Eye Diseases
Eye Diseases and Naturopathic Approaches
Eye health is a critical area of focus, as there are numerous diseases that can affect vision. In today’s lecture, we will concentrate on three specific and commonly encountered eye conditions. While naturopathy may not provide a cure for all eye diseases, it emphasizes understanding the root cause of a condition.
The naturopathic approach involves:
- Nutrition: Ensuring a diet that supports eye health.
- Lifestyle Management: Incorporating healthy daily habits to prevent or slow disease progression.
- Sleep Patterns: Maintaining adequate and quality sleep for optimal eye function.
- Naturopathic Therapies: Utilizing specific treatments suitable for conditions such as glaucoma, night blindness, color blindness, and general vision impairment.
Through these approaches, students will learn how to apply naturopathic principles effectively, with specific guidance provided during the lecture.
By combining scientific understanding with practical therapies, Saffron Educational and Medical Foundation empowers students to take control of their health while gaining insight into disease prevention and management through natural methods.
Understanding the Importance of Eye Health: A Focus on Glaucoma, Night Blindness, and Color Blindness
Today, we focus on three common eye conditions: glaucoma, night blindness, and color blindness. But before delving into the specifics, it’s important to reflect on the immense value of our eyes.
Imagine a life without vision. Ask anyone who is blind, and they will tell you how much they miss the beauty of the world around them. Vision is a gift from nature and, in many ways, one of the most precious senses we possess. While people often focus on external aspects such as hair, skin, or physical appearance, we frequently overlook the importance of eye health.
Many individuals begin experiencing eye problems with age, and unfortunately, some may lose their vision entirely. The inability to see affects every aspect of life, making even simple tasks challenging. While losing a finger or having minor physical impairments may impact life, loss of sight is life-altering, affecting independence and overall quality of life.
As natural therapists, it is our duty to assess the overall health of a patient, including understanding how much care they take of their eyes. Often, patients admit that they give very little attention to eye care, which is a concerning trend. Awareness and education about eye health, even among family members, is essential.
We are fortunate to have vision, whether aided by spectacles or naturally, and we must use and protect it. Additionally, if possible, consider eye donation after life. Eye donation is a simple yet powerful way to help someone experience the world visually. For example, Ms. World Pigeon of India pledged to donate her eyes to help others see the beauty of life, inspiring awareness and encouraging many people to follow suit.

Structure and Function of the Eyes
Before discussing eye diseases, it’s important to understand the structure and function of the eyes. The primary function of the eyes is to allow us to see objects in our surroundings at variable distances and under different lighting conditions. Our ability to perceive colors, depth, and motion is achieved through a complex arrangement of layers and structures within the eye. While eyes may seem simple at first glance, they consist of multiple layers and components that work together to create vision.
Understanding the importance of eye health and its complex structure is the first step in preventing diseases such as glaucoma, night blindness, and color blindness. Proper care, nutrition, and awareness can go a long way in maintaining good vision throughout life.
Understanding the Eye Structure and Common Eye Diseases: Focus on Glaucoma
Before diving into eye diseases, it is essential to understand the basic structure of the eye. While a detailed study of the eye is a complex topic often reserved for ophthalmologists, there are three fundamental layers that form the foundation of vision:
- Outer Layer – Sclera:
The outermost layer, known as the sclera, is the white protective coating of the eye. It provides structural support and safeguards the internal components of the eye. - Middle Layer – Choroid:
The choroid lies beneath the sclera and contains blood vessels that nourish the eye. Proper blood circulation is critical for eye health, and irregularities may contribute to conditions such as ocular hypertension. Eye specialists often check for this during routine examinations. - Inner Layer – Retina:
The retina is the innermost layer containing nerve cells that transmit visual information to the brain. This layer allows us to perceive images, colors, and depth.
In addition to these three layers, several other structures play a vital role in vision:
- Cornea: A clear, dome-shaped surface at the front of the eye that helps focus light.
- Iris: The colored portion of the eye, composed of spongy tissue, which regulates the amount of light entering the eye.
- Pupil: A black circular opening in the iris that allows light to pass through.
- Lens: Focuses incoming light onto the photoreceptors in the retina, enabling clear vision.
- Photoreceptors: Specialized cells in the retina that detect light and color, allowing the brain to form visual images.
Together, these components allow us to experience the world in clarity and color. However, neglecting eye health can lead to common visual problems such as blurred vision or weak eyesight.
Glaucoma: A Leading Cause of Blindness
Among the various eye diseases, glaucoma is one of the most significant and preventable causes of blindness worldwide. It is the second leading cause of blindness, following cataracts.
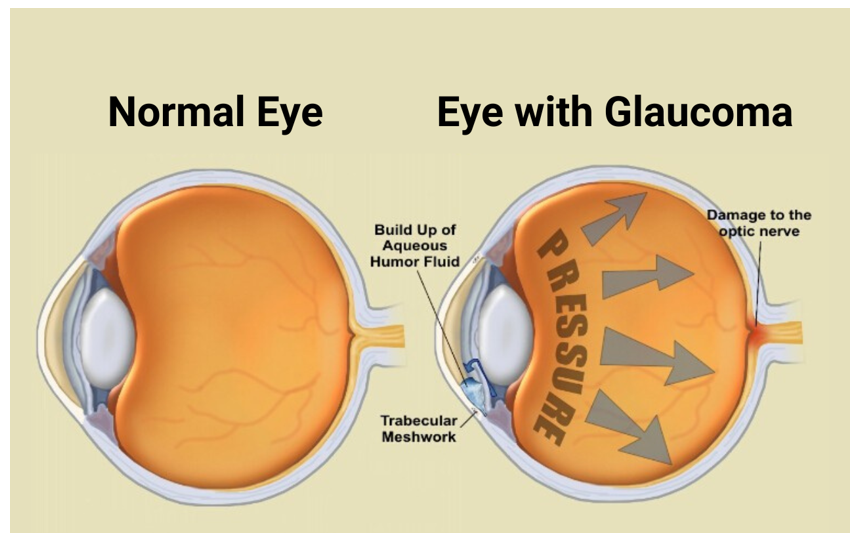
Glaucoma is not a single disease but a group of eye disorders that damage the optic nerve, often due to increased intraocular pressure. This damage is progressive and can eventually result in complete blindness if left untreated.
Symptoms may develop gradually, and early-stage glaucoma often goes unnoticed. Therefore, it is crucial for anyone experiencing blurred vision, reduced clarity, or other visual disturbances to consult an eye specialist immediately. Early diagnosis and management can prevent further damage and preserve vision.
By understanding the eye’s structure and the risks associated with diseases like glaucoma, individuals can take proactive steps in maintaining eye health and protecting one of nature’s most precious gifts.
Glaucoma: Understanding Its Causes, Symptoms, and Diagnosis
Our eyes are incredibly delicate and sensitive organs. Even a small particle, such as a hair or dust, can cause intense discomfort and irritation. Most people can relate to the experience of having something in the eye: it can distract you completely, making it impossible to focus on anything else until the foreign particle is removed. If such minor disturbances can have a strong impact, imagine the effect of serious eye diseases.
It is essential to pay attention to even minor visual disturbances. Any discomfort, blurred vision, or difficulty seeing should prompt an immediate eye checkup. Early diagnosis is crucial, as proper treatment is only possible once a specialist has identified the underlying problem. After diagnosis, individuals may consult a natural or alternative therapist, but the first step must always be medical evaluation.
What Is Glaucoma?
Glaucoma is a group of eye diseases that cause progressive damage to the optic nerve, potentially leading to vision problems or complete blindness. One of the challenges with glaucoma is that early stages often show no noticeable symptoms, making regular eye examinations essential.
The primary cause of glaucoma is the excessive secretion of aqueous humor, a fluid produced in the eye that helps maintain clarity and pressure. Normally, aqueous humor circulates freely, but when its quantity becomes excessive, it can create blockages, increasing intraocular pressure. This pressure damages the optic nerve over time, gradually reducing vision clarity and, in severe cases, resulting in permanent blindness.
Symptoms to Watch For
In the early stages, glaucoma may go unnoticed. Common warning signs include:
- Blurred or hazy vision
- Difficulty focusing
- Seeing optical distortions or “phantom” particles in front of the eyes
If any of these symptoms appear, it is the right time to consult an eye specialist.
How Glaucoma Is Diagnosed
Eye specialists check for glaucoma by measuring intraocular pressure (IOP), a method similar to checking blood pressure. The normal range of eye pressure is typically less than 21 mmHg. If the pressure is within this range, maintaining regular eye care—such as washing the eyes, using eye cups, and protecting the eyes—is generally sufficient.
When eye pressure rises above 25 mmHg, glaucoma may be diagnosed. There are different types of glaucoma, each with specific characteristics:
- Congenital Glaucoma: Present from birth, this type involves an intraocular pressure above 21 mmHg, changes in optic disc appearance, and defects in visual fields caused by excessive aqueous humor secretion.
Other types of glaucoma are also recognized, but congenital glaucoma serves as an important example of how increased eye pressure can damage vision from an early stage.
Types of Glaucoma: Causes, Classifications, and Risk Factors
Glaucoma is a complex group of eye diseases that can cause progressive damage to the optic nerve and vision loss. Understanding the different types of glaucoma and their causes is crucial for prevention, early detection, and proper treatment.
Congenital Glaucoma
Congenital glaucoma refers to glaucoma present at birth or developing during early childhood. It is typically classified based on the age of onset:
- Childhood (Infantile) Glaucoma: Detected within the first three months of life, often due to developmental issues during pregnancy.
- Infantile Glaucoma: Occurs from three months up to three years of age.
- Juvenile Glaucoma: Manifests between three years and 40 years of age.
- Adult Congenital Glaucoma: Diagnosed after the age of 40.
Congenital glaucoma can also be categorized into primary and secondary forms. Primary congenital glaucoma arises from developmental anomalies of the eye’s drainage system, while secondary congenital glaucoma results from other causes such as trauma, neovascular problems, lens abnormalities, steroid-induced complications, or pigmentary disorders.
Among these, childhood and adult congenital glaucoma are the most commonly observed, while infantile and juvenile cases are relatively rare.
Open-Angle and Closed-Angle Glaucoma
Glaucoma is largely determined by the secretion and drainage of aqueous humor, the fluid within the eye. Depending on how this fluid affects intraocular pressure, glaucoma can be classified as:
- Open-Angle Glaucoma:
This is the most common type. Excess aqueous humor is produced, but the drainage angle remains open. The increased fluid raises intraocular pressure slowly, often without noticeable early symptoms. - Closed-Angle (Narrow-Angle) Glaucoma:
When excessive aqueous humor causes the drainage angle to become blocked or narrowed, the flow of fluid is restricted. This results in a rapid increase in eye pressure, potentially leading to sudden vision loss. The mechanism is similar to the way arterial circulation is affected by cholesterol buildup, which narrows blood vessels and restricts flow.
Secondary Glaucoma
Secondary glaucoma develops due to other underlying conditions or external factors. Common causes include:
- Trauma or injuries to the eye
- Neovascular problems (abnormal blood vessel growth)
- Lens abnormalities
- Steroid-induced glaucoma
- Mechanical or genetic abnormalities of the eye’s drainage system
- Eye infections or hemorrhage
Among these causes, diabetes mellitus is a particularly significant risk factor. Patients with poorly controlled blood sugar levels (high HbA1c) are at an increased risk of developing glaucoma. Studies indicate that approximately 30% of diabetic patients may experience glaucoma-related complications.
Causes and Risk Factors of Glaucoma: The Role of Diabetes, Hypertension, and Migraine
Glaucoma is a multifactorial eye disease, and understanding its root causes is essential for prevention and effective management. Among the most common triggers, diabetes mellitus, hypertension, genetics, and lifestyle factors play significant roles.
Diabetes and Glaucoma
Poorly controlled blood sugar is one of the leading causes of glaucoma. Studies indicate that approximately 30% of glaucoma cases are linked to diabetes, especially in individuals with high HbA1c levels or uncontrolled glucose. For diabetics, maintaining blood sugar within the normal range is crucial—not just for protecting the heart, liver, and kidneys, but also to safeguard eye health.
Key Point: Proper glucose control can significantly reduce the progression of glaucoma. In many cases, stabilizing blood sugar levels minimizes optic nerve stress and intraocular pressure, helping prevent further vision loss.

Hypertension and Lifestyle-Related Causes
High blood pressure is another common contributing factor to glaucoma. Hypertension and diabetes are reversible risk factors, meaning that by managing these conditions, glaucoma progression can often be controlled.
Management Approach:
- Monitor and regulate blood pressure regularly
- Maintain a healthy lifestyle, including diet and exercise
- Address underlying root causes before focusing solely on glaucoma treatment
By controlling the root causes, such as blood sugar and blood pressure, the excessive secretion of aqueous humor—the fluid responsible for increased intraocular pressure—can be minimized, slowing the progression of glaucoma.
Other Causes of Glaucoma
Several additional factors can contribute to glaucoma, including:
- Eye Trauma and Injuries: Certain types of ocular trauma or exposure to harmful light may trigger glaucoma.
- Ocular Surgeries: While not common, some surgeries or complications from medications can increase the risk of glaucoma.
- Migraine: Chronic migraines, often overlooked as a cause, can damage the optic nerve. During a migraine, high intraocular pressure and restricted circulation can stress the optic nerve, making migraine sufferers more susceptible to glaucoma. Unlike occasional headaches, chronic migraines may have lasting effects on eye health if left unmanaged.
Key Takeaways
- Early Detection Is Critical: Even minor vision disturbances should prompt an eye examination.
- Control Root Causes: Managing diabetes, hypertension, and chronic migraines can reduce the risk and progression of glaucoma.
- Ongoing Monitoring: Individuals with these risk factors should regularly check intraocular pressure and consult an eye specialist to prevent irreversible damage.
By understanding and addressing the causes of glaucoma, individuals can take proactive steps to protect their vision and maintain healthy eyes throughout life.
Glaucoma: Symptoms, Warning Signs, and Early Detection
Glaucoma is a progressive eye disease that can cause permanent vision loss if left untreated. While some causes, like genetics, cannot be changed, many risk factors are reversible, including diabetes, hypertension, chronic migraines, and lifestyle-related factors. Understanding the signs and symptoms of glaucoma is essential for early detection and management.
The Vicious Cycle: Migraine and Glaucoma
Chronic migraines can contribute to glaucoma by increasing intraocular pressure and restricting circulation to the optic nerve. Over time, this creates a vicious cycle, as migraines exacerbate eye pressure, which in turn can worsen glaucoma. Proper management of migraines, including medical treatment and lifestyle adjustments, can reduce this risk and help protect vision.
Other Contributing Factors
Several additional factors may increase the risk of glaucoma:
- Prolonged steroid use or certain ocular medications
- Ocular surgeries, especially if complications arise
- Eye trauma or injuries
- Diabetes mellitus and hypertension, which are among the most common reversible causes
By addressing these underlying factors, it is often possible to stop further damage and, in some cases, partially restore vision.
Common Signs and Symptoms
Glaucoma may develop gradually, and in many cases, early symptoms are subtle. Key warning signs include:
- Mild Eye Pain or Discomfort
Pain may be mild and intermittent, often noticed while blinking, waking up, or after prolonged focus on tasks such as reading or writing. Continuous eye strain from activities like excessive screen time can also contribute. - Redness of the Eyes
Persistent redness not explained by infection, injury, or lack of sleep may indicate underlying eye pressure issues. - Blurred Vision
Difficulty seeing objects clearly, even after cleaning glasses or correcting refractive errors, can signal vision impairment related to glaucoma. - Difficulty with Color Perception
Problems distinguishing colors may indicate associated conditions such as color blindness or night blindness. - Photophobia (Light Sensitivity)
Sensitivity to light, often experienced during migraine attacks, can accompany glaucoma symptoms. - Other Signs
- Nausea and vomiting (common in migraine-related glaucoma cases)
- Swelling of the cornea (corneal edema)
- Pupil dilation abnormalities
Importance of Early Detection
If any of the above signs are present, it is critical to consult an eye specialist immediately. Early diagnosis allows for appropriate management, preventing irreversible optic nerve damage and preserving vision.
How Glaucoma Is Diagnosed
Eye specialists use a combination of ocular history, instrumental tests, and clinical examination to diagnose glaucoma. Common diagnostic techniques include:
- Measuring intraocular pressure (tonometry)
- Visual field assessment
- Ophthalmoscopy to examine the optic nerve
- Other advanced imaging methods as required
Through careful evaluation, specialists can detect glaucoma early and recommend appropriate medical, lifestyle, or therapeutic interventions to slow or halt disease progression.
Glaucoma Management and Complementary Therapies: A Holistic Approach
Glaucoma is primarily diagnosed and managed by eye specialists using precise instruments and tests such as:
- Visual field assessment
- Tonometry (measuring intraocular pressure)
- Slit lamp examination
These diagnostic procedures help ophthalmologists determine the stage and severity of glaucoma. They then develop a treatment plan tailored to the patient’s needs. Standard medical management often includes eye drops or medications, such as beta-blockers, to control the excessive secretion of aqueous humor and reduce intraocular pressure. These interventions aim to preserve vision and prevent further optic nerve damage.
Role of Alternative Therapies
While diagnostic tests and medications are essential, complementary therapies can support eye health, improve circulation, and reduce stress on the eyes. One of the most effective holistic approaches is breathing-based oxygen therapy.
Oxygen Therapy and Eye Health
Deep breathing exercises increase oxygen levels in the blood, which enhances circulation throughout the body, including the eyes and optic nerves. Improved blood flow ensures that the eyes receive sufficient oxygen and nutrients, which supports eye function and may help slow disease progression.
Recommendations:
- Practice deep breathing exercises for 20 minutes daily
- Adjust the method according to comfort and health conditions
- Maintain overall oxygenation for hemoglobin efficiency and blood health
Mud Therapy for Eyes
Another traditional therapy used to support eye health is mud therapy. This involves:
- Soaking black deep-sea mud (or similar therapeutic mud) overnight in a clean container.
- Spreading a half-inch layer of mud on a white cotton cloth to create a simple pad.
- Placing the mud pad gently over closed eyes while lying down for 20 minutes daily.
This therapy is believed to relieve eye strain, reduce fatigue, and improve local circulation, complementing medical and lifestyle interventions.
Integrating Approaches
It is important to note that complementary therapies do not replace medical treatment. They are most effective when used alongside proper diagnosis, medication, and lifestyle management. Early detection and medical oversight are essential, while holistic practices like oxygen therapy and mud therapy can provide supportive care and overall eye wellness.
Holistic Approaches to Eye Health: Sleep, Nutrition, and Alternative Therapies
Maintaining healthy eyes goes beyond medical treatments and requires lifestyle adjustments, proper nutrition, and supportive therapies. While glaucoma and other eye conditions require professional diagnosis and management, there are several complementary measures that can help maintain vision and prevent further deterioration.
Mud Therapy for Eyes
One traditional supportive therapy is mud application. This therapy does not require a specific time of day; what is essential is a lying-down position while the mud is applied over the closed eyes. The steps are simple:
- Use black deep-sea mud or similar therapeutic mud.
- Spread a half-inch layer of mud on a white cotton cloth.
- Place the mud pad over closed eyes for approximately 20 minutes.
For detailed guidance, pre-recorded video sessions are available, showing the correct preparation and application. This therapy helps relieve eye strain and improve local circulation.
Importance of Sleep
Adequate sleep is critical for eye health. During sleep, the body undergoes regeneration, detoxification, and tissue repair. Proper sleep ensures:
- Reduced ocular pressure
- Relaxation of eye muscles
- Improved blood circulation around the eyes
A well-maintained biological clock ensures that internal organs, including the eyes, function optimally. Disruption of sleep patterns or insufficient rest can exacerbate eye problems.
Acupressure and Acupuncture
Alternative therapies like acupressure and acupuncture are also effective for eye care. These techniques can:
- Reduce eye strain
- Improve blood flow to ocular tissues
- Potentially decrease dependency on corrective lenses for some patients
Modern research has validated these methods as supportive approaches for maintaining eye health.
Nutrition for Healthy Eyes
Diet plays a pivotal role in preventing and managing eye conditions. Vitamin A is especially important for vision, and natural sources are abundant:
- Carrots – Fresh juice or organic carrot powder is highly beneficial.
- Yellow and orange fruits – Apricots, papayas, peaches, and mangoes.
- Yellow and orange vegetables – Pumpkins, sweet potatoes.
- Nuts – Almonds and pistachios, providing protein, vitamins, and antioxidants.
- Green leafy vegetables – Spinach and kale, rich in lutein and other nutrients.
- Non-vegetarian sources – Egg yolks, salmon, tuna, and mackerel, which are excellent sources of Vitamin A and protein.
Including these foods regularly supports retinal health, protects against oxidative stress, and strengthens the optic nerves. For individuals with hypertension or diabetes, these foods also help in maintaining blood sugar and overall health, indirectly benefiting vision.
Holistic Therapies and Dietary Support for Eye Health
Maintaining optimal eye health involves a combination of nutrition, lifestyle practices, and supportive therapies. Both non-vegetarians and vegetarians have multiple options to ensure their diet supports healthy vision.
Dietary Recommendations
For non-vegetarians, including seafood such as salmon, tuna, or mackerel in the diet can provide essential Vitamin A and protein to support retinal function and overall eye health. Vegetarians, on the other hand, have access to a variety of options including:
- Orange and yellow fruits: Carrots, apricots, papayas, mangoes, peaches
- Vegetables: Pumpkin, sweet potatoes
- Nuts: Walnuts and almonds
Incorporating these foods regularly into meals provides nutrition that supports eye function and helps prevent vision problems. These foods also contribute to general health, making them a cornerstone of both naturopathic and holistic approaches.
Naturopathic Therapies
Several simple naturopathic therapies can complement a healthy diet:
- Nasal therapy with cow ghee: Placing 3–4 drops of pure cow ghee in each nostril before bedtime can support ocular health. This method is completely safe and free of side effects. Cow ghee is not only beneficial for the eyes but also boosts immunity and metabolism.
- Magnet therapy for the feet: At Saffron, patients have benefited from magnetized cow ghee applied to the feet using a bronze tool. The treatment involves rubbing the feet for five minutes each night, leveraging acupressure points on the feet. This therapy helps improve circulation from head to toe, indirectly supporting eye health.
- Daily “charging” analogy: Just as mobile phones require daily charging, the body benefits from these therapies every day to maintain optimal circulatory function and eye health.

Importance of Nutrition and Supplements
While these therapies support eye health, nutrition is indispensable. Without proper dietary support, the benefits of therapies alone may be limited. Regular intake of vitamin A-rich foods, fruits, vegetables, and nuts ensures the retina receives essential nutrients, supporting visual clarity and overall eye function.
Night Blindness (Nyctalopia)
Night blindness, also called nyctalopia, is a vision problem primarily related to the retina. Although it is not considered a disease itself, it is a symptom indicating retinal dysfunction. Genetics plays a significant role, with nearly 100 defective genes potentially contributing to the condition. While night blindness does not lead to complete vision loss, it affects the ability to see in low-light conditions and should be addressed with dietary support and early intervention.
Night Blindness (Nyctalopia): Understanding the Causes and Symptoms
Night blindness, also known as nyctalopia, is a condition in which individuals have difficulty seeing in low-light or dark environments. It is important to note that night blindness does not cause complete loss of vision. Instead, it primarily affects the ability to perceive objects clearly in dim lighting.
Causes of Night Blindness
The underlying causes of night blindness are largely related to the retina, particularly the rod and cone cells.
- Rod cells: These are the primary cells affected in night blindness. Rods are responsible for detecting light and motion in low-light conditions. When rod function is impaired, it becomes difficult to see at night or in poorly lit areas.
- Cone cells: While rods are primarily affected, cones can also be gradually impacted, especially affecting color perception and vision during tasks like reading or writing.
Night blindness can arise due to several factors:
- Vitamin A deficiency: Vitamin A is essential for the production of rhodopsin, a pigment in the retina that helps rods detect light. A deficiency in vitamin A can severely impair night vision.
- Genetics: Hereditary factors can influence the structure and function of retinal cells, making some individuals more prone to night blindness.
- Cataracts: Clouding of the lens can block light from reaching the retina, reducing visibility in dim conditions. Cataracts cause the eye to appear whitish or cloudy, affecting night vision.
- Medications: Certain medications, especially those taken in the evening, can have side effects that impair night vision.
Signs and Symptoms
The symptoms of night blindness primarily revolve around difficulty seeing in low-light environments:
- Difficulty navigating in darkness or poorly lit areas
- Narrowed visual fields due to reduced retinal sensitivity
- Gradual decline in overall eyesight with age
- Dependence on artificial lighting for routine activities
Night blindness is more commonly observed in older adults, particularly those aged 50–60 and above, and is less frequently seen in younger individuals. The condition may worsen over time if proper eye care, nutrition, or management of underlying health conditions is neglected.
Night Blindness (Nyctalopia): Risks, Diagnosis, and Management
Night blindness, or nyctalopia, is a condition that affects the ability to see clearly in low-light or dark environments. While individuals are not completely blind, the condition can cause blurred and distorted vision in poor lighting, leading to difficulty in judging objects and navigating safely at night.
Risks and Safety Concerns
People with night blindness are prone to accidents due to impaired vision in darkness. For instance, difficulty in judging steps or obstacles at night can result in falls and injuries, making it essential for affected individuals to exercise caution in low-light conditions. Companionship or ensuring proper lighting when moving in the dark can help prevent accidents.
Symptoms
Key symptoms of night blindness include:
- Difficulty seeing objects in dim light
- Blurred or distorted vision in darkness
- Problems judging distances or shapes in low-light conditions
- Increased risk of falls or minor injuries due to impaired vision
Diagnosis
Night blindness can often be suspected based on symptoms, but medical diagnosis is essential for identifying the underlying cause. Common diagnostic methods include:
- Fundus photography: Imaging of the retina to detect abnormalities in rod and cone cells
- OCT (Optical Coherence Tomography) Angiography: Provides detailed images of retinal structures
- Electrophysiological tests: Measure the electrical activity of retinal cells
- Genetic blood tests: Detect defective genes, including X-linked and other retinal-related genes
- Routine blood tests: CBC and other panels can help assess hemoglobin, WBC count, and platelet levels
Although complete blindness due to night blindness is extremely rare (less than 0.5% of cases), early detection is crucial for proper management.
Treatment and Management
Management of night blindness depends on the underlying cause:
- Vitamin A supplementation: This is the most common and effective therapy for night blindness caused by vitamin A deficiency, as it is crucial for the production of rhodopsin in the retina.
- Cataract management: If clouding of the lens is contributing to poor night vision, addressing cataracts can improve visual clarity.
- Dietary modifications: Nutrient-rich foods can help prevent or mitigate night blindness. Recommended foods include:
- Green vegetables: Spinach, broccoli, green peas, capsicum, and other leafy greens
- Yellow and orange fruits and vegetables: Carrots, pumpkins, sweet potatoes, apricots, mangoes, papayas, and seasonal regional produce
- Dietary supplements: As discussed earlier, these can support overall eye health and prevent progression of night blindness
- Mud application therapy: Naturopathic techniques, including mud packs for the eyes, can support circulation and eye relaxation
- Routine and lifestyle adjustments: Following a consistent sleep schedule and maintaining overall health can positively impact eye function. Understanding the body’s biological clock can help optimize eye rest and recovery.

Eye Health, Nutrition, and Vision Disorders: Night Blindness and Color Blindness
Fasting and Digestive Rhythm for Eye Health
Our bodies operate according to an internal biological clock, and aligning food intake with this rhythm is essential for optimal health. Experts recommend giving the digestive system 12 to 14 hours of fasting each day. This fasting period allows the body to fully digest, absorb, and distribute nutrients into the bloodstream, supporting overall health, including eye function.
For example, it is advised to complete dinner before sunset, around 6:30 to 7:30 PM. By the next morning, after a glass of water or other light intake, this fasting period ensures that the digestive system works efficiently, supporting nutrient absorption, tissue regeneration, and detoxification. A disciplined eating schedule is crucial, especially for individuals with vision problems or other health concerns.
Night Blindness (Nyctalopia)
People with night blindness struggle to see clearly in low-light conditions. Unlike total blindness, night blindness primarily affects the ability to navigate and recognize objects in darkness. This can lead to blurred and distorted vision, making tasks such as walking at night or driving dangerous.
Key precautions for night blindness:
- Avoid driving or moving alone in dark areas.
- Ensure proper lighting at night to prevent accidents or falls.
Night blindness can result from retinal issues, vitamin A deficiency, cataracts, genetic factors, or medication side effects. Diagnosis may involve fundus photography, OCT angiography, electrophysiological testing, and blood tests for genetic analysis. Treatment includes dietary adjustments rich in vitamin A, mud eye applications, lifestyle management, and, in severe cases, modern therapies such as stem cell treatments.
Color Blindness (Defective Color Vision)
Color blindness is a vision condition that makes it difficult or impossible for a person to distinguish between certain colors. It is not complete blindness but rather an inability to perceive colors accurately, affecting daily activities and safety.
People with color blindness may struggle to identify:
- Traffic signals
- Colors of clothing, fruits, and vegetables
- Shades of buildings or natural objects
Types of color blindness:
- Red-green color blindness – difficulty distinguishing red and green shades.
- Blue-yellow color blindness – difficulty distinguishing blue and yellow shades.
- Complete color blindness – no perception of colors, with the world appearing in black, white, and gray tones.
Color blindness can be diagnosed through standard vision tests that involve identifying colors and shades on visual charts or signals. Understanding the type and severity of color blindness is essential for lifestyle adaptation and safety measures.
Integrating Nutrition, Lifestyle, and Eye Care
Eye health can be significantly improved by combining nutritional strategies, therapies, and lifestyle management:
- Follow a disciplined eating schedule in accordance with your body’s biological clock.
- Maintain proper fasting intervals to allow digestion, nutrient absorption, and regeneration.
- Adjust lifestyle activities, such as avoiding driving at night for those with night blindness.
- Include nutrient-rich foods (yellow and orange fruits and vegetables, leafy greens, nuts) to support eye health.
By combining nutrition, mindful living, and preventive strategies, individuals can support their vision and reduce the risk of complications from night blindness, color blindness, and other eye conditions.

Understanding Color Blindness: Signs, Symptoms, and Patient Care
Color blindness is a visual condition that affects a person’s ability to distinguish between certain colors, often leading to frustration, reduced confidence, and challenges in daily life. While the condition does not make someone completely blind, it can significantly impair their ability to perceive the world accurately.
How Color Blindness Affects Vision
Depending on the type of color blindness, individuals perceive the world differently:
- Red-green color blindness: Difficulty distinguishing between red and green shades.
- Blue-yellow color blindness: Difficulty recognizing blue and yellow hues.
- Complete color blindness: The entire world appears in black, white, and shades of gray.
Visual aids, such as color charts or objects with distinct color combinations, can help assess the degree of color blindness in patients. By asking individuals to identify colors of specific objects, practitioners can gain a preliminary understanding of the condition.
Key Signs and Symptoms
People with color blindness may experience:
- Inability to differentiate shades: Even subtle differences in colors may appear identical.
- Difficulty recognizing brightness: Objects may appear darker or less vivid than they actually are.
- Problems with distance perception: Identifying objects from afar can be challenging.
- Emotional impact: Frustration, depression, and loss of confidence are common due to the daily struggles in distinguishing colors.
Unlike total blindness, those with color blindness often have normal vision in daylight but face significant challenges in poor lighting or with certain color-dependent tasks.
Patient Approach and Counseling
When treating patients with color blindness, a therapeutic and supportive approach is critical:
- Build trust and confidence: The first step is to assure patients that their concerns are understood.
- Counseling over consultation: Focus on emotional support and guiding them through lifestyle or dietary adjustments rather than promising a cure.
- Set realistic expectations: Color blindness cannot be completely cured, but improvements in adaptation and perception can be achieved.
Many patients who seek alternative therapies, including naturopathy, often arrive frustrated after multiple failed treatments. They are usually well-informed through social media or online resources, which may lead to misconceptions or heightened expectations. Handling such patients requires patience, clear communication, and positivity, helping them feel supported and empowered.
Practical Tips for Managing Color Blindness
While color blindness cannot be fully reversed, patients can benefit from:
- Adaptive strategies: Using labeled items, apps, or assistive tools to identify colors.
- Nutrition and eye care: Maintaining a balanced diet rich in vitamins, especially vitamin A, to support overall eye health.
- Regular eye monitoring: Ensuring that other conditions like night blindness or retinal issues are managed concurrently.
By combining these strategies with counseling and confidence-building, patients can navigate daily life more effectively and reduce the emotional burden associated with color blindness.
Managing Color Blindness and Eye-Related Conditions Through Naturopathy
Color blindness and other eye-related conditions, such as night blindness or visual impairments, are not completely curable, especially when they are hereditary. However, patients can experience significant improvements in vision and quality of life through careful naturopathic management, counseling, and lifestyle adjustments.
Improvement Through Naturopathy
While naturopathy cannot fully cure color blindness, it offers several benefits:
- Enhanced confidence: Patients often overcome depression and anxiety associated with their condition.
- Symptom management: By addressing secondary health issues and improving lifestyle factors, patients experience better overall well-being.
- Supportive therapies: Mud applications, dietary changes, and other naturopathic interventions can contribute to partial improvements in visual function.
The goal of naturopathy in eye care is to improve patient comfort and adaptability, rather than promise a complete cure. Even minor improvements in vision and daily functioning can significantly boost a patient’s morale and confidence.
Counseling and Psychological Support
Patients with color blindness or night blindness often present with frustration, depression, and a sense of helplessness. A holistic approach focuses on:
- Lowering anxiety: Many patients also have hypertension or lifestyle-related conditions, which can exacerbate stress.
- Building trust: Active listening and understanding the patient’s concerns help create a therapeutic alliance.
- Tailored treatment: Every patient’s needs and responses are unique, requiring individualized approaches.
During the initial sessions, it is important to allow patients to express themselves fully. Many arrive after extensive conventional treatment, often frustrated and searching for alternative solutions. Listening without judgment is critical to foster trust and adherence to therapy.
Identifying Underlying Causes
Color blindness and related eye conditions may result from:
- Genetic factors: Hereditary retinal issues or defective genes.
- Systemic health problems: Conditions such as Parkinson’s, Alzheimer’s, or chronic medication use can contribute to visual difficulties.
- Psychosomatic influences: Stress, skin disorders, or other bodily imbalances may exacerbate symptoms.
Naturopathic therapy focuses on supporting the patient holistically, addressing coexisting health concerns while providing relief for the visual condition itself.
Diagnostic Approaches
While naturopathy does not involve surgical or invasive interventions, awareness of diagnostic methods helps practitioners guide and educate patients:
- Ishihara Test: Developed in Japan, this test includes 27 shades of colors displayed in circular, square, or triangular patterns. Patients identify specific colored dots or figures to determine the type and severity of color blindness.
- Transformation and Vanishing Plates: Additional visual assessments that help evaluate visual perception and color differentiation.
- Specialist Consultation: Eye specialists assess stage and severity, providing recommendations tailored to individual conditions.
High-Risk Groups
Certain professions, due to constant reliance on color differentiation, are more affected by color vision deficiencies:
- Pilots
- Traffic controllers
- IT professionals
- Railway operators
Understanding occupation-related risk factors can guide preventive strategies and adaptive support.
Key Takeaways for Naturopathic Management
- Complete cure is unlikely, but improvement in vision and quality of life is achievable.
- Counseling and psychological support are crucial components of therapy.
- Individualized approaches considering health status, occupation, and lifestyle maximize benefits.
- Dietary support, mud therapies, and lifestyle adjustments complement conventional recommendations to improve patient outcomes.
Naturopathy, while not a substitute for ophthalmic care, provides a safe and supportive pathway for patients seeking improvement in their visual conditions and overall well-being.
Managing Eye Health in High-Risk Professions: Naturopathic Approaches
Certain professions are particularly vulnerable to visual impairments, such as color blindness or night blindness, due to their working conditions and lifestyle demands. These include IT professionals, railway operators, local pilots, and commercial pilots.
Occupational Risk Factors
The following factors increase susceptibility to eye-related issues in these professions:
- Continuous screen exposure: IT professionals spend long hours sharing and viewing screens, which strains the eyes.
- Sedentary work: Railway operators and local pilots sit for extended periods with minimal physical activity.
- Environmental stressors: Pilots are exposed to low air pressure and long flight durations, often exceeding 15–20 hours.
- High alertness demands: Professions requiring constant vigilance are more affected by visual deficiencies.
The combination of these factors can aggravate color perception difficulties, reduce eye efficiency, and increase stress-related visual complaints.
Challenges and Limitations of Conventional Treatment
Currently, conventional medicine offers limited solutions for color blindness:
- Special lenses or filters: These can provide partial improvement in color differentiation.
- Chemical or dye-based lenses: May improve perception in some cases, but results are inconsistent.
It is important to note that genetic causes cannot be reversed, and conventional treatments do not offer a definitive cure. The primary role of healthcare in such cases is management, adaptation, and psychological support.
Naturopathic Approach: Counseling and Emotional Support
A critical component of managing visual impairments through naturopathy is psychological and emotional counseling. Key strategies include:
- Positive affirmation: Reassuring patients that their condition does not define their abilities or potential.
- Confidence-building: Encouraging patients to lead normal, productive lives despite their visual limitations.
- Holistic support: Addressing underlying stressors, such as financial, family, or relational problems, which may worsen symptoms.
Even if the blindness cannot be fully corrected, patients benefit greatly from emotional and psychological support, gaining trust in the practitioner and motivation to follow therapeutic guidance.

Therapeutic Interventions
From a naturopathic standpoint, managing visual impairments includes:
- Deep breathing exercises: To reduce stress and improve circulation.
- Mud applications: Therapeutic applications for eye relaxation and detoxification.
- Nutrition and supplementation: A diet rich in vitamins A and C, along with seasonal yellow and orange fruits, supports retinal health.
- Lifestyle adjustments: Maintaining proper sleep patterns, minimizing screen exposure, and incorporating physical activity to support overall eye function.
By integrating these approaches, patients experience improved well-being, reduced anxiety, and enhanced coping mechanisms, even if the underlying visual impairment persists.
Practitioner Guidelines
- Exhibit confidence and positivity: Your attitude directly influences the patient’s trust and responsiveness.
- Provide comprehensive support: Consider both physical and psychosomatic factors affecting the patient.
- Tailor therapy individually: No single approach works for all; customize interventions based on patient history and lifestyle.
- Address secondary issues: Relieving coexisting health conditions improves patient morale and overall health.
Naturopathic Support for Eye Health: Practical Approaches and Supplementation
Eye health is influenced not only by genetics but also by physiological, psychological, emotional, and mental factors. Naturopathy emphasizes a holistic approach, recognizing that improvement depends on the patient’s active participation alongside therapeutic guidance.
Patient Responsibility and Realistic Expectations
Naturopathy is not a standalone cure. The effectiveness of treatment varies depending on:
- Patient compliance: Following dietary and lifestyle recommendations consistently.
- Individual physiology: Each person’s body responds differently to therapies.
- Mental and emotional health: Stress, anxiety, or depression can affect results.
Even with optimal effort from the practitioner, patients may experience partial improvement, which is not a failure but a reflection of complex interactions in the body. The doctor-patient partnership is essential for meaningful results.
Nutritional Support and Supplementation
Correcting nutritional deficiencies is central to eye health:
- Vitamin A: Essential for retinal function, particularly rod cells.
- Vitamin C and E: Antioxidants that protect ocular tissues.
- B-complex vitamins and magnesium: Support nerve function and overall eye health.
In cases where dietary intake is insufficient, supplements can be used temporarily to restore nutrient levels. These are not steroids or medications, but supportive tools to help the body recover. Blood tests, including hemoglobin, are necessary to ensure underlying deficiencies are addressed, as untreated deficiencies can limit the effectiveness of therapy.
Parallel Therapies
For optimal results, naturopathy should be combined with complementary therapies, as relying solely on diet or topical treatments may not suffice. These therapies include:
- Magnetotherapy: Using cow ghee prepared under specific methods, applied to the feet at bedtime. Approximately 5–7 drops are used, massaged with a bronze applicator (cacia) for 5 minutes per foot. This therapy supports acupressure points and circulatory balance.
- Mud applications and deep breathing: Help relax ocular tissues and reduce stress.
Patients should leave the ghee on the feet overnight without washing to allow full absorption and therapeutic effect.
Practical Supplement Recommendations
For eye-related concerns, practitioners often recommend:
- Vitamin A (for night blindness and retinal health)
- Vitamin C and E (antioxidant support)
- B-complex vitamins and magnesium (support for overall ocular and nerve function)
The goal is to restore deficiencies, improve general health, and support natural healing processes.
Naturopathic Approach to Eye Health: Food, Supplements, and Home Remedies
Maintaining healthy vision is a combination of proper nutrition, supplements, and therapeutic care. Naturopathy emphasizes starting with seasonal and natural foods before relying on commercially available supplements.

Seasonal Foods for Eye Health
Yellow and orange fruits and vegetables are particularly beneficial for vision health. Some examples include:
- Fruits: Mangoes, lemons, grapes, and other locally available seasonal fruits.
- Vegetables: Carrots, pumpkins, spinach, broccoli, green peas, and capsicum.
- Nuts and seeds: Peanuts, sesame seeds, almonds, and sunflower seeds provide essential vitamins such as B-complex and vitamin E.
These foods are rich in nutrients like vitamins A, B-complex, C, E, magnesium, and other antioxidants that support retinal function, improve night vision, and reduce oxidative stress in ocular tissues.
Market Supplements
If dietary intake alone is insufficient, targeted supplementation may be necessary:
- Vitamin B-complex: Methinone (B-complex supplement)
- Vitamin A: Oligo or similar vitamin A supplements
- Vitamin C: Citrus fruits or commercial supplements
- Vitamin E: Almonds, sunflower seeds, avocados, spinach, wheatgrass, or commercial capsules
- Magnesium: Groundnuts, cashews, whole grains, green leafy vegetables, or selected supplements
Important: Start with food-based sources whenever possible. Only use commercial supplements if dietary intake is insufficient or absorption is limited. This minimizes the risk of side effects or intolerance.
Eye Care and Hygiene
For individuals with eye discomfort due to infectious conditions, dryness, redness, or irritation, naturopathy emphasizes gentle home care:
- Hydration and sleep: Ensure adequate water intake and sufficient rest.
- Nutrition: Maintain a nutrient-rich diet to support eye health.
- Eye washing: Rinse the eyes 3–5 times daily—morning, evening, and before bed—with clean, running water to remove dust, debris, and minor irritants.
Additionally, eye cups or home-prepared herbal washes can be used:
- Prepare a mild solution of 100 ml water and herbs, soaked for 6–8 hours, then strained through a fine muslin cloth.
- Apply using an eye cup, ensuring gentle and careful contact with the eyes.
This routine supports eye cleansing, reduces inflammation, and promotes overall ocular comfort.
Eye Health Issues: Redness, Nausea, and Double Vision
Naturopathy emphasizes holistic eye care, combining nutrition, hygiene, and therapeutic practices to manage common ocular problems. Below is a summary of guidance for specific concerns such as eye redness, nausea, and diplopia (double vision).
Redness in the Eyes
Redness in the white part of the eyes, often visible as engorged veins, can have multiple causes, including:
- Hypertension or elevated ocular pressure: Regular eye check-ups with a specialist are recommended to measure intraocular pressure. If high, doctors may prescribe eye drops to manage the condition.
- Injury or infection: Trauma or bacterial/viral infections can result in redness and irritation.
- Chemical exposure: Accidental contact with irritants may cause inflammation.
Naturopathic Care:
- Eye washing: Gently rinsing the eyes multiple times a day with clean water to remove irritants.
- Mud application therapy: Applying therapeutic mud over the eyes can reduce redness and provide a cooling effect.
- Time and rest: Giving the eyes sufficient rest and avoiding exposure to irritants supports natural healing.
Nausea and Vomiting Related to Eye Problems
Nausea and vomiting in patients with ophthalmological conditions are often secondary symptoms rather than direct eye problems. Common causes include:

- Chronic migraine: Eye strain or related neurological issues may trigger nausea.
- Digestive imbalance: Patients under stress, depression, or frustration often consume food without mindfulness. Poor digestion and absorption can burden the liver and stomach, resulting in nausea or vomiting.
Naturopathic Approach:
- Encourage patients to eat mindfully, focusing on the quality and timing of meals.
- Support digestive health through nutrition and supplements to reduce systemic stress on the body.
Double Vision (Diplopia)
Diplopia, or double vision, occurs when a person sees two images of a single object. It is relatively common in children but less frequent in adults, especially in the Asian population. Causes may include:
- Genetic factors: Some cases are hereditary.
- Eye muscle or nerve disorders: Affecting the coordination of eye movements.
Naturopathic Care:
- Early intervention with nutritional support, eye exercises, and therapeutic routines may help reduce symptoms.
- While complete resolution through naturopathy alone is uncertain, improvement in clarity and reduction of double vision can be observed over 30–60 days of consistent care.
- Monitoring progress and adjusting therapy based on observed improvements is key.
Key Recommendations
- Eye hygiene: Regular cleansing and therapeutic mud applications for redness.
- Nutrition: Support eye health and overall digestion with mindful eating and nutrient-rich foods.
- Observation and monitoring: Track improvements in double vision and other symptoms over time.
- Medical consultation: Consult an ophthalmologist for intraocular pressure, injury, or persistent redness.
By combining naturopathic care with medical guidance, patients can manage symptoms effectively while supporting overall eye health and systemic well-being.

Magneto Therapy and Eye Care: Naturopathic Approaches
In naturopathy, magneto therapy is an effective and non-invasive method used to support eye health and overall wellbeing. It focuses on stimulating key points, improving circulation, and reducing stress on the ocular system.
Application of Magneto Therapy
Magneto therapy can be applied daily for both general eye care and therapeutic purposes. Key points include:
- Method of Application
- Apply the magnet to specific pressure points, commonly on the feet or near targeted areas, as instructed by the therapist.
- Use gentle, circular rubbing motions for 5 minutes on each foot.
- Avoid washing the area immediately after application to allow absorption and maintain the therapy’s effectiveness.
- Duration and Frequency
- For general eye health, therapy can be done daily.
- Minimum consistent practice is recommended for 60 days, after which it can be paused for six months and repeated if necessary.
- For patients with diabetes or other chronic conditions, similar routines can be followed to support overall systemic health.
- Equipment and Accessibility
- Magneto therapy tools are widely available in health stores and online.
- While online purchases are convenient, purchasing in person is often preferred to ensure quality and ease of use.
- Specialized plates with motorized systems are also available to facilitate massage and activation of multiple pressure points efficiently.
Benefits of Magneto Therapy
- Activates pressure points: Feet and other areas contain over 276 acupressure points connected to different organs. Stimulating these points supports overall health.
- Supports eye care: Regular application can reduce strain, improve circulation, and complement other eye therapies.
- Holistic wellness: Promotes relaxation, reduces stress, and enhances the body’s natural healing processes.
Routine and Integration
- Daily practice ensures maximum benefit, particularly when combined with proper nutrition, sleep, and eye hygiene.
- Magneto therapy is not limited to eye care; it can support systemic health, including circulation, diabetes management, and general wellness.
- Consistency and proper guidance are key to achieving observable results.
Notes for Students and Patients
- Recordings and instructional videos for magneto therapy are provided to students and patients for reference.
- Queries and troubleshooting regarding therapy tools can be directed to support teams, available Monday to Saturday.
- While magneto therapy is highly effective as a complementary approach, it should be combined with proper medical guidance, especially for chronic or severe eye conditions.
Magneto therapy exemplifies naturopathy’s focus on gentle, non-invasive, and holistic interventions to improve eye health and general wellbeing. With regular practice, patients can experience improved circulation, reduced ocular strain, and a supportive complement to other natural therapies.
Naturopathic Eye Care: Magneto Therapy and Herbal Support
Magneto therapy and herbal supplementation are essential components of naturopathic approaches to eye health. These therapies focus on stimulating key points, improving circulation, supporting nutrition absorption, and reducing ocular stress.
Magneto Therapy: Application and Techniques
Magneto therapy involves the use of magnets in combination with specific tools, such as a magnetic GI (gastrointestinal) device, to enhance systemic and ocular health.
- Equipment and Setup
- Red and blue magnets are available commercially.
- The magnetic device (GI) can be purchased ready-made, sometimes infused with herbal extracts for additional therapeutic benefits.
- At home, a simple setup involves placing the GI device between two magnets; it is not necessary to place it directly on the leg or body.
- Procedure
- Place your feet or targeted area near the magnetized GI device.
- Gently rub the area using the device as instructed.
- Regular use improves acupressure stimulation and systemic energy flow.
- Maintenance and Use
- Commercial devices are more durable but costly; simpler home setups are effective for therapeutic purposes.
- Videos and tutorials are available to guide proper application, including ideal positioning and duration.
Herbal and Nutritional Support
Herbs and nutrition play a crucial role in improving eyesight and supporting overall eye health. Proper absorption of nutrients is vital for effectiveness.
- Key Herbs for Eye Health
- Wheatgrass and Alfalfa: Rich in vitamins and minerals that support ocular function.
- Rifa and other external-use herbs: Can be applied therapeutically for specific eye issues.
- Herbs for Systemic Conditions Affecting Eyes
- If the patient has high blood sugar or hypertension, herbs targeting these conditions are prioritized.
- This ensures the root cause is addressed, indirectly supporting better eye health.
- Vitamin Support
- Vitamin A and Vitamin E: Essential for vision health and preventing degeneration.
- Seasonal and natural sources are preferred, but supplements can be used if deficiencies are present.
Integrative Approach
- Naturopathic eye care is holistic, combining magneto therapy, acupressure stimulation, proper nutrition, and herbal therapy.
- The effectiveness depends on consistent practice, proper absorption of nutrients, and addressing underlying systemic conditions.
- Personalized approaches are essential; the choice of herbs, supplements, and therapy intensity should be tailored to individual patient needs.
Naturopathic Recommendations for Eye Health, Stress Management, and General Wellness
In naturopathy, nutrition, herbal therapy, and lifestyle adjustments play a key role in managing eye health, stress, and systemic wellness. Proper guidance ensures patients and students understand how to integrate natural remedies effectively.

Nutritional and Herbal Support
- Alfalfa
- Rich in iron and calcium, alfalfa is particularly beneficial for patients with diabetic neuropathy.
- Regular consumption supports general health, blood sugar regulation, and ocular function.
- Brown Rice
- A preferred alternative to white rice for diabetic patients due to its lower glycemic index and better starch profile.
- While white rice is generally not recommended for anyone, brown rice is more accessible and pocket-friendly, making it a practical dietary option.
- Turmeric
- Known for its anti-inflammatory properties, turmeric supports eye health and systemic wellness, particularly in patients dealing with oxidative stress.
- Stress Management with Herbal Powders
- Asda powder, when combined with Rammi and Shari, acts as an effective stress buster, supporting both mental and physical health.
- Herbal combinations can be tailored depending on individual conditions, like diabetes, hypertension, or ocular stress.
Specific Herbal Insights
- Ash (Fresh vs. Dried)
- Fresh leaves are beneficial for weight reduction and fat metabolism.
- The dried or processed herb provides over 50 health benefits, making it a versatile option for chronic wellness management.
- Other Herbs for Eye Health
- Wheatgrass, alfalfa, and Rifa can be used externally or internally to support vision and ocular nutrition.
- Vitamins A, E, and other key nutrients are enhanced when paired with herbal supplements.
Integrative Approach and Student Guidance
- Nutrition, herbal therapy, and lifestyle changes must be personalized to each patient’s physiological, psychological, and emotional state.
- Students and practitioners are encouraged to ask questions and seek guidance, as understanding the underlying causes is key to effective naturopathic care.
- Continuous learning and practice are vital. Following naturopathy channels on Instagram and YouTube provides additional insights and practical knowledge outside the classroom.
Closing Recommendations
- Personalized support is critical; practitioners are advised to respond to queries via email for individualized guidance.
- Consistency in diet, herbal supplementation, and therapeutic exercises ensures maximum benefit over time.
- Emphasis on positive affirmation, confidence building, and lifestyle management helps patients maintain a holistic approach to wellness.
Conclusion
Eye health is an often-neglected yet profoundly vital aspect of overall well-being. As explored in this lecture, conditions such as glaucoma, night blindness, and color blindness highlight how delicate and precious our sense of vision truly is. The eyes are not merely organs for sight; they are gateways through which we experience the world, connect with others, and maintain independence in daily life. Loss or impairment of vision can deeply affect physical, emotional, and social functioning, making eye care an essential priority rather than an afterthought.
The naturopathic perspective offers a holistic framework for understanding and supporting eye health. While it may not claim to cure every eye disease, its strength lies in identifying and addressing root causes rather than only managing symptoms. By focusing on nutrition, lifestyle management, sleep patterns, and appropriate naturopathic therapies, naturopathy seeks to create internal balance that supports the eyes as part of the whole body system. This approach encourages prevention, slows disease progression, and enhances quality of life through natural and sustainable methods.
Nutrition plays a foundational role in maintaining healthy vision. Deficiencies, poor dietary habits, and toxin accumulation can all negatively impact eye function over time. Similarly, lifestyle choices such as excessive screen exposure, lack of physical activity, and chronic stress place unnecessary strain on the eyes. Adequate and restorative sleep is equally crucial, as it allows the eyes to recover, repair, and function optimally. Naturopathic therapies, when applied judiciously and condition-specifically, can further support circulation, detoxification, and nerve health related to vision.
Equally important is the mindset of awareness and responsibility. As natural therapists and health practitioners, it is our duty to assess eye health as an integral part of overall patient care. Many individuals admit that they rarely think about protecting or nurturing their eyes until a problem arises. This highlights a broader need for education—not only among patients but also within families and communities—about the importance of regular eye care, preventive habits, and early intervention.
The discussion on glaucoma, night blindness, and color blindness also reminds us that some conditions may be progressive or congenital, requiring realistic expectations and compassionate guidance. Naturopathy, in such cases, offers supportive care, lifestyle modification, and preventive strategies that can help individuals live fuller, more empowered lives despite limitations.
In conclusion, eye health deserves conscious attention, respect, and proactive care. By integrating scientific understanding with naturopathic principles, students and practitioners can develop a deeper appreciation for vision and its preservation. Through education, awareness, and holistic practices, we can encourage individuals to value their eyes, protect their sight, and embrace a preventive approach to health—honoring vision as one of nature’s greatest gifts.







