Gout, Arthritis, Spondylitis Part 2
Understanding Gout, Arthritis, and Spondylitis
In our previous discussion, we explored the complexities of arthritis, laying the groundwork for a deeper understanding of related conditions like gout and spondylitis. In this article, we will briefly recap the key points from Part One and transition into our discussion on gout, arthritis, and spondylitis.
Recap of Part One: Arthritis Overview:

During Part One, we dissected arthritis into two main sections, focusing on the different types and characteristics of this condition. This segmentation allowed us to grasp the various forms of arthritis and how they impact individuals differently. By reviewing these points, we can seamlessly connect the insights gained from Part One to our upcoming exploration of gout and spondylitis.
What We Covered About Arthritis:
- Definition and Types: We established a clear definition of arthritis and outlined its various types. Understanding these distinctions is crucial for recognizing symptoms and formulating effective treatment plans.
- Symptoms: We highlighted the common symptoms associated with arthritis, such as joint pain, stiffness, and swelling. Recognizing these symptoms early can lead to timely intervention and better management of the condition.
- Causes and Risk Factors: Our discussion included the underlying causes of arthritis and the risk factors that may increase susceptibility to the disease. Factors such as age, genetics, and lifestyle choices were addressed to provide a holistic view of arthritis.
- Management and Treatment Options: Finally, we touched on the various management and treatment strategies available for arthritis, including medication, lifestyle modifications, and alternative therapies. Understanding these options empowers individuals to take an active role in their health.
Exploring Gout and Spondylitis:
Today, we will focus on two specific conditions related to arthritis: gout and spondylitis. October is recognized as Arthritis Awareness Month, highlighting the fact that approximately 18 million people worldwide are affected by arthritis, underscoring its significance as a chronic health issue.
What Is Arthritis?
Arthritis is a condition characterized by inflammation or degeneration that affects the joints. This inflammation can lead to considerable pain and discomfort, making it challenging for individuals to move freely or maintain an active lifestyle. It is crucial to understand the different types of arthritis to effectively manage and treat the condition.
Types of Arthritis:
In our previous discussion, we categorized arthritis into three main types:
- Osteoarthritis: This is the most common form of arthritis, often referred to as primary arthritis. It typically occurs due to wear and tear on the joints over time, leading to the breakdown of cartilage.
- Inflammatory Arthritis: This category includes conditions like rheumatoid arthritis and ankylosing spondylitis. Inflammatory arthritis is characterized by joint inflammation caused by an autoimmune response, where the body’s immune system mistakenly attacks its tissues.
- Septic Arthritis: Also known as juvenile arthritis or childhood arthritis, this less common form of arthritis is caused by infection in the joint, leading to inflammation.
Focus on Gout and Spondylitis:
Today, we will specifically delve into gout and spondylitis, both of which present unique symptoms and challenges.
- Gout is a form of inflammatory arthritis characterized by sudden and severe attacks of pain, swelling, and redness, often affecting the big toe. It occurs due to an accumulation of uric acid crystals in the joints, leading to intense inflammation.
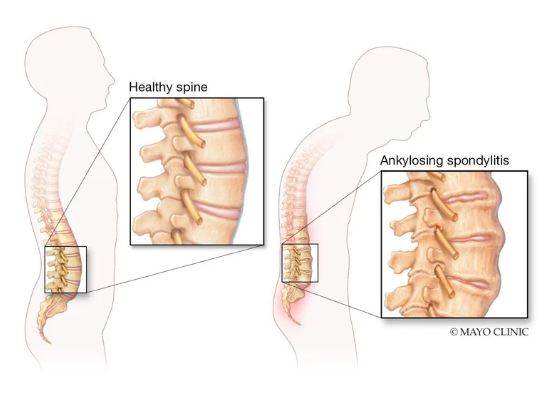
- Spondylitis, particularly ankylosing spondylitis, is a type of inflammatory arthritis that primarily affects the spine, causing pain and stiffness. Over time, it can lead to fusion of the vertebrae, resulting in a reduced range of motion and postural changes.
Understanding Osteoarthritis
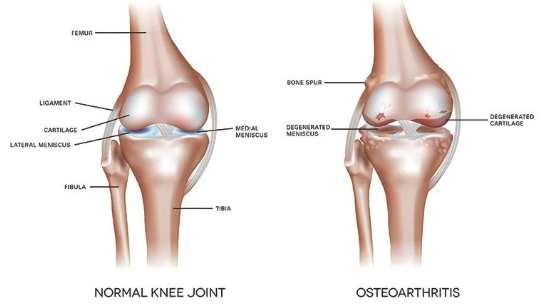
Osteoarthritis is a degenerative joint disease characterized by the deterioration of cartilage, the protective tissue that cushions the ends of bones in the joints. As the cartilage breaks down, it leads to painful interactions between the bones, resulting in discomfort and limited mobility.
What Happens in Osteoarthritis?
In osteoarthritis, the cartilage that normally provides a smooth surface for joint movement begins to erode. This deterioration can create a reduction in the space between the bones, leading to increased friction during movement. The result is pain and stiffness, making it difficult for individuals to remain active and engage in daily activities.
Symptoms of Osteoarthritis:
The symptoms of osteoarthritis often develop gradually and can vary in severity. Common symptoms include:
- Joint Pain: Pain during movement or after periods of inactivity.
- Swelling: Inflammation around the joint area.
- Reduced Flexibility: A decrease in the ability to move the joint through its full range of motion.
- Stiffness: Often felt after resting or in the morning, which can ease with movement.
- Crepitus: A grating sensation or sound when moving the affected joint.
Osteoarthritis can affect any joint in the body, but it most commonly impacts the knees, hips, hands, and spine. Unlike rheumatoid arthritis, which often affects joints symmetrically, osteoarthritis typically impacts one side of the body more than the other.
Causes of Osteoarthritis:
While the exact cause of osteoarthritis is not fully understood, several factors may contribute to its development:
- Age: The risk of developing osteoarthritis increases significantly with age, particularly for those over 60.
- Genetics: A family history of osteoarthritis can increase susceptibility.
- Weight: Excess weight places additional stress on weight-bearing joints, such as the knees and hips.
- Occupational Factors: Jobs that require repetitive stress on joints or prolonged standing can elevate the risk.
- Injuries: Previous joint injuries, such as fractures or ligament tears, can increase the likelihood of developing osteoarthritis later in life.
- Gender: Studies indicate that men may be at a higher risk compared to women, particularly before menopause.
Overall, osteoarthritis is a complex condition influenced by various factors. Understanding these aspects can help individuals identify potential risks and seek appropriate management strategies.
Understanding Rheumatoid Arthritis:
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints, leading to inflammation, pain, and, in severe cases, joint deformity. Unlike osteoarthritis, which is primarily a degenerative joint disease, RA involves the immune system mistakenly attacking healthy joint tissues.
What Happens in Rheumatoid Arthritis
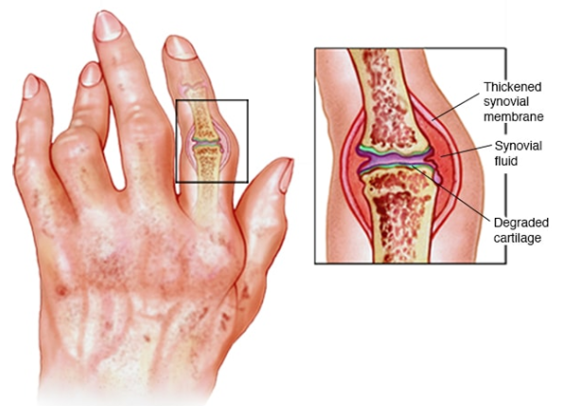
In rheumatoid arthritis, the body’s immune system attacks the synovium, the lining of the membranes that surround the joints. This inflammation can spread to other areas of the body, including internal organs, leading to more systemic effects. Over time, the inflammation can result in joint erosion and deformities if not managed effectively.
Symptoms of Rheumatoid Arthritis:
Common symptoms of rheumatoid arthritis include:
- Joint Pain: Often symmetrical, affecting both sides of the body.
- Swelling: Inflammation can cause visible swelling around the joints.
- Stiffness: Particularly pronounced in the morning or after prolonged periods of inactivity.
- Fatigue: A general feeling of tiredness and lack of energy.
- Fever: Mild fever may accompany the disease.
- Weakness: General weakness due to the body’s inflammatory response.
As the disease progresses, it may affect other systems, leading to complications in organs such as the heart, lungs, and kidneys.
Causes of Rheumatoid Arthritis:
The exact cause of rheumatoid arthritis remains unclear, but several contributing factors have been identified:
- Genetic Factors: A family history of RA may increase the risk, indicating a hereditary component.
- Hormonal Influences: Hormonal changes, especially in women, may play a role, as the disease often develops around menopause.
- Environmental Factors: Exposure to certain environmental triggers, such as smoking or pollutants, may increase susceptibility.
- Infections: Some infections may initiate the autoimmune response in predisposed individuals.
RA typically develops between the ages of 30 and 60, with specific terms used to categorize its onset:
- Young Onset Rheumatoid Arthritis: Occurs between the ages of 16 and 40.
- Late Onset Rheumatoid Arthritis: Develops after age 60.
Risk Factors for Rheumatoid Arthritis
Several risk factors can increase the likelihood of developing rheumatoid arthritis:
- Age: The risk increases with age, particularly for those over 40.
- Gender: Women are more likely to develop RA than men, especially post-menopause due to hormonal imbalances.
- Obesity: Excess weight can increase the strain on joints and contribute to the disease’s onset.
- Metabolic Disorders: Conditions like diabetes may also increase the risk.
- Medications: Long-term use of certain medications may increase susceptibility to autoimmune responses.
Effective management of rheumatoid arthritis often involves a combination of lifestyle changes, alternative therapies, and, when necessary, medications to reduce inflammation and manage symptoms.
Septic Arthritis (Juvenile Arthritis):
Septic arthritis, or juvenile arthritis, is a rare condition worldwide, particularly in our region. While we have encountered very few cases, ongoing research is essential.
This disorder affects the immune system and tissues around deep joints, primarily in children aged 16 years or younger. Bacterial infections, particularly from Staphylococcus aureus (staph), are the most common causes of juvenile arthritis.
Diagnosis of Arthritis
The diagnostic process begins with a thorough assessment of symptoms. Doctors typically do not immediately order blood tests or imaging; instead, they conduct a physical examination, checking for tenderness and swelling near the joints and the presence of excessive fluid.
Once the physician suspects arthritis, they may order specific tests. X-rays are often the first step, useful primarily for rheumatoid arthritis, while MRIs can help identify calcium deposits in the joints. No specific blood tests exist for osteoarthritis, but general blood tests can reveal underlying conditions or infections.
Common initial tests include a Complete Blood Count (CBC) and Erythrocyte Sedimentation Rate (ESR). The ESR usually ranges from 0 to 20; in arthritis cases, it may exceed 50 or 60. Additional tests like the Rheumatoid Factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) can provide further insights.
Treatment Approaches
From a medical perspective, osteoarthritis is generally not reversible, but mild to moderate symptoms can be managed. Supportive devices, physiotherapy, and pain relief injections or steroids may be employed.
Naturopathy Perspective
In naturopathy, various therapies can aid recovery:
- Diet and Nutrition: Adequate nutrition is crucial, including vitamin D3 for bone health.
- Mud Applications: Effective in reducing inflammation and promoting blood flow to swollen areas.
- Yoga and Pranayama: Integral components of a healthy lifestyle.
- Herbal Remedies: Various herbs can alleviate symptoms, including:
- Saffron: Available in juice form or as tablets.
- Turmeric (Haldi): Commonly used in cooking.
- Tulsi (Holy Basil), Giloy, Alfalfa, Guggul, Ashwagandha, Triphala, Wheatgrass, and Aloe Vera: These herbs can help manage pain and symptoms.
Incorporating these strategies can lead to effective management of septic arthritis symptoms and may contribute to overall health improvements.
Key Points on Gout

- Definition: Gout is a condition characterized by the deposition of uric acid crystals in the joints, leading to inflammation and pain, particularly when bending or moving the affected joints.
- Symptoms:
- Patients may experience cracking sounds in their joints, which can be indicative of high uric acid levels.
- Gout can affect multiple joints simultaneously, including fingers, wrists, knees, and ankles.
- Types of Gout:
- Primary Gout: Caused by the body’s overproduction of uric acid.
- Secondary Gout: Resulting from external factors such as medications or excessive supplementation that leads to increased uric acid levels.
- Factors Contributing to Gout:
- The use of certain medications and supplements over extended periods can contribute to elevated uric acid levels.
- Individuals may not seek regular medical advice, believing that the absence of symptoms means they do not need to stop or adjust their supplements.
Understanding Gout and Its Diagnosis
In the field of medicine, particularly during outpatient consultations, accurately diagnosing gout can sometimes pose challenges. This often stems from the need for a comprehensive understanding of a patient’s medical history and the root causes of their condition. Gout, a type of inflammatory arthritis, is primarily associated with elevated uric acid levels in the blood, leading to the deposition of uric acid crystals in and around joints.
Importance of Patient History
When faced with a patient exhibiting symptoms of gout, healthcare professionals must prioritize gathering a detailed patient history. This involves asking specific questions about the patient’s health over the past several years, including:
- Previous Health Issues: Understanding any other health conditions the patient has faced is essential. For instance, comorbidities like diabetes or kidney disease can impact uric acid levels and the overall management of gout.
- Medication and Supplement History: Patients often do not realize that supplements, although not classified as medications, can significantly affect their health. It’s crucial to inquire about any over-the-counter or prescription supplements the patient may have been taking. Many patients continue these supplements without consulting their healthcare provider, which can lead to unrecognized complications.
- Lifestyle Factors: Questions should also delve into dietary habits, alcohol consumption, and any history of injuries or accidents that might have affected joint health.
Observing Patient Behavior
During consultations, healthcare professionals may encounter patients who have been managing their health independently. These patients may avoid seeking medical advice for extended periods—often two to three years—while continuously consuming various supplements. This lack of professional oversight can lead to hyperuricemia (elevated levels of uric acid in the blood), which is a significant contributor to the development of gout.
For instance, when patients take supplements excessively, particularly those containing vitamin B12, calcium, or iron, without medical guidance, they can inadvertently increase uric acid levels. This is particularly concerning in cases where patients self-diagnose and self-treat, leading them to believe that they are managing their health adequately.
Detoxification as a Treatment Approach
When hyperuricemia is diagnosed, healthcare professionals often recommend detoxification as a necessary step. Detoxification can help reduce the overall burden of uric acid in the body, potentially alleviating symptoms associated with gout. This process involves dietary adjustments, hydration, and sometimes the use of specific medications aimed at lowering uric acid levels.
Proactive Consultation Techniques
To facilitate a more effective diagnostic process, healthcare providers should actively engage with patients. This means not only asking about current medications but also encouraging patients to reflect on their complete health history. Specific techniques include:
- Reviewing Medical Records: Analyzing the patient’s past medical records and test reports can provide insights into their health trajectory. For example, if previous lab tests indicated deficiencies, it would be prudent to ask the patient about any supplements they have taken since then.
- Clarifying Treatment Decisions: Practitioners should communicate clearly about the implications of continuing or discontinuing certain medications or supplements. Many patients may not recognize the potential consequences of prolonged supplement use without medical supervision.
Ensuring Thorough Communication
Some patients might withhold information about supplements, viewing them as benign or non-critical to their health discussions. Therefore, it is essential for healthcare providers to encourage open dialogue by repeatedly asking about any supplements or medications the patient has used, regardless of their perception of these substances.
By creating an environment where patients feel comfortable sharing their full health history, practitioners can gather the necessary information to identify the root cause of gout effectively.
The Diagnostic Responsibility
In conclusion, accurately diagnosing gout requires a thorough understanding of a patient’s medical history, including past health issues, medications, and lifestyle choices. A detailed consultation not only helps in identifying the underlying causes of the disease but also facilitates the development of an effective treatment plan tailored to the patient’s unique health needs. Without this critical information, it becomes challenging to provide proper care and management for patients suffering from gout.
Root Causes and Risk Factors of Gout
Gout is a complex condition characterized by sudden and severe pain, redness, and swelling in the joints, often affecting the big toe. The root causes and risk factors of gout are multifaceted and can be influenced by a combination of genetic, dietary, and lifestyle factors. Understanding these elements is crucial for prevention and management.
Root Causes of Gout
- Age and Gender:
- Increasing Age: The prevalence of gout rises with age. As individuals grow older, the likelihood of developing symptoms increases. This is often attributed to changes in kidney function and uric acid metabolism over time.
- Gender: Gout is more common in men than women, particularly before menopause. This gender disparity is thought to be due to hormonal differences affecting uric acid levels.
- Dietary Factors:
- Purine-Rich Foods: High consumption of purine-rich foods such as red meat, organ meats, and certain seafood can lead to elevated uric acid levels in the body. Foods like shellfish and sardines, often prevalent in coastal diets, are particularly high in purines and can contribute to the risk of gout.
- Excessive Alcohol Consumption: Alcohol, especially beer and spirits, can increase uric acid production and decrease its elimination, leading to higher levels in the bloodstream.
- Metabolic Disorders:
- Renal Function: The kidneys play a critical role in filtering and excreting uric acid. Conditions that impair kidney function can lead to an accumulation of uric acid, thus increasing the risk of gout. Individuals with renal failure often exhibit higher uric acid levels due to the kidneys’ inability to eliminate it effectively.
- Detoxification Impairment:
- Kidney Health: The kidneys are essential for detoxifying the body and regulating uric acid levels. If the renal system is compromised, toxins and uric acid can accumulate, leading to gout. Chronic kidney disease can be a significant underlying factor contributing to elevated uric acid levels.
- Infections:
- Certain infections can trigger gout attacks, especially if they affect the joints. The body’s response to infections may lead to increased inflammation, which can precipitate a gout flare-up.
Risk Factors for Gout
- Family History:
- A family history of gout can increase an individual’s risk. Genetic predispositions affect how the body metabolizes purines and excretes uric acid.
- Lifestyle Choices:
- Obesity: Excess weight can lead to increased production of uric acid and decreased excretion by the kidneys. Individuals with higher body mass indexes (BMIs) are at greater risk for developing gout.
- Physical Activity: A sedentary lifestyle can contribute to obesity and metabolic disturbances that may increase gout risk. Regular exercise is crucial for maintaining a healthy weight and metabolic balance.
- Medical Conditions:
- Certain medical conditions, such as hypertension, diabetes, and metabolic syndrome, can contribute to an increased risk of gout. The relationship between these conditions often involves insulin resistance and altered uric acid metabolism.
- Medication:
- Some medications can increase uric acid levels. Diuretics, commonly used to treat high blood pressure, are known to cause elevated uric acid concentrations.
- Dehydration:
- Inadequate hydration can lead to higher concentrations of uric acid in the blood, as the kidneys require sufficient fluid to effectively filter and excrete waste products.
- Dietary Habits:
- Diets high in refined carbohydrates and low in fruits and vegetables may increase the risk of gout. A balanced diet rich in alkaline foods can help mitigate this risk.
Most of the cases observed indicate that individuals with a family history—like grandparents, parents, or siblings—are more prone to face problems related to gout. In addition to genetics, lifestyle, dietary habits, and environmental factors significantly contribute to the issue, particularly through the deposition of monosodium urate crystals in the joints, a condition known as hyperuricemia.
What is Hyperuricemia?

Hyperuricemia refers to the deposition of uric acid crystals, specifically monosodium urate, in the body. A blood test can reveal elevated uric acid levels, often exceeding 90%. The majority of patients are male and older than 30, while women are more affected post-menopause.
There’s a common belief that females are more affected by gout, but research shows that men are actually more prone to this condition. Women benefit from certain hormones, particularly during their menstrual cycles, which may help mitigate risks associated with gout. Hormones like estrogen and progesterone, secreted from the ovaries, are particularly effective in preventing conditions such as osteoarthritis, rheumatoid arthritis, and gout.
In females, gout typically arises after menopause or during the transitional period. However, with proper care—maintaining nutritional balance and focusing on mental and physical health—the chances of elevated uric acid levels can be minimized.
Signs and Symptoms of Gout:
Certain symptoms indicate the presence of gout, including:
- Tophi: Deposits of uric acid in the joints, especially in the fingers, ankles, and toes.
- Affected Areas: Uric acid crystals commonly accumulate in the finger joints, ankle joints, and toes, and can also affect the knee joint.
- Severe Pain: Sudden onset of intense pain in the affected joint, which often starts at night.
- Swelling and Redness: The affected area may appear swollen and red, accompanied by warmth.
- Stiffness: Affected joints may become stiff and tender, making movement difficult.
- Kidney-Related Symptoms: As kidneys play a crucial role in filtering out uric acid, issues with kidney function may also manifest as gout symptoms.
Knee replacements are often discussed due to damaged cartilage and synovial fluid in the joints, primarily caused by the excessive deposition of uric acid. The friction from uric acid crystals leads to pain and restricted movement.
In cases of gout, typical symptoms include:
- Redness
- Swelling
- Pain
- Warmth (the affected area may feel warmer compared to non-affected areas)
Unlike general arthritis and osteoarthritis, warmth is a hallmark symptom of gout. The affected area may appear swollen, fluid-filled, and sometimes develop a thin layer of skin over it. Other symptoms can include fever and weight loss.
Renal Calculus:
Elevated uric acid levels can also lead to renal calculus, commonly known as kidney stones. Many individuals experience kidney stones every few months, which is a sign of increasing uric acid levels in the body.
Gout is a type of inflammatory arthritis characterized by sudden, severe attacks of pain, swelling, and redness in the joints. The condition is primarily associated with high levels of uric acid in the blood, leading to the formation of crystals in the joints. This article explores the signs and symptoms of gout, its relation to kidney function, diagnostic evaluations, and the importance of a comprehensive physical examination and patient history.
The Role of Kidneys in Gout
The kidneys are vital organs responsible for filtering blood and eliminating waste products, including uric acid. Each kidney contains millions of nephrons, which continuously work to eliminate toxins from the body. When the uric acid levels in the blood exceed normal ranges, it can lead to the crystallization of uric acid in the joints, causing gout.
The normal range for uric acid in the blood is typically between 2 to 7 milligrams per deciliter (mg/dL). When these levels rise, it can lead to painful gout attacks. Therefore, measuring uric acid levels is a critical first step for those experiencing symptoms associated with gout.
Diagnostic Evaluation of Gout
Diagnosing gout involves several evaluations:
- Physical Examination: A thorough physical examination can reveal important clues about the presence of gout. Approximately 50 to 60% of the diagnosis can be made through physical assessments.
- Gait Analysis: Observing the patient’s gait can indicate how they move and whether they are experiencing discomfort. Patients with gout may walk with difficulty due to pain in their joints.
- Joint Examination: The doctor should check for swelling or tenderness in the affected joints. Bending the knee and assessing for pain or abnormal sounds (indicative of fluid buildup or uric acid crystal deposits) is essential.
- History Taking: Understanding the patient’s medical history is crucial in diagnosing gout. It is important to ask about:
- Family History: Gout can have genetic components, so knowing whether family members have experienced similar issues can aid in diagnosis.
- Medication History: Patients should disclose any medications they are currently taking or have taken in the past, including modern and alternative therapies.
- Lifestyle Factors: Information on dietary habits, hydration levels, and physical activity can provide insights into the patient’s overall health and potential triggers for gout.
- Laboratory Tests: Blood tests are essential to measure uric acid levels. Elevated uric acid in the blood can confirm a diagnosis of gout.
The Importance of Patient-Doctor Relationship
For effective treatment, building trust and confidence between the patient and healthcare provider is crucial, especially in cases involving chronic conditions like gout. Open communication ensures that the patient feels comfortable discussing symptoms, concerns, and history, which ultimately leads to more effective management of the condition.
Gout is a complex condition influenced by various factors, including diet, kidney function, and genetic predisposition. Understanding the signs and symptoms, conducting thorough physical examinations, and obtaining detailed patient histories are essential steps in diagnosing and managing gout effectively. If you suspect you may have gout, it is important to consult a healthcare professional for a comprehensive evaluation and tailored treatment plan.
Gout Diagnosis and Management: Naturopathic Approach
Gout, a form of arthritis caused by elevated uric acid levels, can lead to severe joint pain, swelling, and inflammation. Proper diagnosis and management of gout require a thorough understanding of its symptoms and comprehensive testing. In this article, we’ll explore the different tests used to diagnose gout, management strategies, and the role of lifestyle changes in managing the condition.
Diagnostic Tests for Gout
To accurately diagnose gout, healthcare professionals use a combination of physical assessments and laboratory tests. The following are key diagnostic tools:
- X-Ray: Although an X-ray may not detect uric acid crystals, it helps reveal bone and joint abnormalities that could be indicative of gout or other types of arthritis.
- Ultrasound (USG): This imaging technique can detect uric acid crystal deposits within the joints. It’s an essential tool for studying the microscopic aspects of synovial fluid and is often recommended in gout diagnoses.
- Serum Uric Acid Test: This blood test measures the concentration of uric acid in the blood. Elevated levels indicate a higher likelihood of gout, though the test alone isn’t always definitive since some people with high uric acid never develop gout.
- Complete Blood Count (CBC): This test provides information on the general health of the patient and helps rule out other causes of joint pain. A CBC evaluates the levels of different blood cells, which may indicate underlying health issues.
- ESR (Erythrocyte Sedimentation Rate): This test measures the rate at which red blood cells settle at the bottom of a test tube. A high ESR can indicate inflammation in the body, which may be associated with gout.
- Kidney Function Tests (Serum Creatinine, Urea, BUN): As kidneys play a crucial role in filtering out uric acid, kidney function tests help determine whether the kidneys are effectively eliminating excess uric acid. These tests include measuring serum creatinine, urea, and blood urea nitrogen (BUN).
- Fasting Blood Sugar and Lipid Profile: Conditions like high blood sugar and elevated triglycerides can contribute to gout and other health issues. These tests provide a complete view of the patient’s metabolic health.
Management of Gout: Pharmacological and Non-Pharmacological Approaches

Managing gout involves both medication and lifestyle changes. Treatment is often divided into two categories:
1. Pharmacological Treatments
- Anti-Inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and alleviate pain during acute gout attacks.
- Urate-Lowering Therapies: Medications like allopurinol or febuxostat are often prescribed to lower uric acid levels and prevent future gout attacks.
2. Non-Pharmacological Treatments
- Physiotherapy and Exercise: Regular joint movement is essential to reduce stiffness. Physical activity improves blood circulation, which helps remove deposited uric acid crystals through the body’s detoxification systems.
- Dietary Changes: Reducing the intake of purine-rich foods (such as red meat, organ meats, and certain seafood) is crucial in managing uric acid levels. Increased hydration helps flush out excess uric acid.
- Lifestyle Modifications: Regular sleep, proper posture, and managing stress can significantly impact the frequency and severity of gout flare-ups. Adjusting sleep schedules to ensure restful sleep between 9 PM to 7 AM is particularly beneficial for tissue repair and reducing inflammation.
- Comfort Devices: For those experiencing chronic gout or joint pain, devices such as ergonomic chairs and footrests can reduce strain on joints during prolonged sitting or standing.
- Weight Management: Obesity increases the stress on joints and can exacerbate gout symptoms. A balanced weight-loss plan, focusing on gradual reduction, is key to relieving pressure on the joints.
The Role of Rest and Proper Posture in Gout Management
For individuals with desk jobs or those who stand for long periods, improper posture can exacerbate gout symptoms. The downward pull of gravity on the legs during prolonged sitting can affect circulation, leading to the pooling of blood in the lower extremities, which may worsen joint inflammation.
It is essential to:
- Take short breaks every 30-40 minutes to stand, stretch, or walk around.
- Avoid sitting in the same position for too long, as this can lead to the deposition of uric acid crystals in specific joints.
- Prioritize rest and ensure a sleep routine that supports recovery and reduces inflammation.
Weight Loss and Its Impact on Gout
Maintaining a healthy weight is vital for individuals with gout. Excess body weight puts additional pressure on joints, particularly those already affected by uric acid crystals. Weight loss can relieve joint strain and improve overall joint health.
Gout is a manageable condition with the right combination of medical treatment and lifestyle changes. Early diagnosis through various tests, alongside personalized pharmacological and non-pharmacological approaches, can significantly reduce symptoms and prevent future flare-ups. Managing weight, adjusting diet, and incorporating physical activity into daily life are key to long-term relief from gout.
Pharmacological Treatments for Gout
- Acute Attacks: During sudden and severe gout attacks, stronger medications or injections may be necessary.
- Medications:
- NSAIDs: These may be prescribed during acute attacks, with examples like 25-50 mg doses.
- Chronic Management: Allopurinol (100 mg) is a common medication for chronic gout management.
- Caution in Prescription: The speaker emphasizes not to prescribe medications without proper knowledge due to potential side effects and the importance of understanding why certain medications are used.
Naturopathic Recommendations
- Lifestyle Modifications:
- Mud Application: Suggested as a topical remedy.
- Deep Breathing and Yoga: These practices can increase oxygen levels and antioxidant activity, benefiting cardiovascular health and circulation.
- Anema (Enema):
- Purpose: Helps eliminate constipation and cleanse the intestines, removing accumulated morbid matter.
- Efficacy: Once the system is clean, other treatments can be more effective.
- Sun Bathing:
- Benefits: Provides strength to bones and muscles near joints, enhances oxygen levels, and contributes to overall well-being.
- Yoga Practices: Recommended to be performed in conjunction with sunbathing for enhanced health benefits.
Gout, a form of arthritis characterized by sudden and severe pain, often results from elevated levels of uric acid in the body. While medications can help manage symptoms, dietary choices play a crucial role in controlling uric acid levels. This article outlines specific foods to avoid and highlights healthier alternatives to foster well-being.
Foods to Avoid
1. High-Protein Foods
When it comes to managing uric acid levels, moderation is key. High-protein foods, particularly from sources like sprouts and heavy seeds, can contribute to elevated uric acid. It’s advisable to limit protein intake, opting for plant-based options that are easier on the body.
2. Fermented Foods
Fermented foods, while popular in many cuisines, can exacerbate gout symptoms. Items like bakery products and heavily fermented items should be avoided. Excessive fermentation can lead to increased acidity in the body, making it essential to be mindful of these foods.
3. Certain Vegetables
Certain vegetables, despite their health benefits, may trigger discomfort in some individuals. Cauliflower, broccoli, and tomatoes have been noted to potentially worsen joint pain and should be consumed with caution.
4. Salt and Sugar
The use of white salt and sugar can be detrimental to those managing uric acid levels. Instead, consider switching to healthier alternatives such as pink salt or rock salt. Additionally, processed foods and soft drinks should be eliminated from the diet, as they can contribute to increased acidity.
5. Nuts
Nuts are often considered healthy snacks, but certain types should be limited. Specifically, excessive consumption of cashew nuts should be avoided. Instead, opt for walnuts in moderation, incorporating them as a part of a balanced diet.
Foods to Embrace
1. Fasting
One of the most effective methods to manage uric acid levels is through fasting. Depending on individual capacity, a fasting period of 3 to 4 days can help cleanse the system. This practice allows the body to rest and reset its digestion, providing relief from symptoms.
2. Raw Fruits and Vegetables
Incorporating raw, alkaline-rich fruits and vegetables into your diet is crucial. These foods not only provide essential nutrients but also help to counteract acidity. Salads made from seasonal and regional produce are excellent additions, fostering a balanced intake of vitamins and minerals.
3. Juice Therapy
Consider introducing a variety of fresh juices into your daily routine. Consuming at least five different juices throughout the day can increase fluid intake and aid in detoxifying the body. Juice therapy offers a refreshing and effective way to promote hydration and balance acidity levels.
4. Soaked Seeds
Soaked seeds can be beneficial in managing uric acid levels. Consider incorporating soaked sal seeds and legumes into your routine. The water used for soaking is particularly beneficial when consumed on an empty stomach, acting as a natural detoxifier.
5. Regular Monitoring
For optimal results, maintain these dietary changes consistently for 60 to 80 days. This commitment allows the body to adapt and can lead to significant improvements in overall well-being.
Managing uric acid levels, particularly in the context of gout, requires a balanced approach that combines dietary awareness with mindful choices. By avoiding certain foods and embracing healthier alternatives, individuals can take control of their health and alleviate the discomfort associated with elevated uric acid. Remember to consult a healthcare professional for personalized advice and recommendations tailored to your specific needs.
Understanding Ankylosing Spondylosis: A Guide to a Chronic Inflammatory Disease
Introduction
Ankylosing spondylosis (AS) is a chronic inflammatory disease that primarily affects the vertebral joints, leading to stiffness and pain in the spine. Over time, it can cause significant changes in posture and mobility, making understanding and management crucial for those affected.
What is Ankylosing Spondylosis?
Ankylosing spondylosis is a type of spondylitis characterized by inflammation of the vertebrae, resulting in a rigid and often stooped posture. The term “ankylosing” refers to the fusion of bones, while “spondylosis” indicates the involvement of the vertebrae. Together, they describe a condition where inflammation leads to the hardening or stiffness of the spinal joints, often resulting in a hunchbacked appearance over time.
The Nature of the Disease
Ankylosing spondylosis is classified as a seronegative spondyloarthritis, meaning that rheumatoid factor tests typically yield negative results. This type of arthritis is distinct because it does not show the common markers found in other inflammatory arthritis forms, complicating diagnosis and understanding.
Key Features of Ankylosing Spondylosis
- Impact on the Spine: AS specifically affects the spinal column and can lead to significant changes in posture. The condition is associated with a reduction in flexibility, causing the spine to become increasingly rigid over time.
- Symptoms: Common symptoms include chronic pain and stiffness in the lower back and hips, especially after periods of inactivity. As the disease progresses, individuals may find it challenging to maintain an upright posture, leading to a pronounced stoop.
- Age of Onset: While AS can occur at any age, it typically begins in early adulthood. It is essential for young individuals experiencing chronic back pain to seek medical evaluation to rule out AS.
The Importance of the Vertebral Column
The human vertebral column consists of 33 vertebrae, a critical structure that supports our ability to stand, walk, and maintain proper posture. Each vertebra plays a vital role in enabling mobility and preventing excessive bending or slouching.
Observations on Aging
As people age, particularly those in their 70s and 80s, it’s common to observe significant postural changes. Many elderly individuals may rely on supports, such as canes or walkers, due to the stiffness and deformity resulting from conditions like ankylosing spondylosis. These changes highlight the importance of maintaining spinal health throughout life.
Preventive Measures and Strengthening the Spine
Maintaining the strength and flexibility of the vertebral column is crucial to preventing the onset or progression of ankylosing spondylosis. Individuals can take proactive measures, including:
- Exercise: Regular physical activity can help improve flexibility and strength. Low-impact exercises such as swimming or yoga are particularly beneficial.
- Posture Awareness: Practicing good posture can help alleviate strain on the spine and prevent discomfort.
- Healthy Lifestyle Choices: A balanced diet and avoiding smoking can contribute to overall health and may help manage inflammation.
Ankylosing spondylosis is a serious condition that requires awareness and management to mitigate its effects on the spine and overall quality of life. By understanding the disease, its impact on posture, and adopting preventive measures, individuals can maintain their independence and mobility well into their later years. It is essential to prioritize spinal health and seek medical advice for symptoms that may indicate ankylosing spondylosis or other related conditions.
Understanding Spinal Anatomy and Joint Function: An In-Depth Exploration
The human spine is a complex structure that plays a vital role in our overall health and mobility. It is composed of various vertebrae, each serving a specific function. In this article, we will delve into the anatomy of the spine, the mechanics of joints, and the importance of maintaining joint health.
Anatomy of the Spine
The spine consists of several types of vertebrae, categorized based on their location:
1. Cervical Vertebrae
Located in the neck, the cervical vertebrae are the first set of vertebrae in the spinal column. Conditions such as cervical spondylosis are common in this region, often resulting from wear and tear over time. These vertebrae support the head and allow for a wide range of motion.
2. Thoracic Vertebrae
Below the cervical vertebrae are the thoracic vertebrae, which form the upper back. These vertebrae are attached to the ribs and provide stability and protection for the organs in the thoracic cavity.
3. Lumbar Vertebrae
The lumbar vertebrae are found in the lower back and are larger and stronger than the other vertebrae, as they bear most of the body’s weight. Issues like lumbar spondylosis can occur due to strain and wear in this region.
4. Sacral and Coccygeal Vertebrae
The final segments of the spine are the sacral vertebrae, which form the back of the pelvis, and the coccygeal vertebrae, commonly known as the tailbone. Together, they contribute to pelvic stability and support.
Function of Joints in the Spine
The joints between the vertebrae are critical for both mobility and stability. These joints enable various movements while protecting the spinal cord and surrounding structures.
Intervertebral Discs
One of the most important components of spinal joints is the intervertebral discs. These discs act as shock absorbers between the vertebrae, preventing them from grinding against each other during movement. The discs are composed of a gel-like substance that allows for smooth movement and flexibility. Damage to these discs can lead to significant discomfort and pain.
The intervertebral discs have two primary types of collagen—type one and type two—that help maintain their structure and function. When the discs become damaged, it can lead to conditions like herniated discs, which can cause pain and limited mobility.
Importance of Synovial Fluid
In addition to intervertebral discs, the joints in the spine contain synovial fluid, which lubricates the joints, preventing friction. This fluid is crucial for maintaining joint health and function.
When the levels of synovial fluid decrease, individuals may experience stiffness and pain. In some cases, healthcare providers may recommend injections to replenish the synovial fluid, thereby reducing friction and discomfort.
The Role of Joint Capsules
Joint capsules are protective structures surrounding the joints. They help contain synovial fluid and maintain joint stability. During movement, these capsules stretch, which can sometimes create a popping or cracking sound, known as crepitus. This phenomenon is generally harmless but can indicate underlying issues if accompanied by pain.
Movement and Joint Sounds
Certain movements, such as stretching or lifting heavy objects, can produce sounds in the joints. These sounds occur when the joint capsule stretches and pressure changes within the joint space. Additionally, fluctuations in hydration levels can impact joint function and the sounds produced during movement.
Ayurvedic Perspective
In Ayurveda, the balance of bodily fluids and structures is essential for overall health. An imbalance can lead to joint issues and discomfort. Understanding these principles can guide individuals in maintaining joint health through lifestyle choices.
The spine is a remarkable structure composed of various vertebrae and joints that allow for movement and stability. Understanding spinal anatomy and joint function is crucial for maintaining overall health and preventing pain. Regular exercise, proper hydration, and awareness of body mechanics can contribute to the longevity and well-being of our spinal health. If you experience persistent discomfort or mobility issues, consulting a healthcare professional is essential for proper diagnosis and treatment.
Understanding the Spinal Joints and Related Disorders
The human spine is a remarkable structure, functioning not only as a support system for our body but also as a complex mechanism that enables movement. It comprises various joints and vertebrae, each playing a crucial role in our physical activities. This article explores the anatomy of spinal joints, the impact of inflammation, and specific conditions such as ankylosing spondylitis.
The Role of the Nervous System
The brain communicates with the body through the nervous system, sending messages that guide our movements. For instance, when performing a task, the brain instructs our muscles to grip, lift, or move in specific ways. This coordinated action involves a network of nerves that control the range of motion in the spine.
The Impact of Inflammation
Over time, chronic inflammation can lead to the deterioration of spinal joints, including intervertebral joints, facet joints, and sacroiliac joints. Many individuals often overlook initial joint pain, thinking it is a minor issue that can be alleviated with over-the-counter painkillers. However, neglecting these warning signs can exacerbate the underlying problem, leading to further joint degradation.
The Consequences of Joint Damage
When joints are subjected to continuous pressure without adequate care, inflammation can persist and cause significant damage. As inflammation progresses, it can result in the destruction of three major types of joints in the spine:
- Intervertebral Joints: Located between vertebrae, these joints allow for flexibility and movement.
- Facet Joints: These are located at the back of the spine and help stabilize and guide movement.
- Sacroiliac Joints: Connecting the spine to the pelvis, these joints absorb shock and provide support during movement.
Fibroblasts, cells involved in tissue repair, may replace damaged joint tissue with fibrin, leading to restricted movement and increased pain over time.
Fibrous Bands and Range of Motion
The fibrous bands around the joints serve a critical purpose: they limit the range of motion to prevent injury. For instance, when attempting to bend at a specific angle, these bands help control the movement, ensuring it does not exceed safe limits. This mechanism prevents the joints from collapsing or overextending.
The Process of Ossification
Ossification is the process through which fibro tissues can turn into bone, leading to immobility in the affected area. This transformation can significantly affect the flexibility and function of the spine.
Ankylosing Spondylitis: A Case Study
Ankylosing spondylitis is a specific inflammatory condition that primarily affects the spine, leading to severe pain and stiffness. Here are some key symptoms associated with this condition:
- Sudden Weight Loss: Patients may experience unexpected weight loss.
- Fever and Fatigue: Persistent fatigue and occasional fever can accompany the condition.
- Buttock Pain: Known as sacroiliac pain, discomfort in the buttocks region is common. Sitting on hard surfaces may exacerbate this pain, requiring individuals to seek softer seating options for relief.
- Cervical and Thoracic Pain: Pain may also extend to the cervical (neck) and thoracic (upper back) regions, often accompanied by stiffness. In some cases, patients may experience shortness of breath or a feeling of fatigue due to thoracic pain, as it can affect lung function.
Understanding the anatomy and functionality of spinal joints is crucial for maintaining spinal health. Ignoring early signs of joint pain can lead to more severe issues over time. Awareness of conditions such as ankylosing spondylitis and their symptoms is essential for early detection and intervention. If you experience persistent pain or mobility issues, seeking medical advice is vital to ensure proper diagnosis and treatment.
Understanding Spinal and Joint Disorders: Diagnosis, Genetic Factors, and Treatment Options

Spinal and joint disorders can be influenced by various factors, including genetic predispositions, fatty tissue inside the body, and autoimmune processes. A comprehensive approach to diagnosing and treating these conditions is necessary to manage symptoms effectively and improve patients’ quality of life.
Fatty Tissue and its Role in Joint Health
Fatty tissue within the body plays a role in several joint-related conditions. Excessive fatty deposits around the joints can aggravate inflammation, leading to restricted movement and discomfort. Additionally, this can impact the overall health of the skeletal system, potentially contributing to conditions like osteoarthritis, where the joint cartilage deteriorates, or other inflammatory disorders. Fatty tissue can also interact with the body’s immune system, contributing to autoimmune conditions that affect joints and the spine.
The Role of Genetic Factors: HLAB 27 Gene
One significant genetic factor that may contribute to spinal and joint issues is the HLAB 27 gene. This gene is associated with certain autoimmune conditions that can affect the spine and joints, most notably ankylosing spondylitis (AS). Ankylosing spondylitis is an inflammatory disease that primarily affects the spine, leading to the fusion of vertebrae, often referred to as “bamboo spine.” This condition can cause stiffness, pain, and restricted mobility over time.
The HLAB 27 gene predisposes individuals to autoimmune attacks, specifically targeting the vertebral joints. The immune system, instead of protecting the body, begins attacking healthy tissues, leading to inflammation and degradation of joints. When vertebrae are damaged, they are often replaced by fibrous tissue, which can further stiffen the spine and restrict movement.
Diagnostic Methods: MRI, CT Scans, and Genetic Testing
Proper diagnosis of spinal and joint disorders requires a detailed examination of the affected areas. Several diagnostic methods help pinpoint the problem:
- MRI (Magnetic Resonance Imaging): MRI is one of the most accurate tools for diagnosing joint and spinal conditions. It helps detect narrowing of joint spaces, joint fusion, and erosion. MRI scans provide detailed images of soft tissues, which is critical for understanding the extent of damage in the joints and spine.
- CT Scans and X-rays: These imaging techniques help detect structural changes in the bones, such as the formation of abnormal bony growths or loss of vertebral density. They also aid in identifying the presence of fluid buildup or “annulus,” which can contribute to stiffness and pain.
- Genetic Testing: When traditional diagnostic methods do not yield conclusive results, genetic testing may be recommended to detect the presence of the HLAB 27 gene. If this gene is positive, it indicates a higher likelihood of developing conditions like ankylosing spondylitis. However, it’s important to note that while genetic testing can reveal a predisposition, it cannot reverse or cure the genetic condition.
Autoimmune Conditions and Their Impact on the Body
Autoimmune conditions like those related to the HLAB 27 gene can affect more than just the joints. In some cases, the disease may gradually impact other organs, including the eyes, aorta, tendons, muscles, and lungs. Though rare, the possibility of these organs being affected underscores the importance of early detection and management.
Treatment Approaches: From Medication to Surgery
Treatment for spinal and joint disorders typically involves a combination of medication, physical therapy, and, in severe cases, surgery. While the genetic component of diseases like ankylosing spondylitis cannot be reversed, treatment focuses on managing symptoms and maintaining mobility.
- Medications:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Commonly prescribed medications like ibuprofen help reduce inflammation and pain in affected joints. These drugs can help manage symptoms, allowing individuals to maintain daily activities with less discomfort.
- Anti-Rheumatoid Drugs: In cases where inflammation is severe, medications such as methotrexate or sulfasalazine are used to reduce joint damage and slow disease progression. These drugs are typically prescribed by rheumatologists and require regular monitoring due to their potential side effects.
- Steroid Injections: In more advanced cases, patients may be given steroid injections to control inflammation and pain in the joints. These injections provide temporary relief but may need to be repeated periodically.
- Physical Therapy and Exercise:
- Physiotherapy: Both medical professionals and naturopaths agree that physical therapy plays a crucial role in managing spinal and joint disorders. Regular physiotherapy sessions can improve mobility, reduce stiffness, and strengthen the muscles supporting the spine. This is especially important for conditions like ankylosing spondylitis, where maintaining flexibility is key to preventing long-term immobility.
- Exercise Regimens: A well-designed exercise program, focusing on stretching, strengthening, and posture improvement, can help reduce stiffness and keep the spine as flexible as possible.
- Surgical Intervention: Surgery is considered the last resort in treating spinal disorders. It is typically recommended only when all other treatment options have failed and the condition significantly impairs quality of life.
- Spinal Surgery: Spinal surgeries are risky, and surgeons usually avoid them unless there is extensive damage to the vertebrae or other critical areas. Surgeries may involve correcting deformities, stabilizing the spine, or relieving pressure on nerves. However, spinal surgery is one of the riskiest procedures and is recommended in only 2-5% of cases where other treatments have not succeeded.
- Joint Replacement: In severe cases where the hip or knee joints are affected, joint replacement surgery may be recommended. Hip and knee replacements are more common than spinal surgeries and generally have a higher success rate in restoring mobility and reducing pain.
Naturopathy for Managing Health Conditions: Insights on Natural Therapies
Naturopathy is an alternative medicine approach that emphasizes the body’s intrinsic ability to heal itself. This holistic form of treatment focuses on natural remedies, lifestyle changes, and preventative care. Among the various conditions treated through naturopathy, there is a growing interest in how it can aid patients with chronic diseases such as arthritis, diabetes, and obesity. In this article, we will explore how naturopathic therapies can assist in managing symptoms, improving quality of life, and promoting overall well-being.
Understanding Naturopathy
Naturopathy blends traditional healing practices with modern science, utilizing a range of natural therapies. Key components of naturopathy include:
- Diet and Nutrition: Emphasizing whole foods, easy-to-digest meals, and balanced diets to prevent diseases and promote healing.
- Hydrotherapy: Utilizing water treatments to alleviate pain and improve circulation.
- Herbal Medicine: Employing various plants and herbs known for their medicinal properties to treat ailments.
- Physical Therapies: Incorporating practices such as massage, acupuncture, and yoga to enhance physical well-being.
- Lifestyle Modifications: Advocating for changes in daily habits to support health and prevent diseases.
Role of Naturopathy in Chronic Conditions
Naturopathy can play a significant role in managing chronic conditions by balancing symptoms and enhancing the body’s natural healing process. Here are several naturopathic treatments that can benefit patients:
- Cow Urine Therapy: Cow urine therapy is a traditional practice believed to possess healing properties. It is often suggested to use cow urine extract, which is more hygienic and less acidic than direct consumption.
- How to Use: It is recommended to consume two tablespoons of filtered cow urine mixed with four tablespoons of water on an empty stomach, preferably in the morning. For those who can, adding honey can enhance its benefits.
- Benefits: Cow urine is believed to help detoxify the body, boost immunity, and maintain pH balance.
- Mud Therapy: Mud applications have been used for their cooling and therapeutic properties.
- Application: Mud can be applied to areas of inflammation or pain, providing relief and promoting healing.
- Benefits: The minerals present in mud help in reducing inflammation, absorbing excess heat, and soothing the affected area.
- Therapeutic Massage: Professional massage therapy can stimulate circulation, relieve tension, and enhance relaxation.
- Technique: Gentle massage with oils such as black seed or castor oil can be particularly beneficial.
- Frequency: Regular sessions, ideally once or twice a week, can greatly improve overall well-being.
- Physical Exercises and Yoga: Regular physical activity is crucial for maintaining health, especially for those with chronic pain or stiffness.
- Recommended Asanas: Specific yoga postures can help in improving flexibility, strength, and overall health. Engaging with a qualified yoga instructor ensures that the poses are suitable for the individual’s health conditions.
- Dietary Adjustments:
- Early Dinner: A significant principle in naturopathy is having an early dinner, ideally before sunset. This practice helps in better digestion and metabolism.
- Balanced Nutrition: Consuming easy-to-digest foods supports better absorption of nutrients and minimizes digestive issues.
Naturopathy offers a comprehensive approach to managing chronic conditions. By focusing on natural therapies, lifestyle adjustments, and preventive measures, it can help improve the quality of life for patients suffering from various health challenges. Individuals interested in exploring naturopathic treatments should consult with qualified practitioners to tailor a plan that best suits their needs and health conditions. This holistic approach, grounded in the principles of nature, can empower patients to take control of their health and promote long-lasting wellness.
The Health Benefits of Whole Barley and Natural Remedies for Digestive Health
In today’s fast-paced world, many people struggle with digestive issues, often exacerbated by poor dietary choices and sedentary lifestyles. However, incorporating natural remedies and whole grains into our diets can significantly improve digestive health and overall well-being. This article explores the benefits of whole barley, various natural remedies, and dietary suggestions for maintaining digestive health.
The Case for Whole Barley
Nutritional Benefits
Whole barley is a nutrient-dense grain that offers numerous health benefits. It is high in fiber, which aids digestion and helps maintain a healthy gut. The fibrous content in barley assists in the smooth transit of food through the digestive tract, reducing constipation and enhancing nutrient absorption.
Easy to Digest
Unlike processed grains like white wheat, whole barley contains its outer bran layer, making it easier for the body to digest. The fibrous cover promotes gut health by fostering beneficial bacteria in the intestines, which further supports digestion and nutrient absorption.
Incorporating Barley into Your Diet
To reap the benefits of whole barley, consider incorporating it into your daily meals. It can be boiled and added to salads or consumed as a warm porridge. Additionally, barley water is a refreshing beverage that provides hydration along with its digestive benefits. Drinking barley water regularly can also help in kidney health by aiding in stone prevention and removal.
Other Beneficial Foods
Broccoli and White Pill
In addition to barley, other foods such as broccoli can be effective in promoting digestive health. Including these vegetables regularly in your diet can bolster your immune system and contribute to overall wellness.
Mukwash and Seeds
In many cultures, it is customary to consume mukwash (a digestive mix of seeds) after meals. Adding ingredients like soft teel (sesame seeds) and ajwain (carom seeds) can help improve digestion. Health-conscious individuals often add flaxseeds and sunflower seeds for added fiber and nutrients.
Avoiding Certain Foods
To maintain optimal digestive health, it’s advisable to limit the intake of processed and oily foods. Non-vegetarian protein sources should be minimized in favor of plant-based proteins, which are easier for the body to digest. Reducing consumption of bakery products and high-fat foods can also prevent digestive discomfort.
Natural Remedies for Digestive Health

Ginger and Turmeric
Ginger and turmeric (haldi) are potent natural remedies known for their anti-inflammatory and digestive benefits. Ginger tea or a paste made from ginger and turmeric can be consumed daily to help with digestion and alleviate discomfort.
Barley Water
Barley water is particularly beneficial for individuals with kidney stones or renal issues. Regular consumption can help dissolve stones and reduce the need for surgical interventions. Aim to drink approximately 100 ml of barley water daily for maximum benefits.
Moringa and Alfalfa
Moringa leaves and powder are recognized for their rich nutritional profile. They can be consumed in various forms, including fresh leaves or powdered supplements. Similarly, alfalfa is another superfood that provides calcium and promotes bone health. Incorporating these herbs into your diet can enhance your overall health and support digestion.
Dosage and Usage
When using herbal supplements, it is essential to follow proper dosage guidelines to avoid adverse effects. A teaspoon of moringa powder can be soaked in water overnight and consumed the next morning for optimal health benefits.
Incorporating whole grains like barley, along with various natural remedies and foods, can significantly enhance digestive health. Adopting a diet rich in fiber, vitamins, and minerals while avoiding processed foods can help alleviate digestive issues and promote overall well-being. By embracing the gifts of nature, we can pave the way for a healthier lifestyle, particularly in an era where digestive disorders are increasingly common.
By prioritizing natural remedies and a wholesome diet, individuals can experience improved digestive health and overall vitality. It is crucial to remember that dietary changes should be made with care and, if necessary, under the guidance of a healthcare professional.
Conclusion:
Maintaining digestive health is crucial for overall well-being, especially in a world where unhealthy eating habits are prevalent. Incorporating whole grains like barley into our diets can provide significant benefits, including improved digestion, enhanced nutrient absorption, and support for gut health. Alongside dietary adjustments, natural remedies such as ginger, turmeric, and various seeds can further promote digestive wellness.
As we strive for better health, it’s essential to prioritize nutrient-dense foods while limiting processed options that can hinder our digestive systems. By embracing a holistic approach to nutrition, we can foster a healthier lifestyle that not only alleviates digestive issues but also enhances our quality of life.
Ultimately, making informed dietary choices, utilizing natural remedies, and listening to our bodies can pave the way for a healthier future. With commitment and awareness, we can navigate the complexities of modern diets and reclaim our digestive health, leading to a happier and more vibrant life.