EYE DISORDERS
EYE DISORDERS
Our eyes are remarkable organs that enable us to perceive the world around us. The primary function of the eyes is to capture light from our surroundings and convert it into neural signals that the brain can interpret, allowing us to recognize and understand objects.
The process of seeing begins when light enters the eye. Light reflects off objects and enters the eye through the cornea, the transparent front layer of the eye. It then passes through the aqueous humor, a clear fluid in the anterior chamber, before reaching the lens. The lens focuses the light onto the retina, the light-sensitive layer at the back of the eye.
The retina contains photoreceptor cells called rods and cones, which detect light and color. These cells convert light into electrical signals, which are transmitted to the brain via the optic nerve. The brain then processes these signals, allowing us to perceive and recognize objects.
The eye’s ability to function effectively relies on a complex arrangement of layers and structures. These include:
- Cornea: The transparent front layer that helps to focus light.
- Aqueous Humor: The clear fluid in the anterior chamber that nourishes eye tissues and maintains intraocular pressure.
- Lens: The flexible, transparent structure that focuses light onto the retina.
- Vitreous Humor: The gel-like substance filling the posterior chamber of the eye, helping to maintain the eye’s shape.
- Retina: The light-sensitive layer at the back of the eye containing photoreceptor cells.
- Optic Nerve: The nerve that transmits visual information from the retina to the brain.
Two pockets of transparent fluid, the aqueous humor and the vitreous humor, play crucial roles in maintaining eye health and function. The aqueous humor, found in the anterior chamber, provides nutrients to the eye tissues and helps maintain intraocular pressure. The vitreous humor, which fills the posterior chamber, helps the eye maintain its shape and provides support to the retina.
Understanding the intricate structure and function of the eye helps us appreciate the complexity of vision. In today’s lecture, we will delve deeper into these topics, exploring how each component of the eye contributes to our ability to see and how various eye disorders can impact this vital function.
Understanding the Structure of the Eye:
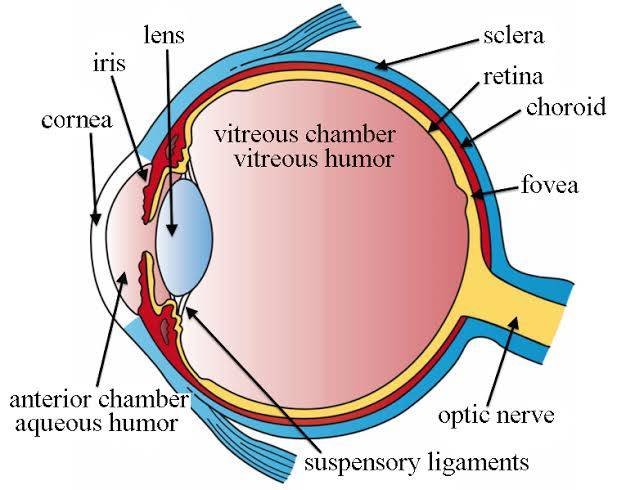
The human eye is a complex organ composed of several layers, each playing a crucial role in the process of vision. These layers work together to protect the eye, nourish its tissues, and transmit visual information to the brain.
The Three Layers of the Eye:
- The Sclera: The Outer Protective Layer The sclera is the white, opaque outer layer of the eye. It serves as a protective coating, providing structural support and shielding the delicate inner components from injury and infection. The sclera also serves as the attachment point for the eye muscles, which control eye movement.
- The Choroid: The Middle Nourishing Layer The choroid is the middle layer of the eye, situated between the sclera and the retina. This layer is rich in blood vessels, which supply essential nutrients and oxygen to the eye tissues. The choroid also contains pigment that helps to reduce light scattering within the eye, ensuring that the light focused onto the retina is sharp and clear.
- The Retina: The Inner Sensory Layer The retina is the innermost layer of the eye and is crucial for vision. It contains photoreceptor cells known as rods and cones, which detect light and color. The retina converts light into electrical signals, which are transmitted to the brain via the optic nerve. The brain then processes these signals to form the images we see.
Understanding the structure of the eye is fundamental to appreciating how vision works. The sclera provides protection and structural support, the choroid nourishes the eye, and the retina captures and transmits visual information. Each layer plays an essential role in maintaining the health and functionality of our eyes, allowing us to perceive the world around us.
Reaching the Retina: Understanding Light-Sensitive Receptor Cells
The retina is a crucial component of the eye, consisting of a thin layer of nerve cells located at the back of the eyeball. It plays a vital role in converting light into electrical signals that the brain can interpret as visual images. Within the retina, there are two types of light-sensitive receptor cells that are essential for vision: rods and cones.
Types of Light-Sensitive Receptor Cells:
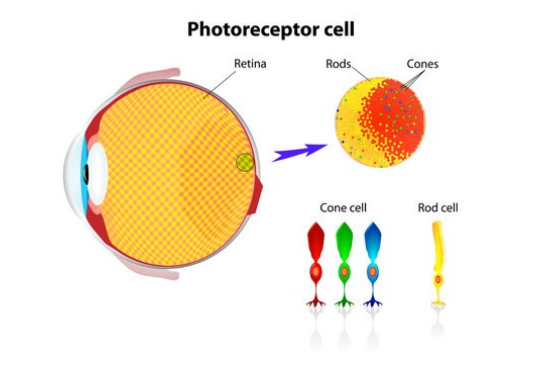
- Rods: Rods are thin, cylindrical receptor cells in the retina that are highly sensitive to light. They are primarily responsible for vision in low-light conditions, allowing us to see in dimly lit environments. Rods do not detect color; instead, they provide black-and-white vision and help with peripheral vision.
- Cones: Cones are cone-shaped, light-sensitive receptor cells in the retina responsible for sharp focus and color perception, particularly in bright light. Cones enable us to see fine details and distinguish a wide range of colors. They are less sensitive to light than rods but are crucial for tasks that require visual acuity and color discrimination.
The Fovea: A Region of High Sensitivity
Cones are concentrated in a specific part of the retina known as the fovea. The fovea is a small, central region of the retina that is densely packed with cones, making it particularly sensitive to detail and color. This concentration allows the fovea to provide the sharpest and most detailed vision, which is essential for activities such as reading, driving, and recognizing faces.
The combination of rods and cones in the retina allows the eye to adapt to different lighting conditions and provides a wide range of visual information. While rods ensure that we can see in low light, cones enable us to perceive fine details and vibrant colors in well-lit environments. This intricate arrangement of receptor cells ensures that the retina can effectively capture and transmit visual information to the brain, facilitating our ability to see and interpret the world around us.
The Structure of the Human Eye: A Detailed Overview
The human eye is an extraordinary organ, intricately designed to capture light and convert it into the images we see. Each part of the eye plays a specific role in this complex process. Let’s explore the key components and their functions.
The Cornea: The Eye’s Light Gateway
At the front of the eye is the cornea, a transparent, dome-shaped layer that covers the iris and pupil. This clear portion of the eye serves as its primary refractive surface, bending light rays that enter the eye. The cornea’s curvature and clarity are essential for focusing incoming light onto the lens and ultimately onto the retina, allowing us to see clearly.
The Iris: The Eye’s Colorful Regulator
Behind the cornea lies the iris, the colored part of the eye. This structure is an extension of the choroid, a layer of the eye rich in blood vessels. The iris is composed of spongy tissue and is responsible for controlling the diameter and size of the pupil.
The pupil, the black circular opening in the center of the iris, acts as the eye’s aperture, regulating the amount of light that enters. In bright conditions, the iris contracts, making the pupil smaller to reduce light entry. In dim conditions, the iris expands, enlarging the pupil to allow more light to pass through, thereby optimizing vision in varying lighting conditions.
The Lens: Focusing Light
Directly behind the pupil is the lens, a transparent, flexible structure that further refines the focus of incoming light rays. The lens adjusts its shape, becoming thicker or thinner, to focus light precisely onto the retina. This process, known as accommodation, enables us to focus on objects at different distances, whether near or far.
The Retina: Light Detection
Once light passes through the lens, it reaches the retina, a thin layer of tissue at the back of the eye. The retina is equipped with millions of photoreceptors—specialized cells that absorb and convert light into electrical signals. There are two main types of photoreceptors:
- Rods, which are highly sensitive to light and enable us to see in low-light conditions.
- Cones, which are responsible for detecting color and work best in bright light.
These photoreceptors play a crucial role in transforming light into the electrical signals needed for visual perception.
The Optic Nerve: Transmitting Signals to the Brain
The optic nerve is a bundle of more than a million nerve fibers that carries electrical signals from the retina to the brain. Once these signals reach the visual cortex, the brain processes and interprets them as the images we see. This transmission of visual information is essential for our perception of the world around us.
Understanding the structure of the human eye highlights the incredible complexity and precision required for vision. Each component, from the cornea to the optic nerve, has a specific function that contributes to our ability to see. The eye’s ability to capture light, focus it, convert it into electrical signals, and transmit those signals to the brain is a marvel of biological engineering. Maintaining eye health is vital, as it ensures that this sophisticated system continues to function effectively, providing us with the sense of sight.
Common Eye Disorders: A Brief Overview
Night Blindness: Night blindness, or nyctalopia, is a condition where individuals have difficulty seeing in low-light or dark environments. While it doesn’t cause complete blindness at night, it significantly impairs vision in dim lighting. Common causes include vitamin A deficiency, cataracts, and retinitis pigmentosa. Treatment focuses on addressing the underlying cause, such as improving diet or undergoing cataract surgery.
Glaucoma: Glaucoma is a group of eye disorders that damage the optic nerve, usually due to increased intraocular pressure (IOP). This damage can lead to gradual vision loss and, if untreated, blindness. The main types are open-angle glaucoma, which develops slowly, and angle-closure glaucoma, which can cause a sudden increase in eye pressure. Management includes medications, laser therapy, or surgery to lower IOP and protect vision.
Diabetic Retinopathy: Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina. High blood sugar levels can damage these vessels, leading to vision problems and, potentially, blindness. The condition progresses from early stages, where vessels weaken and leak, to advanced stages, where abnormal new vessels grow. Managing blood sugar levels, laser treatments, and injections are key to controlling this condition and preventing vision loss.
- Night Blindness: Understanding Nyctalopia
Night blindness, also known as nyctalopia, is a vision problem related to the retina, where individuals have difficulty seeing in low-light conditions or at night. It is not a disease or condition by itself but rather a symptom indicating an underlying issue with the eye’s ability to adjust to reduced lighting.

People experiencing night blindness often find it challenging to see in dimly lit environments or when moving from bright areas to darker ones. This can impact daily activities such as driving at dusk or navigating in low-light settings.
Night blindness can be caused by various factors, and treatment depends on addressing the root cause. Improving dietary habits, undergoing surgical procedures, or managing specific eye conditions can help alleviate the difficulties associated with night blindness and enhance vision in low-light conditions.
If you or someone you know has trouble seeing in the dark, it’s important to consult an eye care professional to identify the cause and determine the best course of action.
Understanding Night Blindness: Causes and Implications
Night blindness, or nyctalopia, is a condition where individuals experience difficulty seeing in low-light or dark environments. This issue is not a standalone disease but a symptom of underlying problems with the eye. Here are some of the primary causes of night blindness:
Vitamin A Deficiency: Vitamin A is crucial for producing rhodopsin, a pigment found in the retina that is necessary for low-light vision. Without sufficient vitamin A, the retina cannot function properly in dim lighting. This deficiency can severely impair night vision, making it difficult to see in the dark or in poorly lit environments.
Retinitis Pigmentosa: Retinitis pigmentosa is a genetic disorder that affects the retina’s light-sensitive cells. This condition causes a gradual deterioration of the rods, which are responsible for vision in low-light conditions. Over time, retinitis pigmentosa can lead to significant night blindness and even loss of peripheral vision.
Cataracts: Cataracts involve the clouding of the eye’s lens, which scatters light and can blur vision. This clouding impacts vision in all light conditions, including low light. People with cataracts often find it particularly challenging to see at night or in dimly lit settings because the reduced clarity makes it harder to process available light.
Certain Medications: Some medications can have side effects that affect night vision. For example, drugs used to treat glaucoma, high blood pressure, or certain psychiatric conditions can sometimes interfere with the eye’s ability to adapt to low-light conditions, leading to night blindness.
Night blindness can significantly impact daily life, particularly in situations requiring good vision in low-light conditions. Understanding the various causes—ranging from vitamin deficiencies and genetic disorders to cataracts and medication side effects—is crucial for identifying and addressing the issue. If you experience difficulty seeing at night, it is essential to consult an eye care professional to determine the underlying cause and explore appropriate treatments.
Night Blindness: Recognizing the Signs and Symptoms
Night blindness, or nyctalopia, is a condition where individuals have trouble seeing in low-light environments. It is often a symptom of an underlying issue with the eye, rather than a standalone condition. Recognizing the signs and symptoms of night blindness can help in seeking appropriate medical attention and management. Here are the key indicators:
Difficulty Seeing in Low Light Conditions
One of the most noticeable signs of night blindness is difficulty seeing in dimly lit environments. People with night blindness struggle to see clearly when the lighting is poor, such as at dusk, dawn, or in artificially lit spaces like restaurants or theaters. This can make navigating in such conditions particularly challenging.
Needing More Light to See Clearly
Individuals with night blindness often find that they require more light to see clearly than they previously did. Tasks that others might perform comfortably in standard lighting, like reading or working on a computer, may require additional light for those with night blindness to see without strain.
Bumping into Objects in Dimly Lit Environments
A common symptom of night blindness is bumping into objects in areas with low lighting. The inability to see obstacles clearly in dim light increases the risk of tripping or colliding with objects. This can be especially dangerous in unfamiliar or cluttered spaces.
Seeing Objects Appear Blurry or Distorted
Another symptom of night blindness is seeing objects as blurry or distorted in low-light settings. Even if there is enough light to discern shapes and outlines, the details may not be clear, and objects may appear fuzzy or out of focus.
Night blindness can significantly affect daily activities, especially those conducted in low-light conditions. If you or someone you know experiences any of these signs and symptoms, it is essential to consult with an eye care professional. Early recognition and diagnosis can lead to effective management and treatment, improving vision and quality of life in dimly lit environments.
Night Blindness: Treatment Options
Night blindness, or nyctalopia, can make it difficult to see in low-light conditions. Treating this condition involves addressing its root causes and managing symptoms through various approaches. Here are the key treatment options:
Conventional Medicine
Vitamin A Supplements
For night blindness caused by vitamin A deficiency, the primary treatment is vitamin A supplements. Vitamin A is essential for the production of rhodopsin, a pigment in the retina crucial for seeing in low light. Replenishing this vitamin can significantly improve night vision.
Addressing Underlying Conditions
If night blindness is due to conditions such as cataracts, treatment focuses on addressing these underlying issues. Cataracts, which cause clouding of the lens, can impair vision in all lighting conditions. Surgical removal of the cataract and replacement with an artificial lens often restores clarity and improves night vision.
Naturopathic Approaches
Dietary Changes
Increasing the intake of foods rich in vitamin A can help manage night blindness. Foods such as carrots, sweet potatoes, spinach, and kale are high in beta-carotene, which the body converts to vitamin A. Incorporating these foods into your diet can enhance your ability to see in low-light conditions.
Lutein and Zeaxanthin Supplements
Lutein and zeaxanthin are antioxidants found in the retina that play a role in protecting the eyes and improving vision. Some studies suggest that supplements containing these compounds may help improve night vision and overall eye health. They are naturally present in green leafy vegetables and other colorful fruits and vegetables.
Treating night blindness involves both conventional and naturopathic approaches. Whether through vitamin A supplementation, addressing underlying conditions like cataracts, or making dietary changes, there are effective ways to manage and improve night vision. If you experience symptoms of night blindness, consult an eye care professional to explore the most suitable treatment options for your condition.
Dietary Sources of Lutein and Zeaxanthin
Lutein and zeaxanthin are important antioxidants known as carotenoids that are beneficial for eye health, particularly in protecting against conditions like age-related macular degeneration (AMD) and improving night vision. Here are some common dietary sources of lutein and zeaxanthin:

- Yellow and Orange Fruits: Such as oranges, peaches, papaya, and watermelon.
- Vegetables: Including carrots, spinach, broccoli, peas, capsicum (bell peppers), and basil.
- Corn: Yellow corn is particularly rich in lutein and zeaxanthin.
- Egg Yolk: Contains lutein and zeaxanthin, which are beneficial for eye health.
- Pistachios: A nut that contains significant amounts of these antioxidants.
- Green Leafy Vegetables: Such as spinach, kale, and collard greens, which are excellent sources of lutein and zeaxanthin.
Incorporating these foods into your diet regularly can help support eye health and potentially improve night vision by providing essential nutrients like lutein and zeaxanthin.
2. Understanding Glaucoma: A Complex Eye Condition
Glaucoma encompasses a group of eye diseases that progressively damage the optic nerve, often leading to irreversible vision loss. It is one of the leading causes of blindness among adults worldwide. Here’s an overview of this complex eye condition:

Definition:
Glaucoma is a term used to describe a group of eye diseases characterized by damage to the optic nerve. This damage is typically associated with elevated intraocular pressure (IOP), but it can also occur with normal or even low IOP in some cases.
Leading Cause of Blindness:
Glaucoma is a significant public health concern and is recognized as one of the leading causes of blindness globally. The gradual loss of vision that occurs with glaucoma often goes unnoticed in its early stages, making regular eye exams crucial for early detection and treatment.
Risk Factors:
One of the primary risk factors for glaucoma is increased pressure within the eye, known as intraocular pressure (IOP). However, not everyone with elevated IOP develops glaucoma, and some individuals may develop the condition with normal IOP levels. Other risk factors include age, family history, ethnicity (African descent being at higher risk), and certain medical conditions.
Glaucoma is a complex eye condition that requires ongoing management and treatment to preserve vision. Early detection through regular eye exams is critical, as treatment can help slow or halt the progression of the disease. If you have risk factors for glaucoma or experience any symptoms such as blurred vision or headaches, consult an eye care professional promptly for evaluation and appropriate management.
Signs and Symptoms of Glaucoma:
Glaucoma is a group of eye diseases that can lead to irreversible vision loss if left untreated. Recognizing the signs and symptoms is crucial for early detection and management. Here are the key indicators:
Gradual Vision Loss
One of the most common signs of glaucoma is gradual vision loss, often starting with peripheral vision (side vision). Over time, the loss of peripheral vision can progress to affect central vision as well.
Tunnel Vision:
In advanced stages of glaucoma, individuals may experience tunnel vision—a narrowing of the field of vision where only central vision remains. This narrowing occurs as peripheral vision continues to diminish.
Acute Angle-Closure Glaucoma:
Acute angle-closure glaucoma presents with sudden and severe symptoms, including:
- Sudden Onset of Severe Eye Pain: Often described as a deep ache within the eye.
- Redness: The affected eye may appear red due to increased pressure.
- Blurred Vision: Vision may become suddenly blurred or hazy.
- Seeing Halos Around Lights: A halo effect around lights, especially in dim conditions.
These symptoms indicate a medical emergency requiring immediate attention to prevent permanent vision loss.
Recognizing the signs and symptoms of glaucoma is crucial for early diagnosis and treatment. Regular eye exams, especially as you age or if you have risk factors such as family history or certain medical conditions, are essential for detecting glaucoma in its early stages. If you experience any of these symptoms, particularly sudden onset of severe eye pain or vision changes, seek prompt evaluation by an eye care professional to preserve your vision and eye health.
Understanding Glaucoma: Causes and Risk Factors
Glaucoma is a complex group of eye diseases that can lead to irreversible vision loss. Understanding its causes and risk factors is crucial for prevention and early detection. Here’s an overview:
Causes:
- Increased Intraocular Pressure (IOP): One of the primary causes of glaucoma is elevated pressure within the eye due to fluid buildup. This increased pressure can gradually damage the optic nerve, leading to vision loss.
- Damage to the Optic Nerve: The optic nerve can be damaged by various factors, including prolonged elevated IOP and other conditions that affect optic nerve health.
Risk Factors:
Several factors increase the risk of developing glaucoma:
- Age: The risk of glaucoma increases with age, particularly after 60 years old.
- Family History: Having a close relative with glaucoma increases your risk, suggesting a genetic predisposition.
- Certain Medical Conditions: Conditions such as diabetes and high blood pressure can increase the risk of glaucoma.
- Race: African Americans have a higher risk of developing glaucoma compared to other ethnic groups.
Glaucoma can develop slowly over time, often without noticeable symptoms in its early stages. Regular eye exams are crucial, especially if you have any of these risk factors. Early detection and treatment can help preserve vision and manage glaucoma effectively. If you have a family history of glaucoma or any concerns about your eye health, consult an eye care professional for personalized evaluation and management.
Lifestyle Factors that Modify Intraocular Pressure (IOP)
The intraocular pressure (IOP) within the eye can be influenced by various lifestyle factors. Understanding these influences is important for managing eye health, particularly in individuals at risk for conditions like glaucoma. Here are some lifestyle factors known to modify IOP:
Playing High Wind Instruments:
Playing high wind instruments such as the trumpet or flute can temporarily increase intraocular pressure. This is due to the increased air pressure exerted during blowing, which can affect the pressure within the eye.
Dietary Sources of Caffeine:
Consuming caffeine, such as a cup of coffee, can transiently elevate intraocular pressure. This effect is generally temporary and varies among individuals.
Yoga Positions:
Certain yoga positions, such as headstand postures, where the heart is positioned above the eye, can alter intraocular pressure. The change in blood flow and pressure dynamics may affect IOP temporarily.
Tight Neckties:
Wearing tight neckties can potentially increase intraocular pressure by affecting blood flow and circulation around the neck and head area.
Weight Lifting:
Engaging in weight lifting or other strenuous activities that involve intense physical exertion can briefly elevate intraocular pressure. This increase is typically temporary and resolves after cessation of the activity.
Cigarette Smoking:
Smoking cigarettes has been associated with higher intraocular pressure. The exact mechanisms are not fully understood, but smoking cessation may help reduce this risk factor.
Awareness of these lifestyle factors can contribute to better management of intraocular pressure and overall eye health. If you have concerns about your eye pressure or are at risk for conditions like glaucoma, discuss these factors with an eye care professional. They can provide guidance on minimizing potential risks and maintaining optimal eye health through lifestyle modifications and regular eye exams.
Glaucoma Treatment Options
Managing glaucoma typically involves a combination of approaches aimed at reducing intraocular pressure (IOP) and preserving vision. Here are the main treatment options:
Conventional Medicine:
Eye Drops:
The primary treatment for glaucoma involves prescription eye drops that help lower intraocular pressure. These eye drops work by either reducing the production of aqueous humor (the fluid in the eye) or increasing its outflow to maintain a healthy pressure level within the eye.
Laser Surgery:
Laser surgery, such as laser trabeculoplasty, is a procedure that can improve the drainage of fluid from the eye, thereby reducing intraocular pressure. It is often used when eye drops are not sufficient in controlling IOP.
Surgical Procedures:
In cases where eye drops and laser surgery are not effective, surgical procedures may be necessary. These surgeries aim to create new drainage channels in the eye to allow fluid to flow out more efficiently and reduce intraocular pressure.
Treatment for glaucoma aims to lower intraocular pressure to prevent or slow down the progression of optic nerve damage and vision loss. The specific treatment plan depends on the type and severity of glaucoma, as well as individual factors such as overall health and response to treatment. Regular monitoring by an eye care professional is essential to assess the effectiveness of treatment and adjust the approach as needed to preserve vision and maintain eye health.
Vitamin B3 Sources: Foods Rich in Niacin:

Vitamin B3, also known as niacin, is an essential nutrient that plays a key role in energy production and metabolism. It is found in various foods, particularly in:
- Peanuts (Moongphali)
- Sesame Seeds (Til)
- Bajra (Pearl Millet)
- Jowar (Sorghum)
- Mushrooms (Khumb)
- Peas and Beans
- Lentils
- Chickpeas
- Corn
Incorporating these foods into your diet can help ensure an adequate intake of vitamin B3, supporting overall health and well-being.
Vitamin B12 Sources:
Vitamin B12, also known as cobalamin, is an essential nutrient involved in nerve function, red blood cell production, and DNA synthesis. It is primarily found in animal-based foods and some fortified products. Here are common sources of vitamin B12:
- Dairy Products: Such as milk, cheese, and yogurt.
- Fortified Foods: Including breakfast cereals, nutritional yeast, and plant-based milk alternatives fortified with vitamin B12.
- Meat and Seafood: Beef, poultry, fish (such as salmon and trout), shellfish (like clams and mussels), and other animal-derived products.
- Fermented Foods: Some fermented foods, such as tempeh and certain types of fermented soy products, may contain small amounts of vitamin B12 due to bacterial fermentation.
These sources provide essential vitamin B12 for vegetarians and non-vegetarians alike, ensuring adequate intake for overall health and well-being.
Vitamin B6 Sources:
Vitamin B6, also known as pyridoxine, is important for brain development and function, as well as for maintaining overall health. It is found in a variety of foods, including:
- Bananas (Kela)
- Green Peas (Matar)
- Pistachios (Pista)
These foods are excellent natural sources of vitamin B6 and can be easily incorporated into a balanced diet to support optimal health and well-being.
Vitamin B1 Sources:
Vitamin B1, also known as thiamine, is essential for energy metabolism and nerve function. It is found in a variety of foods, including:
- Legumes: Whole moong dal, chana dal, masoor dal, rajma (kidney beans), soybeans
- Nuts and Seeds: Sunflower seeds, peanuts (groundnuts), almonds, walnuts, pistachios
- Fruits and Vegetables: Oranges, tomatoes, peas, spinach, methi leaves (fenugreek leaves)
- Eggs and Fish
- Dairy Products: Milk and yogurt
Incorporating these foods into your diet can help ensure an adequate intake of vitamin B1, supporting energy production and overall health.
Vitamin C Sources:
Vitamin C, also known as ascorbic acid, is an essential nutrient with powerful antioxidant properties that supports immune function, wound healing, and collagen production. It is found abundantly in various fruits, vegetables, and sprouted pulses. Here are some sources of vitamin C:
- Amla (Indian Gooseberry)
- Guava
- Oranges
- Lemon
- Drumsticks (Moringa)
- Bell Peppers
- Broccoli
- Sprouted Pulses (Green Gram)
Incorporating these vitamin C-rich foods into your diet can help maintain optimal health and support immune function. Including a variety of these foods ensures a sufficient intake of vitamin C to meet daily requirements.
Vitamin E Sources:
Vitamin E is a fat-soluble antioxidant that plays a crucial role in protecting cells from oxidative stress and maintaining skin health. It is found in a variety of foods, particularly in:
- Sunflower Seeds
- Almonds
- Peanuts
- Avocado
- Spinach
- Wheat Germ Oil
- Mustard Greens
- Mango
Incorporating these foods into your diet provides essential vitamin E, contributing to overall health and well-being. Including a mix of these sources ensures a balanced intake of this important nutrient.
Magnesium Sources:
Magnesium is an essential mineral involved in over 300 biochemical reactions in the body, including energy production, muscle function, and nerve transmission. It is found in a variety of foods, particularly:
- Nuts: Such as groundnuts (peanuts), cashew nuts, walnuts, and almonds.
- Whole Grains: Including wheat, bajra (pearl millet), and jowar (sorghum).
- Shellfish: Such as crab and oyster.
- Dark Green Leafy Vegetables: Such as spinach and other leafy greens.
- Legumes: Including peas and lotus stem.
Incorporating these magnesium-rich foods into your diet can help maintain adequate magnesium levels and support overall health. Including a variety of these sources ensures a balanced intake of this important mineral.
Vitamin A Sources:
Vitamin A is a fat-soluble vitamin essential for vision, immune function, and skin health. It is found in a variety of foods, particularly:
- Orange and Yellow Fruits and Vegetables: Such as carrots, mangoes, papaya, pumpkins, sweet potatoes, and apricots.
- Green Leafy Vegetables: Including spinach, kale, and mustard leaves.
- Dairy Products: Milk, cheese, and yogurt are all good sources of vitamin A.
- Fish: Oily fish, such as salmon, tuna, and mackerel, are rich in vitamin A.
- Eggs: Eggs are a good source of vitamin A and many other nutrients.
Incorporating these vitamin A-rich foods into your diet can help maintain optimal levels of this important vitamin, supporting overall health and well-being. Including a variety of these sources ensures a balanced intake of vitamin A and its precursors.
3. Diabetic Retinopathy: Understanding a Complex Condition
Diabetic retinopathy is a serious complication of diabetes mellitus that affects the retina, the light-sensitive tissue at the back of the eye essential for vision. This condition develops due to prolonged high blood sugar levels, which damage the tiny blood vessels within the retina.
Introduction:
Diabetic retinopathy is characterized by various pathological changes triggered by hyperglycemia. These changes include oxidative stress, inflammation, abnormal growth of blood vessels (angiogenesis), accumulation of advanced glycation end products, and overactivation of protein kinase C (PKC). These factors collectively contribute to the deterioration of retinal blood vessels and the surrounding tissues, leading to vision impairment and, if untreated, potentially blindness.

Pathophysiology:
- Oxidative Stress: Elevated glucose levels lead to an increase in reactive oxygen species (ROS), causing oxidative damage to retinal cells.
- Inflammation: Chronic hyperglycemia triggers inflammatory responses in the retina, further exacerbating tissue damage.
- Angiogenesis: Abnormal blood vessel growth (angiogenesis) in the retina can lead to leakage of fluids and blood, impairing vision.
- Advanced Glycation End Products (AGEs): These compounds accumulate in the retina due to prolonged exposure to high glucose levels, contributing to tissue damage and dysfunction.
- Protein Kinase C (PKC) Activation: Overactivation of PKC in response to hyperglycemia disrupts cellular signaling pathways, leading to vascular and neuronal cell death.
Diabetic retinopathy underscores the importance of managing blood sugar levels in diabetic patients to prevent or delay the onset and progression of this sight-threatening condition. Regular eye examinations, early detection, and timely intervention are crucial for preserving vision and maintaining eye health in individuals with diabetes. Managing diabetes through lifestyle modifications, medication adherence, and ongoing medical care plays a pivotal role in reducing the risk and severity of diabetic retinopathy.
Signs and Symptoms of Diabetic Retinopathy:
Diabetic retinopathy is a serious complication of diabetes mellitus that affects the eyes, specifically the retina. Recognizing the signs and symptoms is crucial for early detection and treatment. Here are the common indicators:
Blurred Vision:
One of the earliest signs of diabetic retinopathy is blurred vision. Fluctuating blood sugar levels can cause temporary changes in vision clarity.
Floaters:
Floaters are small dark spots or shapes that appear to float across your field of vision. They are caused by small flecks of protein or blood cells floating in the vitreous, the gel-like substance that fills the inside of your eye.
Difficulty Seeing Colors:
Diabetic retinopathy can affect color perception, leading to difficulty seeing colors as vividly or accurately as before.
Wavy or Distorted Vision:
Vision may appear wavy or distorted, which can indicate swelling or fluid leakage in the retina.
Sudden Vision Loss (in Advanced Stages):
In advanced stages of diabetic retinopathy, sudden and significant vision loss may occur, often due to the detachment of the retina or severe hemorrhage.
If you have diabetes, it is important to monitor your eye health regularly and undergo comprehensive eye exams as recommended by your healthcare provider. Early detection and timely intervention are critical in managing diabetic retinopathy and preserving vision. If you experience any of these symptoms or notice changes in your vision, seek prompt evaluation by an eye care professional to prevent progression and minimize vision loss.
Causes of Diabetic Retinopathy:
Diabetic retinopathy is a serious complication of diabetes mellitus that affects the eyes, specifically the retina. The condition develops due to various pathological changes induced by prolonged high blood sugar levels. Here are the primary causes:
High Blood Sugar Levels:
High blood sugar levels (hyperglycemia) over time can damage the delicate blood vessels in the retina, which are crucial for vision. This damage occurs due to the accumulation of metabolic by-products and oxidative stress.
Leakage of Fluid and Blood:
As a result of the damaged blood vessels, there is leakage of fluid and blood into the retina. This leakage can lead to swelling (edema) and distortions in vision.
Growth of Abnormal New Blood Vessels:
In response to the lack of oxygen and nutrients caused by damaged blood vessels, the retina may initiate neovascularization—the growth of abnormal new blood vessels. These new vessels are fragile and prone to leakage, further exacerbating vision problems and potentially causing more severe complications such as retinal detachment.
Diabetic retinopathy underscores the importance of managing blood sugar levels effectively to prevent or delay the onset and progression of this sight-threatening condition. Strict glycemic control, regular eye examinations, and timely intervention are crucial in reducing the risk and severity of diabetic retinopathy. If you have diabetes, work closely with your healthcare provider to monitor and manage your condition to protect your vision and overall eye health.
Treatment Options for Diabetic Retinopathy:
Diabetic retinopathy, a complication of diabetes affecting the eyes, requires careful management to preserve vision and prevent progression. Treatment options aim to address the underlying causes and complications associated with the condition. Here are the main approaches:
Controlling Blood Sugar Levels:
Effective blood sugar control is fundamental in managing diabetic retinopathy. Tight glycemic management helps reduce the progression and severity of retinal damage.
Laser Therapy:
Laser therapy is commonly used to treat diabetic retinopathy by targeting specific areas of the retina:
- Sealing Leaking Blood Vessels: Laser photocoagulation is used to seal leaking blood vessels, reducing fluid leakage and preventing further damage.
- Destroying Abnormal Blood Vessels: Laser treatment can also destroy abnormal new blood vessels (neovascularization) that can cause bleeding and impair vision.
Anti-VEGF Injections:
Anti-VEGF (vascular endothelial growth factor) injections are medications injected into the eye to inhibit the growth of abnormal blood vessels. This treatment helps reduce leakage and swelling in the retina.
Surgery (Vitrectomy):

In advanced cases of diabetic retinopathy, vitrectomy may be necessary:
- Removing Scar Tissue: During vitrectomy, surgeons remove scar tissue that can distort vision.
- Removing Blood from Vitreous Humor: This procedure involves removing blood that has leaked into the vitreous humor (the gel-like substance in the eye), which can improve vision clarity.
Treatment for diabetic retinopathy is tailored to the specific stage and severity of the condition. Regular eye examinations and early intervention are crucial in managing diabetic retinopathy effectively. If you have diabetes, work closely with your healthcare team to monitor your eye health and manage your condition to reduce the risk of vision loss associated with diabetic retinopathy.
Naturopathic Approaches for Diabetic Retinopathy:
In addition to conventional medical treatments, naturopathic approaches can complement the management of diabetic retinopathy. These approaches focus on lifestyle modifications and natural supplements that may support eye health and reduce the progression of the condition. Here are some naturopathic recommendations:
Dietary Changes:
Dietary modifications can play a crucial role in managing diabetic retinopathy:
- Increase Fruits and Vegetables: Consuming a diet rich in fruits and vegetables provides essential vitamins, minerals, and antioxidants that support eye health.
- Omega-3 Fatty Acids: Including sources of omega-3 fatty acids, such as fish (salmon, mackerel) and flaxseeds, may have anti-inflammatory benefits for the eyes.
- Limit Processed Foods and Sugary Drinks: Avoiding processed foods and beverages high in added sugars helps maintain stable blood sugar levels, which is crucial for preventing further damage to the retina.
Supplements:
Certain supplements may be recommended by naturopaths to support eye health in diabetic retinopathy:
- Bilberry: Known for its antioxidant properties, bilberry may help improve blood circulation in the retina.
- Lutein and Zeaxanthin: These antioxidants are found in high concentrations in the retina and may help protect against oxidative damage.
- Alpha-Lipoic Acid: Known for its antioxidant effects, alpha-lipoic acid may help reduce oxidative stress in the retina.
Naturopathic approaches for diabetic retinopathy emphasize holistic strategies that can be used alongside conventional medical treatments. It’s important to consult with a qualified naturopathic doctor or healthcare provider before starting any new supplements or making significant dietary changes. Integrating these approaches with regular medical care and monitoring can help optimize eye health outcomes for individuals with diabetic retinopathy.
Sources of Omega-3 Fatty Acids: A Comprehensive Guide:
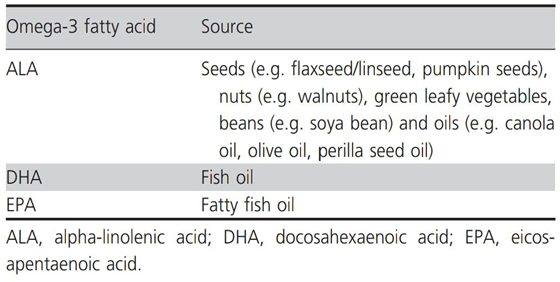
Omega-3 fatty acids are essential nutrients known for their numerous health benefits, particularly for heart health and brain function. They are classified into three main types: ALA (alpha-linolenic acid), DHA (docosahexaenoic acid), and EPA (eicosapentaenoic acid). Each type plays a unique role in supporting overall health, and their sources vary widely across different food groups.
ALA (Alpha-Linolenic Acid):
ALA is a plant-based omega-3 fatty acid that our bodies cannot produce and must be obtained through diet. It serves as a precursor to EPA and DHA, although the conversion efficiency in the body is limited. Rich sources of ALA include:
- Seeds: Such as flaxseed (or linseed) and pumpkin seeds.
- Nuts: Particularly walnuts, which are also rich in other nutrients.
- Green Leafy Vegetables: Like spinach and kale, which provide a variety of vitamins and minerals.
- Beans: Such as soybeans (soya bean), a versatile source of protein and omega-3s.
- Oils: Including canola oil, olive oil, and perilla seed oil, which are used in cooking and salad dressings.
Consuming a diet containing high levels (50–60%) of ALA involves incorporating these sources regularly into meals, ensuring a steady intake of this essential nutrient.
DHA (Docosahexaenoic Acid) and EPA (Eicosapentaenoic Acid):
DHA and EPA are primarily found in marine sources and are particularly beneficial for brain health, cardiovascular health, and reducing inflammation. The main sources include:
- Fish Oil: A concentrated source of DHA and EPA extracted from fatty fish such as salmon, mackerel, and trout.
- Fatty Fish: Direct consumption of fatty fish like salmon, sardines, and tuna provides significant amounts of DHA and EPA.
These marine sources are highly bioavailable, meaning the body can readily absorb and utilize DHA and EPA from fish and fish oil supplements.
Incorporating Omega-3 Fatty Acids into Your Diet:
Including a variety of these omega-3 rich foods in your diet is essential for maintaining overall health and well-being. Here are some practical tips:
- Include Fatty Fish: Aim to eat fatty fish at least twice a week to ensure an adequate intake of DHA and EPA.
- Use ALA Sources: Incorporate ALA-rich foods like flaxseeds, walnuts, and leafy greens into salads, smoothies, or as toppings for yogurt.
- Choose Healthy Oils: Opt for oils such as canola oil and olive oil in cooking and meal preparation to boost ALA intake.
Omega-3 fatty acids play a vital role in supporting various bodily functions, from heart health to brain function and inflammation reduction. By diversifying your diet to include sources of ALA, DHA, and EPA, you can optimize your omega-3 intake and promote long-term health benefits. Whether through plant-based sources or marine options, incorporating omega-3 fatty acids into your daily meals is a proactive step towards enhancing your overall health oil.

Metabolism and Effects of Omega Fatty Acids:
Introduction:
Omega fatty acids are essential fats that the human body cannot produce on its own. They play a crucial role in various bodily functions, including inflammation regulation and cell membrane formation. This article explores the metabolism and effects of two primary types of omega fatty acids: Omega-3 and Omega-6.
Omega-3 Fatty Acids:
Sources:
- Seeds, nuts, green leafy vegetables, beans, and oils
- Fish oil
- Fatty fish oil
Types:
- Alpha-Linolenic Acid (ALA)
- Eicosapentaenoic Acid (EPA)
- Docosahexaenoic Acid (DHA)
Metabolism:
- ALA: Found in plant sources such as seeds, nuts, green leafy vegetables, beans, and oils. ALA is metabolized in the body to produce EPA and DHA.
- EPA and DHA: These are primarily obtained from fish oil and fatty fish oil. DHA is also produced through the metabolism of ALA. Both EPA and DHA are crucial for anti-inflammatory and anti-angiogenic (preventing the formation of new blood vessels) functions.
Health Benefits:
- Anti-inflammatory properties: Omega-3 fatty acids help reduce inflammation in the body, which can lower the risk of chronic diseases such as heart disease and arthritis.
- Anti-angiogenic effects: Preventing the formation of new blood vessels can be beneficial in conditions such as cancer, where reducing blood supply to tumors is advantageous.
Omega-6 Fatty Acids:
Sources:
- Vegetable oils
- Nuts
- Seeds
- Animal products
Types:
- Linoleic Acid
- Arachidonic Acid
Metabolism:
- Linoleic Acid: Found in vegetable oils, nuts, seeds, and animal products. Linoleic acid is metabolized in the body to produce arachidonic acid.
- Arachidonic Acid: This is a precursor to various pro-inflammatory compounds such as prostaglandins and leukotrienes.
Health Effects:
- Pro-inflammatory properties: Omega-6 fatty acids can promote inflammation when consumed in excess. This is due to their conversion to arachidonic acid, which subsequently produces pro-inflammatory prostaglandins and leukotrienes. While some inflammation is necessary for immune function, excessive inflammation can lead to chronic inflammatory diseases.
Balancing Omega-3 and Omega-6 Fatty Acids:
For optimal health, it is crucial to maintain a balance between omega-3 and omega-6 fatty acids. The typical Western diet often contains a higher ratio of omega-6 to omega-3, which can contribute to increased inflammation and associated health issues. Increasing the intake of omega-3-rich foods while moderating omega-6 consumption can help achieve a healthier balance.
Omega fatty acids, specifically omega-3 and omega-6, are vital for various bodily functions. Omega-3 fatty acids, found in fish oils and certain plant sources, offer anti-inflammatory benefits. In contrast, omega-6 fatty acids, present in vegetable oils and animal products, can promote inflammation if consumed in excess. Understanding their metabolism and effects can guide dietary choices to maintain a healthy balance and support overall well-being.
Omega-6 Rich Foods to Limit for a Healthier Diet:

Omega-6 fatty acids are essential fats that the body needs for normal growth and development. However, an imbalance between omega-6 and omega-3 fatty acids can contribute to inflammation and other health issues. Here are some sources of omega-6 that should be limited in your diet:
Vegetable Oils:
- Safflower Oil
- Sunflower Oil
- Corn Oil
- Grape Seed Oil
These oils are commonly used in cooking and food processing and are high in omega-6 fatty acids. Consuming them in excess can skew the omega-3 to omega-6 ratio unfavorably.
Processed Foods:
- Fried Snacks
- Baked Goods (made with above oils)
Many processed foods, such as fried snacks and baked goods, are made with vegetable oils high in omega-6. These products often contain trans fats and other unhealthy additives that can contribute to inflammation and health problems.
Fatty Cuts of Meat:
- Red Meat
- Processed Meats
While meat is a good source of protein, fatty cuts of red meat and processed meats (like sausages and bacon) can contain high levels of omega-6 fatty acids. Moderation is key to maintaining a balanced diet.
Some Nuts and Seeds:
- Peanuts
- Sunflower Seeds
While nuts and seeds are generally healthy sources of fats and protein, certain varieties like peanuts and sunflower seeds are higher in omega-6 fatty acids. Enjoy them in moderation as part of a balanced diet.
Importance of Balance:
While omega-6 fatty acids are essential for health, it’s crucial to maintain a balanced ratio with omega-3 fatty acids. Aim to include more sources of omega-3s, such as fatty fish (salmon, mackerel), flaxseeds, and walnuts, in your diet to counterbalance the omega-6 intake.
By being mindful of the sources of omega-6 fatty acids in your diet and making conscious choices to limit them, you can support overall health and reduce the risk of inflammation-related conditions. Opting for healthier cooking oils, minimizing processed foods, and choosing leaner cuts of meat can help achieve a better balance of omega-6 and omega-3 fatty acids for optimal well-being.
Tips for a Diabetic Retinopathy Diet:
Managing diabetic retinopathy involves making dietary choices that support eye health and overall well-being. Here are some practical tips to consider:
Focus on Omega-3 Rich Foods:
Omega-3 fatty acids are beneficial for reducing inflammation and supporting cardiovascular health, which is crucial for managing diabetic retinopathy. Include these sources in your diet:
- Fatty Fish: Such as salmon, tuna, and mackerel, which are rich in DHA and EPA.
- Flaxseeds and Chia Seeds: Plant-based sources of ALA, a precursor to DHA and EPA.
- Walnuts: A nutritious nut that provides omega-3s along with other essential nutrients.
Choose Healthy Fats:
Opt for healthy fats that support heart health and overall well-being:
- Olive Oil: Use extra virgin olive oil in cooking and salad dressings for its anti-inflammatory properties.
- Avocado: Rich in monounsaturated fats and fiber, avocados are a versatile addition to meals.
Limit Processed Foods and Saturated Fats:
Processed foods and foods high in saturated fats can contribute to inflammation and may worsen diabetic retinopathy. Limit or avoid:
- Processed Foods: Such as fried snacks, baked goods made with unhealthy oils.
- Saturated Fats: Found in fatty cuts of meat, full-fat dairy products, and some processed foods.
Maintain a Healthy Weight and Manage Blood Sugar Levels:
Achieving and maintaining a healthy weight through balanced nutrition and regular physical activity is essential for managing diabetes and its complications like diabetic retinopathy.
- Monitor Blood Sugar Levels: Regularly check and manage blood glucose levels as advised by your healthcare provider to prevent fluctuations that can impact eye health.
A diabetic retinopathy diet focuses on nutrient-dense foods that support eye health, manage blood sugar levels, and reduce inflammation. By incorporating omega-3 rich foods, healthy fats, and avoiding processed foods and excessive saturated fats, you can optimize your diet to support overall health and well-being while managing diabetic retinopathy effectively. Always consult with your healthcare provider or a registered dietician for personalized dietary recommendations tailored to your specific health needs.
Conclusion: Managing Eye Disorders Effectively:
Managing eye disorders, whether common conditions like night blindness or more complex issues such as diabetic retinopathy, requires proactive care and attention. Here are key takeaways to ensure optimal eye health:
Early Detection and Management:
Early detection through regular eye exams is critical for identifying and addressing eye disorders before they progress. Routine screenings can catch issues early when treatments are most effective.
Importance of Regular Eye Exams:
Regular eye exams are not just for vision correction; they are vital for detecting eye disorders early, especially for individuals at higher risk due to age, family history, or chronic conditions like diabetes.
Role of a Healthy Lifestyle:
A healthy lifestyle can significantly impact eye health:
- Nutritious Diet: Including foods rich in essential nutrients like vitamins A, C, and E, omega-3 fatty acids, and antioxidants.
- Regular Exercise: Promoting overall health, circulation, and potentially reducing the risk of eye diseases.
- Avoiding Risk Factors: Such as smoking and excessive alcohol consumption, this can contribute to eye problems.
Personalized Advice from Healthcare Professionals:
Consulting with your doctor or ophthalmologist is crucial for personalized advice and treatment plans tailored to your specific needs and risk factors. They can provide guidance on managing chronic conditions, adjusting lifestyle habits, and selecting appropriate treatments.
By prioritizing early detection, regular eye exams, adopting a healthy lifestyle, and seeking professional advice, you can take proactive steps to prevent, manage, or slow the progression of various eye disorders. Your vision and overall eye health are worth investing in through consistent care and informed decisions.
Remember, your eyesight is precious—take care of it today for a brighter tomorrow.