LIVER CIRRHOSIS
LIVER CIRRHOSIS
Liver cirrhosis, also known simply as cirrhosis, is a chronic condition that affects the liver, which is often hailed as the “chemical factory” of the human body. Responsible for producing hormones and vital biochemicals, the liver plays a pivotal role in maintaining overall health. It is one of the largest organs in the body, both in terms of size and weight, highlighting its significance in bodily functions.
Unlike other organs, such as the heart or kidneys, which exhibit immediate signs of damage, the liver possesses remarkable regenerative capabilities. This is attributed to its high concentration of regenerative cells, allowing it to repair and rejuvenate damaged tissue over time. However, despite its resilience, liver cirrhosis remains a significant global health concern.
Statistics reveal that approximately 1 million people worldwide succumb to the complications of liver cirrhosis annually, with countless others grappling with its debilitating effects. In fact, among all diseases, liver cirrhosis ranks as the 11th most common cause of death globally, underscoring the urgent need for heightened awareness and proactive management strategies.
This silent yet formidable adversary demands attention not only from healthcare professionals but also from policymakers and the public. By fostering greater understanding of liver cirrhosis and its underlying causes, we can strive towards early detection, effective treatment, and ultimately, the prevention of needless suffering and loss of life.
Furthermore, the liver’s remarkable regenerative capacity underscores its importance in maintaining overall health. Unlike many other organs, the liver can repair and rejuvenate itself, given the right conditions. However, this regenerative ability can be hindered by factors such as chronic alcohol consumption, viral infections, and fatty liver disease, all of which contribute to the development of cirrhosis.

Bile production, another vital function of the liver, aids in the digestion and absorption of fats and fat-soluble vitamins. Stored in the gallbladder and released as needed, bile plays a crucial role in the breakdown of food and the transport of nutrients throughout the body.
Given the liver’s central role in numerous bodily functions, including metabolism, detoxification, and nutrient processing, it is essential to prioritize its health through preventive measures. By promoting awareness of liver cirrhosis and its risk factors, as well as advocating for regular screenings and healthy lifestyle choices, individuals can take proactive steps to safeguard their liver health and overall well-being.
The liver serves a multifaceted role in the body, including the breakdown of fats into essential fatty acids, crucial for proper digestion. Without fatty acids, digestion becomes impaired. Bile production, facilitated by the liver, aids in this breakdown process and is indispensable for nutrient absorption in the digestive tract.
Another vital function of the liver is the excretion of drugs, hormones, and bilirubin. The liver removes inactive steroid hormones, which would otherwise burden the kidneys and impact nephron function. Additionally, bilirubin elimination from plasma by the liver helps maintain optimal plasma levels, ensuring metabolic balance.
Liver function extends to detoxification and metabolism, pivotal processes for overall health. By metabolizing fats, proteins, and carbohydrates, the liver supports balanced metabolic rates essential for weight management, digestion, and overall vitality.
Understanding the intricate functions of the liver underscores its significance in maintaining bodily functions and highlights the importance of prioritizing liver health through preventive measures and lifestyle choices.

Indeed, dietary fats play a crucial role in safeguarding our organs, forming a protective layer around them. Proteins, essential for bodybuilding and brain function, along with carbohydrates, which provide the energy needed for work, are metabolized with the assistance of the liver.
Enzyme activation, initiated from the mouth with saliva, is vital for breaking down nutrients. For instance, enzymes like fructose two respond to hormonal signals, such as glucagon, illustrating the intricate workings of enzyme activation throughout the body.
The liver’s contribution extends to storing vitamins, glycogen, and minerals, serving as a reservoir for essential nutrients. In times of fasting or inadequate nutrient intake, the liver taps into these reserves, ensuring the body functions systematically and optimally.
Understanding the liver’s role in nutrient metabolism and storage underscores its importance in maintaining overall health and vitality. By prioritizing liver health through a balanced diet, adequate hydration, and lifestyle choices, individuals can optimize their body’s functioning and well-being.
Lack of adequate storage can lead to deficiencies, resulting in weakness or breakdowns. Having sufficient storage ensures a buffer against such situations, providing a safety net for our overall well-being.
The liver’s role in synthesizing plasma proteins, including albumin, globulin, fibroin, and protons, cannot be overstated. These proteins are fundamental to the structure and function of our body’s cells, highlighting the critical importance of the liver in maintaining bodily functions.
While the heart, kidneys, and other organs may seem to perform more visible functions, their proper functioning relies heavily on the liver’s support. The liver’s ability to regulate essential processes ensures the balance and health of the entire body.
Understanding the consequences of liver damage, particularly when it reaches significant levels, underscores the importance of prevention. Once the liver is compromised, maintaining optimal health becomes challenging, emphasizing the significance of proactive liver care.
Prioritizing liver health through preventive measures is essential for overall well-being. By recognizing the liver’s pivotal role and taking proactive steps to preserve its function, individuals can safeguard their health and vitality for the long term.
Various factors contribute to the development of liver cirrhosis, with alcohol consumption being a primary culprit. Regular and excessive alcohol intake exceeds the body’s capacity to metabolize it, leading to increased pressure on organs and causing liver damage. Alcohol’s acidity and the body’s lack of enzymes to digest it exacerbate its harmful effects.
Cigarette smoking, obesity, and high blood pressure are also significant contributors to liver damage. Obesity poses a substantial risk as it leads to the accumulation of fatty cells, burdening organs and impairing their function. Maintaining a healthy weight and blood pressure levels is crucial for liver health.
Recognizing the detrimental effects of these lifestyle factors is essential for preventing liver cirrhosis. By adopting healthier habits, such as reducing alcohol consumption, quitting smoking, managing weight, and controlling blood pressure, individuals can mitigate their risk of developing liver cirrhosis and promote overall liver health.

Another significant contributor to liver damage is hypertension, particularly among individuals who have been on heavy medication to control their blood pressure for an extended period. Uncontrolled hypertension can damage arteries, including those in the kidneys, ultimately affecting liver function. Similarly, long-term uncontrolled diabetes can lead to liver damage, as the organ becomes burdened with excessive secretions due to unregulated sugar levels.
Cholesterol levels also play a role in liver health, especially in conjunction with conditions like hypertension and diabetes. Often, imbalances in one of these factors can lead to the exacerbation of the others, demonstrating the interconnected nature of these health issues. Therefore, it’s crucial to prioritize the natural management of blood pressure, diabetes, and cholesterol to prevent further complications.
Hepatitis B and C infections pose another significant risk to liver health, leading to inflammation and damage to the liver. However, advancements in both conventional medicine and naturopathy offer effective treatments to reverse or cure these viral infections. Individuals with a history of hepatitis are particularly vulnerable to liver-related complications and should prioritize proactive measures to maintain liver health.
Improper diet and lifestyle habits, particularly excessive fat consumption, contribute significantly to liver damage, potentially leading to liver cirrhosis. Accumulation of excessive fat in the liver can obstruct its functions and trigger conditions like liver psoriasis.
Symptoms of liver damage, including cirrhosis, may manifest in various ways. Jaundice, characterized by yellowing of the skin and eyes, is a common indicator of liver problems. Weakness and fatigue, even after sufficient rest and nutrition, can also signal liver issues. Additionally, decreased appetite or anorexia may occur, with individuals experiencing a sudden loss of hunger or reduced food intake.
Recognizing these symptoms is crucial for early detection and intervention. Persistent or worsening symptoms should prompt further medical evaluation to address potential liver damage and prevent complications.
Very suddenly, your appetite may diminish or become very low, even after consuming a small portion of food that you struggle to digest. This is often accompanied by unexplained itching, occurring anywhere on the skin without any apparent allergen or skin disease present. Itching may persist in areas with bulging fatty tissues, such as the hands, face, abdomen, groin, or thighs, leading to continuous discomfort. In some cases, individuals require medication like Allegra to alleviate itching and facilitate sleep, especially as these symptoms tend to worsen at night, disrupting sleep patterns.
Disrupted sleep can further exacerbate the situation, as inadequate rest can lead to thinning skin and increased susceptibility to bleeding, such as bleeding gums during brushing. Despite dental reassurances of no oral health issues, persistent gum bleeding can persist, indicating underlying liver damage affecting blood clotting factors. These symptoms serve as important indicators of liver damage or cirrhosis, necessitating medical attention for diagnosis and management.

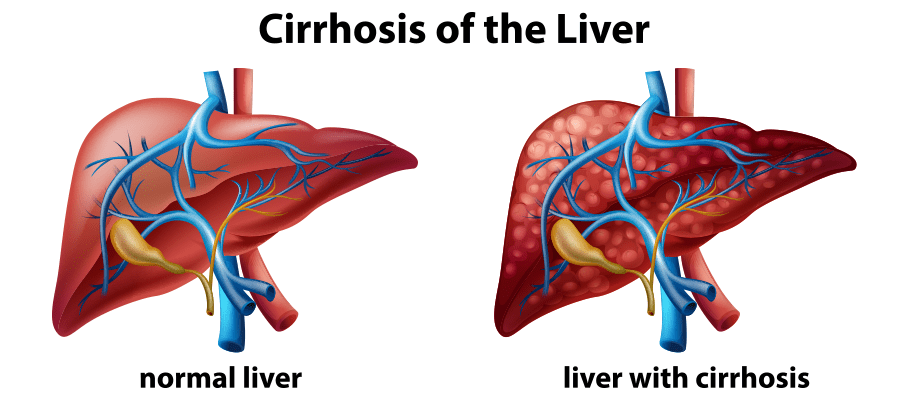
Different stages of liver damage can be observed from a diagnostic perspective to determine the appropriate treatment approach by liver specialists or MD doctors. Each stage presents distinct symptoms, guiding physicians in assessing the extent of liver damage and the potential for salvaging liver function or the need for a transplant.
While science and alternative therapies have their limitations, caution should be exercised, especially in chronic cases like liver cirrhosis, where abruptly stopping ongoing medications can lead to complications. Gradual reduction or cessation of medications should be based on symptom improvement and patient vitality.
Naturopathy and parallel medicine can complement allopathic treatments, aiding in detoxification and minimizing medication side effects. The detoxification process is ongoing, contributing to overall liver health.
Preventive measures are crucial, particularly for those over 40 and health-conscious individuals, to invest in their well-being and address symptoms early. Liver damage typically progresses through stages, starting with inflammation, leading to scarring, and eventually culminating in cirrhosis over several months to years, depending on treatment adherence and lifestyle factors.
Diet plays a pivotal role in liver health, with approximately 80% of therapy focusing on dietary interventions, making it a critical tool in managing liver problems and preventing further damage.
Let’s explore how science categorizes the different stages of liver damage. In stage one, liver scarring may occur, but symptoms are minimal, rendering it a compensated cirrhosis stage. At this stage, liver damage is potentially reversible, and complications are rare. However, it’s crucial to seek medical attention upon experiencing any symptoms or signs of liver problems to prevent progression.

Stage two marks the worsening of portal hypertension and the development of ascites. Portal hypertension involves increased pressure within the portal vein, leading to vein inflammation and hypertension. At this stage, it is still possible to reverse the condition, but vigilance is necessary to prevent advancement.
Stage three, termed decompensated cirrhosis or decompensated disease, signifies a significant progression of liver damage. Inflammation and ascites (fluid accumulation in the abdomen) are common symptoms. Ascites can cause abdominal bloating, visible as an enlargement of the stomach. Medical intervention becomes crucial at this stage to manage complications and prevent further deterioration.
Neglecting early stages can lead to the aggravation of liver damage, making it imperative to seek timely medical advice and monitoring. Decompensated cirrhosis poses significant risks, underscoring the importance of proactive healthcare measures and adherence to treatment protocols.
Serious complications, such as liver failure, are associated with this advanced stage, hence the term decompensated disease. However, until stage three, there remains a slim chance of recovery, albeit decreasing as the disease progresses. Stage three marks complete liver cirrhosis, where the liver undergoes significant damage, leading to life-threatening complications.
Complications can extend to other organs, including the kidneys, making a liver transplant imperative for survival. Without transplantation, longevity is severely compromised. Treatment approaches vary across the four stages, with doctors determining the appropriate course of action based on the severity of liver damage.
Organ transplantation, particularly in cases like liver transplants, poses significant challenges, especially considering the scarcity of donors. Hence, the importance of organ donation cannot be overstated. Donating organs after death can offer a lifeline to those battling for survival.
Maintaining good health is crucial for becoming an eligible organ donor. Conditions like diabetes can disqualify individuals from donating. Therefore, it’s essential to prioritize health to extend the possibility of posthumous organ donation and potentially save lives.
Advocating for organ donation is a noble cause, emphasizing the need for individuals to express their willingness to donate and encourage others to do the same. Medical practitioners, including natural therapists, homeopaths, and doctors, utilize various diagnostic tests like blood tests, sonography, elastography, and biopsies to assess liver health and guide treatment decisions.
Not all tests can be prescribed without the guidance of a specialist doctor; certain tests require their specific prescriptions. So, what tests are necessary to understand liver health? Firstly, an ultrasound sonography of the abdomen is essential to visualize the liver and detect any signs of portal hypertension. If the portal veins measure more than 12 mm in size, it indicates liver damage, which can only be diagnosed through sonography.
Once abnormalities are detected through ultrasound, the doctor may recommend specific blood tests. These include tests for hepatitis B and C viruses, liver function tests (LFT) measuring albumin, globulin ratio, SGPT, SGOT levels, serum ferritin, complete blood protein (CBP), and serum iron. Any naturopathic doctor can suggest or provide prescriptions for these blood tests, which can be conducted at any pathology lab.
If signs of liver cirrhosis or other liver abnormalities persist, the doctor may recommend liver elastography to assess liver stiffness and determine the stage of liver damage. If necessary, a liver biopsy may be performed to obtain tissue samples for further examination, typically in 10 to 15% of patients. A liver biopsy is particularly useful if there are suspicions of liver carcinoma or abnormal cell multiplication.
Upper gastrointestinal (GI) endoscopy is valuable in cases of bleeding, black stools, or blood vomiting, indicating potential complications such as esophageal varices. Additionally, a CT scan of the abdomen may be necessary to assess liver surface abnormalities comprehensively.
While initial tests like ultrasound and blood tests provide crucial insights into liver health, additional investigations such as liver elastography, biopsy, upper GI endoscopy, and CT scans may be required based on clinical suspicion and the progression of liver disease. These tests are instrumental in accurately diagnosing and monitoring liver conditions, facilitating appropriate treatment decisions.
After the ultrasound sonography (USG) and elastography, if the doctors have any doubts, they may suggest an abdominal CT scan to verify the stages of liver damage. Additionally, routine blood tests for hepatitis B and C are essential to understand liver function and determine the course of treatment.
Liver cirrhosis patients often seek alternative therapies like naturopathy, although they are relatively fewer in number compared to patients with other chronic conditions. Those who understand the importance of natural remedies or have faith in naturopathy may seek treatment in this field, often through referrals from previous patients.
Naturopathy offers specific therapies tailored to liver health, primarily focusing on dietary adjustments and mud applications on the stomach. Mud application is considered one of the best therapies for liver cirrhosis, regardless of its stage or type. Patients typically experience improvements in symptoms such as increased appetite, reduced weakness, and cessation of acid reflux shortly after beginning mud therapy.

Regular mud applications over a period of three to four months, preferably on an empty stomach every day, are strongly recommended to minimize symptoms and promote liver health. Monitoring the effectiveness of treatment through follow-up sonographies can reveal reductions in inflammation and portal hypertension, indicating the therapy’s success.
Naturopathic treatments, especially mud application therapy, offer promising outcomes for liver cirrhosis patients, emphasizing the importance of holistic approaches to health and wellness.
Mud application therapy not only yields the best results for patients but also offers additional benefits for overall well-being. Depending on the patient’s capacity, it is advisable to suggest 10 to 15 minutes of daily deep breathing exercises. This can help alleviate irritability, a common issue among liver cirrhosis patients due to difficulties with eating and digestion. Despite potential challenges in adopting new practices, it is the practitioner’s responsibility to recommend beneficial therapies.
Alongside deep breathing exercises, specific yoga asanas such as Ardha Matsyendrasana (Half Spinal Twist) and Bhujangasana (Cobra Pose) can be suggested, as they aid in improving digestion and liver health. Additionally, gastro-hepatic packs, which involve applying hot and cold packs alternately to the stomach and back, can be highly beneficial. This therapy helps reduce inflammation and discomfort, contributing to overall liver health improvement.
Sunbathing or sun gazing for five to fifteen minutes in the morning, between 6:00 AM to 8:00 AM, is recommended to increase vitamin D levels, which play a crucial role in cell regeneration and overall health. Dietary modifications, such as fasting or following a mono-diet, can also support liver health. However, it is essential to customize dietary recommendations based on individual patient needs and monitor their response closely.
Moreover, liver detoxification can be facilitated through the consumption of animal-based foods. However, it is crucial to limit animal-based diets to three to five days continuously and avoid experimentation. Warm water consumption is encouraged throughout these therapies to support the body’s natural detoxification processes.
Nature offers a myriad of therapeutic options for treating liver cirrhosis and related conditions. By incorporating holistic practices such as mud therapy, deep breathing, yoga, dietary adjustments, and controlled detoxification, practitioners can effectively support patients on their journey to improved liver health and overall wellness.

Turmeric, known as haldi in Asian cuisines, is a common spice and medicinal herb used in daily routines. Its curcumin-rich variety is particularly essential for liver health. It is advisable to provide organic, pure forms of turmeric, preferably raw. Consuming two to three inches of raw turmeric daily before meals can significantly benefit liver health. Alternatively, one can soak one teaspoon of turmeric in 100 ml of water overnight and consume it on an empty stomach in the morning. Aloe vera, another miracle herb for treating liver diseases, should be sourced organically. Fresh aloe vera pulp or organic aloe vera juice can be consumed twice daily, preferably after breakfast and 30 minutes after dinner.
Another beneficial herb is Amrutha (Tinospora cordifolia), commonly known as Guduchi or Giloy. Freshly available herbs provide the best results. If fresh herbs are not accessible, one can opt for powdered or tablet forms. Another helpful herb is Punarnava (Boerhavia Diffusa), which can be consumed in various forms such as fresh juice, tablets, or powder.
Una, also known as diffuse cap (Andrographis paniculata), is another useful herb for liver health. It can be consumed as fresh juice or in tablet or powder form if fresh juice is not available. Additionally, Ana tablet or powder is also beneficial and readily available.
At Saffron, we are blessed with access to natural herbs due to Saffron4Health Private Limited’s organic farm. Fresh herbs are directly provided to patients, contributing to favorable outcomes in treating liver diseases. These herbs, when used in their purest forms, offer significant support for liver health and overall well-being.
Whatever herbs are available, whether they are known by common names or botanical terms, can be beneficial for treating liver damage. One such herb belongs to the family of ura, known as s Mariana. These herbs are highly effective in reversing and regenerating liver cells. Alongside therapy, incorporating these herbs into one’s regimen can yield tremendous results without any side effects.
Another essential aspect in treating liver diseases is diet. The right food, along with these herbs, plays a crucial role in the healing process. Our experience and knowledge, derived from Ayurveda, emphasize the significance of natural health medicines. To delve deeper into this knowledge, one can refer to the Ayurveda scriptures, such as the Aria Bishop, which provide comprehensive information about natural remedies.
These herbs are thoroughly researched and can be administered in various forms based on availability. Whether it’s fresh herbs, powders, tablets, or juices, their efficacy remains consistent. The availability of resources like the Aria Bishop, accessible in multiple languages including English, ensures that this valuable information reaches a wider audience.
In conclusion, by incorporating these herbs into treatment plans and adhering to a balanced diet, individuals can effectively combat liver cirrhosis and promote overall well-being.