or brain regions responsible for vision, leading to visual disturbances such as blurry vision, double vision, or even vision loss in severe cases.
5. Epilepsy: Some individuals may develop epilepsy after encephalitis, characterised by recurrent seizures. These seizures can vary in type and severity and may require medication to control.
6. Hydrocephalus: Encephalitis can lead to the buildup of cerebrospinal fluid in the brain, known as hydrocephalus. This can increase pressure inside the skull, leading to symptoms such as headache, nausea, and changes in mental status. Treatment may involve the placement of a shunt to drain the excess fluid.
1. Encephalitis
2. Inflammation of brain
- Meninges
- Cerebellum
- Brainstem
Characteristics
- Fits can Vary in duration, intensity and duration
- Symptoms may include loss of consciousness, muscle jerking, or conclusions, sensory changes, emotional alterations and cognitive impairments.
- Understand the common causes and risk factors is crucial for identifying potential triggers
And it helps in developing appropriate management strategies.
Connections with other diseases:
- Epilepsy can be associated with other neurological conditions such as migraine, autism spectrum disorder, cerebral palsy, and neurodevelopmental disorders.
- Additionally, some medical conditions, like heart disease, diabetes and depression may also be linked to Epilepsy.
- Basic Lab Studies
- Complete Blood Count
- Comprehensive metabolic panel
- Consider lumbar puncture and Torch titers if there are infectious concerns

Meningitis is a Condition that Causes inflammation of the Meningitis, which are the layers of Protective tissues that surround your brain and Spinal Cord. A few Pathogens can cause meningitis, Such as bacteria, Fungal, or viral Infections. This can happen through metabolic causes also, if we see from the upper side, it can be nutritious.
The Majority person with metabolic epilepsy present with symptoms in infancy or early childhood, which often include seizures typically with each symptom such as:
Delayed Development or loss of skills.
Abnormal movements
Problems with other body organs such as liver or kidneys.
Risk Factors
Features of genetic
Head injuries
1. Bad Habits
2. Body Strain
3. Tumors, benign & malignant
4. Infection diseases of the brain
5. Anomalies of the gestation period, cognitive Pathology
6. Birth trauma
7. Feverish Conditions
8. Metabolic disorders
The Risk Factors are quite like the factors of Epilepsy.
Characteristics
Fits can Vary in duration, intensity and duration
Symptoms may include loss of consciousness, muscle jerking, or conclusions, sensory changes, emotional alterations and cognitive impairments.
Understand the common causes and risk factors is crucial for identifying potential triggers
And it helps in developing appropriate management strategies.
Connections with other diseases:
Epilepsy can be associated with other neurological conditions such as migraine, autism spectrum disorder, cerebral palsy, and neurodevelopmental disorders.
Additionally, some medical conditions, like heart disease, diabetes and depression may also be linked to Epilepsy.
- Basic Lab Studies
- Complete Blood Count
- Comprehensive metabolic panel
- Consider lumbar puncture and Torch titers if there are infectious concerns

Imaging:
- MRI
- Ultrasound or CT if MRI not available
EEG:
- Urgent EEG, with LTM if possible
- Pyridoxine challenge
- Pyridoxal phosphate
- Folinic acid
Second Tier Texts
- Metabolic Screening
- Specific tests for treatable epilepsy
- Syndromes
- Genetic testing
- Cerebrospinal fluid/ serum glucose
This is Diagnosis

- Electroencephalogram (EEG)
Understanding involves unravelling the complexity of its mechanisms.
Medical Professionals rely on Diagnostic tests
They are EEG for epilepsy and brain imaging.
It’s to diagnose and classify types accurately.
So, this are the Neurological imaging studies
- Magnetic Resonance Imaging (MRI)
- Functional MRI (fMRI)
- Computed Tomography (CI)
- Positron Conclusion Tomography (PET)
- Single – Phelon Conclusion Computerized tomography (SPECT)
Understanding the Symptoms of Epilepsy: A Staged Approach
Epilepsy, a neurological disorder characterized by recurrent, unprovoked seizures, affects millions worldwide. The symptoms of epilepsy can vary widely among individuals, depending on the type of seizure and the area of the brain involved. To better understand and recognize epilepsy, it is helpful to consider the symptoms as they often unfold in successive stages. These stages, from initial harbingers to the post-seizure phase, provide insight into the complex nature of this condition.
- Harbingers: The Warning Signs
The onset of an epileptic episode is often preceded by certain warning signs, known collectively as harbingers. These early symptoms are not necessarily specific to epilepsy but can signal an impending seizure. Individuals may experience a range of sensations, including headaches, a pervasive feeling of discomfort, irritability, or even subtle changes in mood or sensation. These harbingers serve as the body’s preliminary alert, suggesting that something unusual is happening within the brain’s electrical activity.
2. Aura: The Prelude to a Seizure
Following the initial harbingers, some individuals encounter what is known as an aura. This phase can be considered both a warning sign and a part of the seizure itself, particularly for focal seizures that start in one area of the brain. Auras are often sensory or emotional in nature and can include hallucinations, such as seeing, hearing, or smelling things that are not present. Some people may experience a sudden wave of fear, happiness, or even déjà vu. The aura phase offers a crucial window, allowing some individuals to prepare for the possibility of a full-blown seizure.
3. The Tonic Phase: Loss of Consciousness
The seizure typically intensifies with the onset of the tonic phase. During this stage, the body’s muscles suddenly contract, causing a stiffening effect, particularly in the arms, legs, and back. This phase is marked by the loss of consciousness, which occurs as the excessive electrical discharge spreads throughout the brain, disrupting normal functions. The tonic phase is often brief but signals the transition to more noticeable and severe seizure activity.
4. Clonic Phase: The Convulsive Seizure
Following the tonic phase, the individual enters the clonic phase, where the classic symptoms of a convulsive seizure become apparent. This stage is characterized by rhythmic, jerking movements of the muscles, resulting from rapid contractions and relaxations. These convulsions are what most people associate with epilepsy. The clonic phase can vary in duration and intensity, and it is during this time that the risk of injury can be highest due to the uncontrollable nature of the movements.
Understanding Partial Seizures: A Closer Look at Simple Partial Seizures
Partial seizures, now more commonly referred to as focal seizures, represent a significant portion of epileptic episodes, affecting approximately 80% of patients with epilepsy. These seizures are characterized by their origin within one hemisphere of the brain, unlike generalized seizures that affect both hemispheres. Among partial seizures, simple partial seizures stand out for their distinct feature: they do not cause loss of consciousness. Understanding simple partial seizures is crucial for patients and caregivers alike to manage epilepsy effectively.
What Are Simple Partial Seizures?
Simple partial seizures, also known as focal onset aware seizures, involve brief episodes where seizure activity is limited to a specific area of the brain. Despite the abnormal electrical activity, individuals remain conscious and aware throughout the episode. These seizures can manifest in various forms, depending on the brain area affected, and typically last less than a minute.
These are the Signs & Symptoms:
- Motor – convulsive jerking, chewing motions, Lip Smacking
- Sensory & somatosensory – Paresthesia, auras
- Automatic – sweating, Flushing, pupil dilation
- Behavioral – Hallucinations, dysphasia, impaired consciousness(rare)
The complex partial seizures are :
- Impairment of Consciousness
- Purposeless behavior is common
- Affected person may wander about aimlessly
- Aggressive behavior
- Automatism
- Visual, auditory, or olfactory hallucinations
The Focal Seizures nerve cell Participate, also can be divided into the following categories:
Simple partials (aura): A common symptom of such seizures is anxiety, smelling extraneous odors, and seeing spots before the eyes, By the aura, many patients determine the proximity of an attack and manage to take measures so as not to be injured in the event of a fall.
Complex partial (psychomotor or temporal lobe epilepsy)
The attack proceeds in 3 phases.
In the first stages, the patient stops his activity for a few seconds.
Then the aimless action begins: a person can take off or put on clothes, unfasten and fasten buttons, fiddle with fingers, smack his lips.
In the third phase, consciousness returns but is still confused.
After a short period of disorientation, the person may resume the activity.
Generalized seizures:
1. Affecting both hemispheres
2. Diffuse
There are 3 types:
1 Idiopathic epilepsies
- Age Related
- Genetic Origin
- Symptomatic epilepsies
- A consequence of a known / suspected Underlying disorder of CNS
- Cryptogenic epilepsies
- Disorder of a hidden course
- Age related
The Absence Seizures are:
- Alterations of consciousness lasting for 10-30 sec
- Staring & loss in Postural tone
- 100 or more daily
- Onset occurs from 3-16 yrs., and disappears by 40 yrs.
Myoclonic: sudden, Involuntary jerking of facial, Limb or trunk muscles in a rhythmic manner.
Clonic: sustained muscle contractions alternating with relaxations.
Tonic: sustained muscle stiffening
The tonic- clonic phase of seizure are:

Tonic Phase
- Sudden Muscle Stiffness: The body, arms, and legs suddenly become extremely stiff. This stiffness is due to the muscles contracting forcefully and simultaneously.
- Loss of Consciousness: The individual loses consciousness rapidly as the seizure begins, which prevents them from remembering the episode afterward.
- Falling: Due to the loss of muscle control and consciousness, the person often falls to the ground if they were standing when the seizure started.
- Cry or Groan: A cry or groan may be heard at the onset, caused by the forceful exhalation of air from the lungs as the muscles around the ribcage contract.
- Breathing Difficulties: Breathing may become irregular or stop for a short period during the tonic phase, leading to cyanosis (bluish tint to the skin, especially around the lips) due to the lack of oxygen.
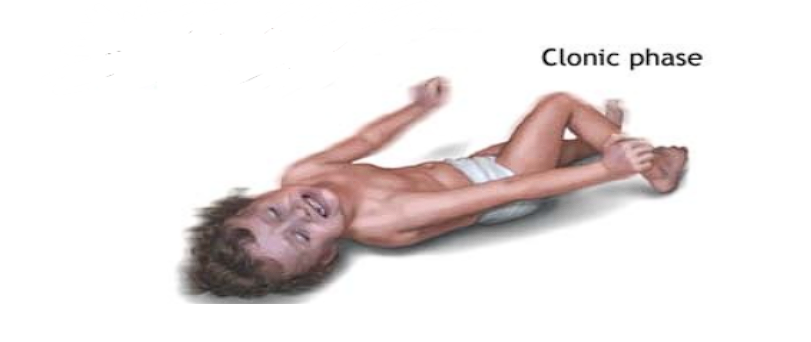
Clonic Phase
- Rhythmic Jerking: Following the tonic phase, the body begins to jerk rhythmically as muscles contract and relax rapidly. These movements are usually more pronounced in the arms and legs.
- Foaming at the Mouth: Saliva may accumulate and foam at the mouth due to the combination of rapid breathing, excessive salivation, and the inability to swallow.
- Biting of the Tongue or Cheek: The intense muscle contractions can cause the person to bite their tongue or cheek accidentally.
- Incontinence: Loss of bladder or bowel control may occur during this phase, adding to the distressing nature of the seizure.
During postictal phase: Headache, confusion, nausea, drowsiness this are symptoms may last for hours.
The Atonic (drop Attacks) signs are
Sudden loss of postural tone,pt falls to the ground and mostly occur primarily in children. The Unclassified Seizures are Neonatal which includes Status Epilepticus; Seizure occurs repeatedly with No recovery of the consciousness b/w attacks.
Exploring the Brain’s Complex Landscape: A Guide to Its Four Major Lobes
The Frontal Lobe: The Center of Decision-Making
Occupying the front part of the brain, the frontal lobe is vital for cognitive functions such as decision-making, problem-solving, and planning. It oversees our ability to recognize future consequences resulting from current actions, choose between good and bad actions, and suppress socially unacceptable responses. The frontal lobe also plays a crucial role in controlling movement and speech, as well as in managing emotions and personality. Impairments in this area can lead to significant changes in behaviour and personality, alongside difficulties with movement.
The Occipital Lobe: The Realm of Vision
At the brain’s rear is the occipital lobe, primarily dedicated to visual processing. This lobe receives and interprets information from the eyes, allowing us to understand shapes, colors, and distances. The occipital lobe’s ability to integrate visual data helps us navigate our environment safely and efficiently. Damage to this area can disrupt an individual’s ability to recognize objects, interpret visual stimuli, or can lead to visual impairments.
The Temporal Lobe: The Archive of Memory and Sound
Located beneath the temples, the temporal lobe is essential for processing auditory information from our ears. It is intricately involved in the formation of long-term memory and is a critical player in understanding language and speech production. The temporal lobe also processes information related to sensory input such as taste and smell. Disorders of the temporal lobe can manifest as difficulties in memory, speech, and understanding language.
The Parietal Lobe: The Hub of Sensation and Perception
Positioned between the frontal and occipital lobes, the parietal lobe integrates sensory information from various parts of the body, focusing on touch, temperature, and pain. It plays a significant role in spatial orientation and the coordination of movements. This lobe is where the brain interprets signals from the eyes and muscles to help us understand spatial relationships and navigate our surroundings. Damage here can lead to challenges with spatial awareness, hand-eye coordination, and the ability to perform tasks requiring fine motor skills.
The Seizure Types of Recurrence is 60% of the people with Epilepsy have Focal Seizures, 30% of the people with epilepsy have Generalized Seizures, 10% of have of Seizure have Unknown Onset.
Providing Support During a Seizure: A Simple Guide
Witnessing someone experience a seizure can be frightening, but knowing how to respond calmly and effectively can make a significant difference in ensuring their safety. Here are some simple steps to follow when assisting a person during a seizure episode:
- Stay Calm and Stay Safe
- Protect the Person from Injury
- Time the Seizure Note the start time of the seizure to help medical professionals later
- Position the Person Correctly
- Do Not Put Anything in the Person’s Mouth
- Stay with the Person Until They Recover
- After the Seizure
The Neuropathy Treatment:
- Dietary Changes
- Minerals and Vitamins
- Avoiding triggers
- Stress Relief
- Biofeedback
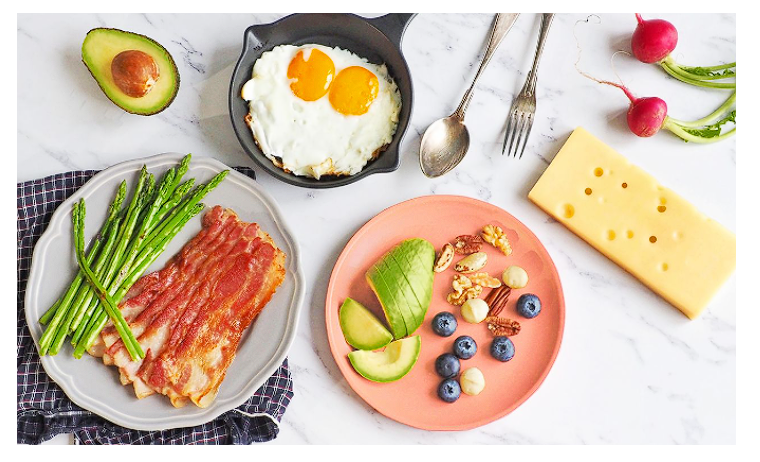
The Keto Diet
The ketogenic diet, or keto diet, has gained popularity in recent years for its potential health benefits and effectiveness in weight loss. This low-carbohydrate, high-fat diet is designed to induce a state of ketosis, where the body burns fat for fuel instead of carbohydrates. Here’s a simple guide to understanding the keto diet:
How It Works
The keto diet drastically reduces carbohydrate intake, typically to less than 50 grams per day. This forces the body to rely on fats for energy, which are broken down into ketones in the liver. These ketones serve as an alternative fuel source, especially for the brain, which normally relies heavily on glucose from carbohydrates.
Foods to Eat
The keto diet emphasizes foods that are high in fats and low in carbs, such as:
- Meat: Beef, poultry, pork, and lamb
- Fish: Salmon, tuna, trout, and mackerel
- Eggs: Preferably organic or pastured eggs
- High-fat dairy: Cheese, butter, and cream
- Nuts and seeds: Almonds, walnuts, chia seeds, and flaxseeds
- Healthy oils: Olive oil, coconut oil, and avocado oil
- Low-carb vegetables: Leafy greens, broccoli, cauliflower, and zucchini
Foods to limit or avoid on the keto diet include:
- Sugary foods: Soda, fruit juice, candy, and pastries
- Grains: Wheat, rice, and cereal
- Starchy vegetables: Potatoes, corn, and peas
- Fruit: Bananas, apples, and oranges (small portions of berries are acceptable)
- Processed foods: Chips, cookies, and processed meats
Benefits
The keto diet has been shown to have several health benefits, including:
- Weight loss: The diet’s high-fat, low-carb nature can lead to rapid weight loss, especially in the initial stages.
- Improved blood sugar control: The keto diet may help stabilise blood sugar levels and reduce insulin resistance.
- Enhanced mental clarity: Some people report improved focus and mental clarity when following a keto diet.
- Increased energy levels: Burning fat for fuel can lead to a more consistent energy supply throughout the day.
Neuropathic Approaches to managing Epilepsy
- Diet Modifications: Diet is a special high Fat, Low carbohydrate that helps to control Seizures in some people with epilepsy.
Exploring the Role of Vitamins in Managing Epilepsy
Epilepsy, a neurological disorder characterised by recurrent seizures, can be challenging to manage. While medications are often the primary treatment, research suggests that certain vitamins may play a role in reducing the frequency and severity of seizures in some individuals. Here’s a brief overview of vitamins that have shown promise in epilepsy management:
Vitamin B6 (Pyridoxine)
- Role in Epilepsy: Vitamin B6 is involved in the synthesis of neurotransmitters like serotonin and GABA, which play a role in regulating brain activity.
- Research: Studies have shown that supplementation with vitamin B6 may reduce the frequency and severity of seizures in some individuals, particularly in children with certain types of epilepsy.
- Caution: High doses of vitamin B6 can lead to nerve toxicity, so it’s essential to consult with a healthcare provider before starting supplementation.
Vitamin D
- Role in Epilepsy: Vitamin D is crucial for maintaining healthy bones and may also have anti-inflammatory and neuroprotective effects in the brain.
- Research: Some studies suggest that low levels of vitamin D may be associated with a higher risk of epilepsy and that supplementation may help reduce the frequency of seizures, especially in individuals with vitamin D deficiency.
- Caution: Excessive vitamin D supplementation can lead to toxicity, so levels should be monitored by a healthcare provider.

Harnessing Nature’s Bounty: Herbs Used in Epilepsy Management
For centuries, traditional medicine has turned to nature for remedies to various ailments, including epilepsy. While modern medicine remains the primary treatment for epilepsy, some herbs have shown promise in managing the condition.
Lavender (Lavandula angustifolia)
- Role in Epilepsy: Lavender is known for its calming and soothing properties, which may help reduce stress and anxiety, common triggers for seizures.
- Research: Some studies suggest that inhaling lavender essential oil may reduce the frequency of seizures in individuals with epilepsy, although more research is needed to confirm these findings.

Managing Seizure Triggers: A Guide to Prevention
Seizures, episodes of abnormal electrical activity in the brain, can be triggered by various factors. While triggers vary from person to person, understanding and managing these triggers can help reduce the frequency and severity of seizures. Here’s a brief overview of common seizure triggers and strategies for prevention:
1. Lack of Sleep
- Prevention: Maintain a regular sleep schedule, aiming for 7-8 hours of sleep per night. Avoid caffeine and electronic devices before bedtime.
2. Stress and Anxiety
- Prevention: Practice stress-reducing techniques such as yoga, meditation, deep breathing exercises, or hobbies that promote relaxation.
3. Alcohol and Substance Use
- Prevention: Avoid excessive alcohol consumption and recreational drug use, as these can lower the seizure threshold.
4. Flashing Lights (Photosensitivity)
- Prevention: For individuals with photosensitive epilepsy, avoid exposure to flashing or flickering lights, such as strobe lights and certain video games.
5. Missed Medications
- Prevention: Take prescribed anti-seizure medications regularly and on time. Use reminder apps or pillboxes to help remember doses.
6. Certain Foods and Food Additives
- Prevention: Identify and avoid foods that may trigger seizures, such as those containing MSG or artificial sweeteners.
- Hormonal Changes
- Prevention: Maintain a healthy lifestyle with regular exercise and balanced nutrition to help stabilize hormonal fluctuations.
8. Overheating
- Prevention: Stay cool in hot environments and avoid prolonged exposure to high temperatures.
9. Illness and Fever
- Prevention: Maintain a healthy immune system through regular handwashing, vaccinations, and staying home when sick to reduce the risk of infections that can lead to fever.
10. Certain Medications
- Prevention: Work with healthcare providers to find alternative medications if current medications are known to lower the seizure threshold.
Acupressure Points for Epilepsy
While there is limited scientific research on acupressure for epilepsy, some practitioners suggest focusing on acupressure points that promote relaxation and reduce stress, as stress is a common trigger for seizures. These points include:
- Third Eye Point (GV24.5): Located between the eyebrows, this point is believed to help calm the mind and relieve stress.
- Union Valley (LI4): Found between the thumb and index finger, stimulating this point is thought to promote relaxation and reduce anxiety.
- Heart 7 (HT7): Located on the wrist, this point is believed to help calm the mind and improve sleep quality.
Natural Treatment may complement your medical treatment. In some cases, these therapies may even improve your treatment.