Liver Diseases
Introduction to Liver and Its Importance in Our Body
Welcome to Saffron Educational and Medical Foundation — An opportunity to be your own doctor.
Before beginning every lecture, students are informed that for any doubts related to the curriculum, clerical matters, upcoming examinations, or study-related queries, they can always stay in touch with our support team through the provided contact numbers, email ID, and official links. These details are shared multiple times during and at the end of the lecture to ensure easy access for every student, as all learners are equally important to us.
With this, let us begin today’s lecture.
Overview of the Liver
Today’s topic focuses on liver diseases, and to understand them properly, it is essential to first understand the liver itself—its position, structure, and role in the human body.
The liver is the largest internal organ and is often referred to as the biggest chemical factory of the human body. Almost all essential enzymes, hormones, and biochemical substances required to regulate and maintain bodily functions are either produced or processed by the liver. It plays a central role in maintaining overall health.
The liver is directly connected to multiple organs and systems in the body, which is why its proper functioning is crucial for the regulation and balance of the entire body.
The Unique Nature of the Liver
One of the most remarkable features of the liver is its regenerative capacity. Unlike organs such as the kidneys or heart—where damage often leads to chronic conditions or the need for complete organ replacement—the liver has the ability to regenerate.
If a small part of the liver is damaged or surgically removed, the remaining portion can still function efficiently and gradually regenerate. This extraordinary ability makes the liver a unique and precious organ, truly a gift of nature.
Because of this, it is absolutely true to say that the entire body is highly dependent on the liver for survival and well-being.
Functions and Role of the Liver
Understanding the functions of the liver helps us appreciate why it is so vital to our health.
- Bile Production and Digestion
One of the primary functions of the liver is bile production. Bile plays a crucial role in the digestive system.
Bile secreted from the liver helps in:
- Proper digestion of food
- Breakdown of fats
- Absorption of nutrients
When food enters the stomach and intestines, bile assists in converting complex food substances into simpler forms that the body can absorb. If bile secretion is either insufficient or excessive, it can lead to digestive disturbances and negatively affect gut health.
Improper bile secretion may result in:
- Poor digestion
- Nutrient malabsorption
- Digestive discomfort
- Disturbance in overall gut health
Therefore, for a healthy digestive system, the liver must secrete bile in the required and balanced amount.
Liver and Gut Health: A Direct Connection
The liver and gut health are directly related to each other. A healthy liver supports a healthy digestive system, and any imbalance in liver function can directly affect gut health, digestion, and overall metabolism.
Detoxification and Excretion Functions of the Liver
One of the most important functions of the liver is the excretion and detoxification of harmful substances. The liver continuously works—365 days a year, without rest—to process and eliminate:
- Drugs and medications
- Hormones
- Bilirubin
- Metabolic waste products
- Environmental and internal toxins
The liver plays a central role in detoxifying the body. Periodic detoxification, especially focused on liver health, helps the body function more efficiently. When the liver functions optimally, many common issues such as hormonal imbalance, indigestion, gas, and acidity can be reduced.
When the entire system works in harmony—hormones are properly secreted, toxin levels are controlled, and metabolic balance is maintained—the body becomes more resilient. Proper detoxification also helps reduce the burden of side effects in individuals who are already taking medications.
In short, detoxification primarily happens through liver secretions. While detoxifying water or foods may support the process, complete cleansing of the body ultimately depends on the liver’s natural detoxifying mechanisms.
Role of the Liver in Metabolism
Another major role of the liver is the metabolism of nutrients, including:
- Fats
- Carbohydrates
- Proteins
We eat food to obtain proper nutrition that supports every organ and system in the body. Each nutrient has a specific purpose:
- Fats (especially good fats) are essential for cell walls, brain health, and energy storage
- Carbohydrates provide energy and stamina
- Proteins are essential for muscle health, organ function, enzyme activity, and hormone formation
Even hormones require specific types of proteins for their formation.

Importance of Protein, Fats, and Carbohydrates
Protein plays a critical role in maintaining:
- Muscle strength
- Organ health
- Hormonal balance
- Overall body function
When protein deficiency begins, common symptoms include:
- Low energy and lethargy
- Muscle pain
- Fatigue
- Weakness
These three nutrients—proteins, fats, and carbohydrates—are essential for proper functioning of the body, and their metabolism must be carried out efficiently by the liver.
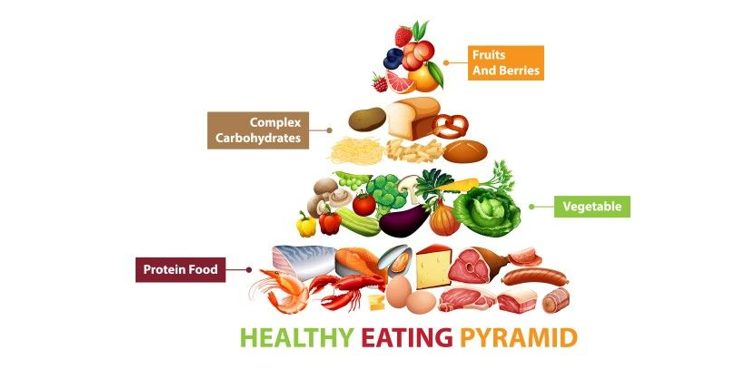
Dietary Sources of Essential Nutrients
For vegetarians, excellent sources of protein include:
- Paneer
- Tofu
- Pulses such as moong, matki, chana, chickpeas, and other legumes
Healthy fats can be obtained from:
- Cow ghee (clarified butter)
- Nuts and seeds
Carbohydrates are naturally supplied through:
- Food grains and cereals
When these nutrients are consumed in proper quantity and right combinations, it is often said that one is following a balanced and nutritious diet.
Importance of Proper Metabolism and Absorption
However, merely consuming nutritious food is not enough. If:
- Metabolism is weak
- Digestion is improper
- Absorption does not occur efficiently
Then despite eating a healthy diet, the body may still remain in a deficient state. This can result in:
- Persistent fatigue
- Low energy levels
- Muscle pain
- Poor stamina
- Effects on heart and overall organ health
Thus, for nutrients to truly benefit the body, their metabolism must be carried out effectively, and this process is primarily managed by the liver.
Role of the Liver in Enzyme Secretion and Nutrient Metabolism
The liver secretes various chemicals and enzymes that are essential for the metabolism of fats, carbohydrates, and proteins. These secretions help break down nutrients into simpler forms so that the body can absorb them efficiently. Without proper liver enzyme activity, nutrient absorption becomes difficult, even if a person consumes a nutritious and balanced diet.
Enzyme Activation and Digestive Health
Enzyme activation is another vital function of the liver. Digestion begins in the mouth, where saliva—naturally alkaline—initiates the digestive process. This marks the first step of the digestive system.
For digestion to proceed smoothly throughout the gastrointestinal tract, enzymes must be:
- Properly activated
- Secreted in adequate quantity
If enzyme secretion or activation is inadequate, the body fails to utilize food effectively. As a result, despite consuming high-quality and nutritious food, individuals may still experience weakness, fatigue, or deficiency symptoms. Once again, this entire process is strongly dependent on proper liver function.
Homeostasis and Blood Glucose Regulation
One of the most crucial roles of the liver is maintaining homeostasis, especially blood glucose regulation. The liver helps balance blood sugar levels after food intake by storing and releasing glucose as required.
If this regulatory mechanism fails, metabolic imbalance occurs, leading to conditions such as diabetes mellitus. This is why diabetes is often referred to as a metabolic disorder and, more specifically, a liver-related disorder, as blood glucose regulation is directly controlled by liver function.
Liver’s Role in Diabetes Management
In Type 2 diabetes, the primary therapeutic focus should be on improving liver function. When liver secretions and metabolic activity are normalized:
- Blood glucose regulation becomes easier
- Insulin sensitivity improves
- Better glycemic control is achieved
As a result, HbA1c (glycosylated hemoglobin) levels can be effectively maintained. Ideally, HbA1c should remain between 6.0 to 6.5, indicating controlled blood sugar levels over time.
Therefore, in managing or reversing Type 2 diabetes, cleansing and strengthening liver function is a critical first step.
Liver as a Storage House of Essential Nutrients
The liver acts as the largest storage organ for essential vitamins and minerals required by the body. It stores:
- Fat-soluble vitamins: A, D, E, K
- Water-soluble vitamins: B12
- Various essential minerals
Importance of Stored Vitamins
- Vitamin K is essential for proper blood clotting. Deficiency can lead to excessive bleeding and delayed clot formation after injury.
- Vitamin A and E support skin, eye health, and immunity.
- Vitamin D3 and Vitamin B12 deficiencies are extremely common today, affecting nearly 2–3 out of every 5 individuals. These vitamins are essential for bone health, nerve function, brain health, heart function, and overall metabolism.
Because the liver stores these vitamins, the body can continue to function efficiently even when daily dietary intake is inconsistent. This storage capacity protects the body from sudden deficiencies.
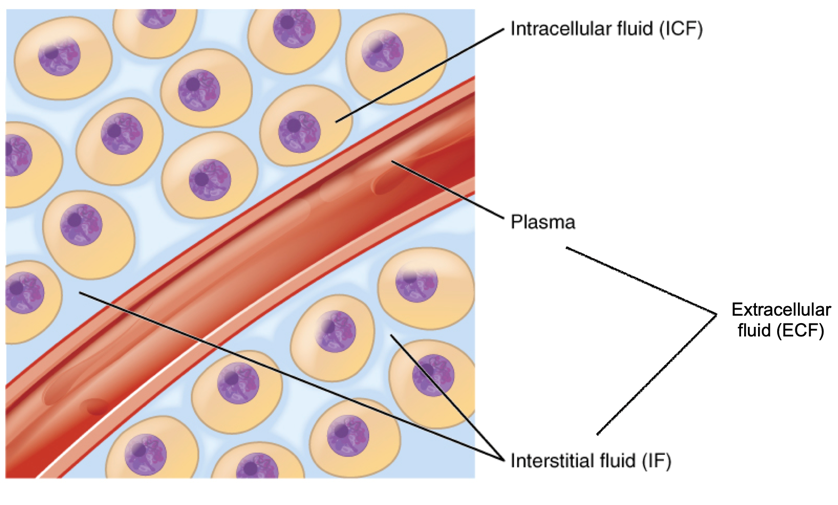
Mineral Storage and Electrolyte Balance
In addition to vitamins, the liver also stores and regulates minerals, which are vital for:
- Maintaining electrolyte balance
- Supporting bone strength
- Preventing dehydration
- Ensuring proper muscle and nerve function
Adequate mineral balance helps the body remain strong, hydrated, and metabolically stable.
Synthesis of Plasma Proteins and Lipids
Another critical function of the liver is the synthesis of plasma proteins, including:
- Cholesterol
- Triglycerides
- Lipoproteins
These substances are essential for cellular structure, hormone production, and energy transport. However, imbalance in their synthesis can lead to lifestyle diseases, such as:
- High cholesterol
- Plaque formation in arteries
- Partial or complete arterial blockages
Proper liver function ensures balanced synthesis and regulation of these substances, thereby reducing the risk of cardiovascular disorders.
Liver-Centered Approach to Treating Diseases
When treating any disease, the first and most important target should always be the liver. From a holistic and naturopathy point of view, the liver is considered the “giver”—the giver of vitality, balance, and internal cleansing. If the liver functions properly, the entire body begins to heal naturally.
Importance of Liver Detoxification
The primary goal in disease management is detoxification of the liver. According to naturopathy, the most effective, fastest, and result-oriented therapy for liver detoxification is fasting.
Fasting: The Best Natural Therapy for Liver Detox
From the naturopathy perspective, fasting is the most powerful and curative therapy to cleanse the liver. It is:
- Natural
- Highly effective
- Cost-free
- Result-oriented
Fasting may range from one day to five days or even up to a week, depending on:
- Patient’s age
- Body capacity
- Health condition
- Metabolic strength
During fasting, the body shifts its energy from digestion to self-healing and detoxification. This allows the liver to cleanse itself rapidly and efficiently. In such cases:
- Expensive herbs
- Medicines
- Special diets
become secondary. When fasting is followed correctly, liver detoxification happens naturally, quickly, and accurately.
Liver Health and Overall Well-Being
These fundamental liver functions collectively support the entire body system. It is often said:
- If digestion is good, health is good
- If the stomach is clean, diseases stay away
Proper digestion, metabolism, enzyme secretion, blood glucose regulation, and vitamin balance are all dependent on a healthy liver. Without proper liver function, maintaining health becomes nearly impossible.
Seasonal Detoxification: A Preventive Approach
For maintaining long-term health, regular detoxification is essential, especially during seasonal changes. Ideally:
- Every 3 months (90 days)
- Detoxification should be done for 3–5 days
This practice helps reset metabolism, improve digestion, strengthen gut health, and support enzyme and hormone balance. Regardless of the method used, detoxification is necessary for preventive health care.
Liver and Metabolism
When metabolism slows down:
- Digestion becomes weak
- Gut health deteriorates
- Enzyme activity reduces
- Blood glucose regulation becomes imbalanced
- Vitamin and mineral utilization declines
Without proper liver function, even eating food becomes ineffective. Therefore, to treat the root cause of any disease or deficiency, the liver must always be addressed first.
Weight of the Liver and Obesity Impact
In a healthy adult human:
- Liver weight ranges between 2 to 1.5 kg
- Slight variations exist between males and females
In an ideal body weight of 55–60 kg, the liver already carries a significant workload. When a person becomes overweight or obese, excessive fat accumulation increases the burden on the liver. This forces the liver to:
- Secrete more enzymes
- Produce more hormones
- Work harder to metabolize excess fat
Excess body fat negatively impacts liver health and overall metabolism, making obesity a major risk factor for liver disorders.
Common Liver Diseases
Liver health directly affects overall health. Below is a list of common liver diseases identified through scientific research and clinical observation:
- Cirrhosis of the liver
- Hepatitis B and Hepatitis C
- Human hepatitis
- Liver cancer
- Metabolic Dysfunction–Associated Fatty Liver Disease (MAFLD)
- Jaundice
- Hemochromatosis
- Portal hypertension
- Primary biliary cholangitis
- Schistosomiasis
- Hepatic encephalopathy
- Hepatorenal syndrome
- Intrahepatic cholestasis of pregnancy
- Alcoholic liver disease
- Alpha-1 antitrypsin deficiency
- Budd–Chiari syndrome
- Gilbert syndrome
This list highlights how liver dysfunction can manifest in multiple systemic disorders, reinforcing the importance of early liver care and preventive detoxification.
Rare and Common Liver Diseases: Understanding What Matters Most
There are several liver-related conditions such as hepatic encephalopathy, Wilson’s disease, and acute hepatic disorders. While it is important for medical and health students to be familiar with these names, many of these conditions are rare, especially from an Asian population perspective. Diseases like Gilbert’s syndrome and Wilson’s disease are uncommon and are not frequently encountered in routine clinical practice.
From a public health and treatment point of view, the primary focus should be on common liver disorders. When common diseases are well understood, a larger population benefits, and early intervention becomes possible.

Most Common Liver Disorders
Among liver diseases, the most commonly encountered conditions in clinical practice include:
- Fatty liver disease
- Jaundice
- Alcoholic liver disease
These conditions are frequently seen during patient consultations and often represent the early stages of chronic liver disorders. Among them, fatty liver is considered the starting point for many long-term liver problems.
Fatty Liver Disease: The Beginning of Chronic Liver Disorders
Fatty liver disease is often detected incidentally during ultrasound or sonography. Many patients are diagnosed with Grade 1 fatty liver without experiencing any noticeable symptoms.
A Grade 1 fatty liver indicates:
- Disturbed liver function
- Excess fat deposition in the liver
- Impaired fat metabolism
In most cases, patients are unaware of the condition until an imaging test is performed for an unrelated health issue. This makes fatty liver a silent but significant disorder.
Common Conditions Associated with Fatty Liver
Fatty liver disease is commonly associated with several metabolic and lifestyle-related conditions, including:
- Central obesity
- Dyslipidemia (abnormal lipid levels)
- Hypertension
- Insulin resistance
Central Obesity
Central obesity, or fat accumulation around the abdomen, is considered a major root cause of multiple diseases. Since the liver is responsible for metabolizing fats, carbohydrates, and proteins, any sudden or unexplained weight gain may indicate liver dysfunction.
For example, if a person experiences:
- Rapid weight gain within a short period
- Difficulty losing weight despite diet and exercise
Then liver-related investigations should be considered.
Dyslipidemia and Hypertension
Dyslipidemia often leads to lifestyle diseases such as hypertension. If blood pressure remains uncontrolled despite:
- Lifestyle modifications
- Pranayama and stress management
- Dietary changes
- Modern medications
Then underlying liver dysfunction should be evaluated, as improper lipid metabolism can contribute to persistent hypertension.
Insulin Resistance and Diabetes
Insulin resistance is closely linked to liver function. When glucose regulation is disturbed, it may indicate combined dysfunction of the liver and pancreas. This often leads to diabetes-related complications and metabolic imbalance.
Common Symptoms Suggestive of Fatty Liver
Although fatty liver is often asymptomatic, some individuals may experience subtle signs, including:
- Persistent weakness
- Lethargy
- Morning fatigue
- Generalized tiredness
- Mild pain or discomfort in the upper abdominal region
When these symptoms occur alongside conditions like obesity, high blood pressure, or insulin resistance, fatty liver disease should be suspected.
Treatment Approach: Focus on Liver Detoxification
Regardless of the specific liver disease—whether fatty liver, jaundice, or alcoholic liver disease—the core treatment approach remains the same:
- Target liver detoxification first
- Improve liver metabolism
- Support liver function through naturopathy and herbal therapies
While disease names may differ, the foundation of treatment lies in cleansing and strengthening the liver. Once detoxification is achieved, the body’s natural healing mechanisms begin to restore balance.
When to Screen for Liver Health
In today’s lifestyle, especially for individuals above 35 years of age or those who are on long-term medications, it is highly advisable to undergo regular liver screening. One of the most effective and easily accessible tests is an abdominal ultrasound, which clearly shows:
- Liver position
- Liver size
- Fat deposition (fatty liver grading)
Although several blood tests are available, ultrasound is often the first and most reliable indicator of fatty liver disease.
Early Symptoms Indicating Liver Dysfunction
Poor liver health can present with multiple subtle symptoms that are often ignored. These may include:
- Persistent lack of energy
- Mood fluctuations
- Disturbed or obstructed sleep
- Drowsiness and weakness
Energy in the body primarily comes from carbohydrates. If a person consumes adequate carbohydrates but still feels tired and low on energy, it indicates impaired carbohydrate metabolism, which is largely managed by the liver.
Liver Function, Hormones, and Mental Health
The liver plays a major role in the secretion and regulation of hormones and enzymes. When liver function is disturbed:
- Hormonal imbalance may occur
- Mood swings increase
- Confusion and restlessness may be experienced
- A person may feel mentally dull or uneasy
From a naturopathic perspective, aggravated internal imbalances—especially involving bile and air elements—can directly affect emotional stability and mental clarity.
Gut Health and Liver Connection
When digestion is disturbed and gut health deteriorates, bile secretion and absorption become irregular. This further worsens liver function, creating a vicious cycle. Therefore, maintaining proper liver function is essential for good gut health.
Disturbed Sleep as a Warning Sign
Sleep disturbances are another important indicator of liver dysfunction. If symptoms such as poor sleep, fatigue, or mood changes persist for more than 10 to 15 days, they should not be ignored. These are early warning signs, and timely medical consultation is essential.
Early diagnosis allows liver disorders to be treated effectively before they progress into chronic diseases.

Importance of Listening to the Body
The human body is highly intelligent and continuously sends signals. By observing:
- Daily energy levels
- Mood changes
- Eating patterns
- Digestion
- Physical movement
One can detect abnormalities at an early stage. Early intervention makes liver treatment easier and prevents long-term damage.
Pain and Discomfort in Liver Region
One of the most specific signs of liver involvement is pain or discomfort in the upper right side of the abdomen, which corresponds to the anatomical location of the liver.
Advanced Signs of Liver Dysfunction
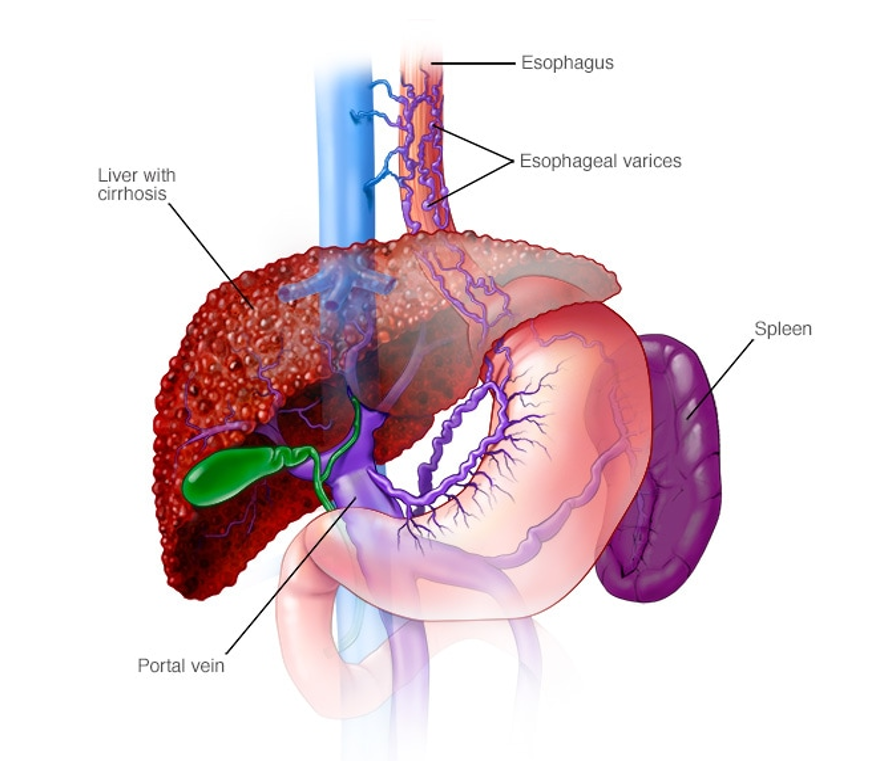
As liver disease progresses, more serious signs may appear, including:
- Abdominal swelling due to fluid accumulation (ascites)
- Enlarged blood vessels
- Enlarged spleen (splenomegaly)
These conditions often develop due to Non-Alcoholic Steatohepatitis (NASH), an advanced form of fatty liver disease.
Relationship Between Liver and Spleen
The liver and spleen are closely connected in their function. If the liver enlarges or becomes dysfunctional:
- The workload on the spleen increases
- Blood flow dynamics change
- Spleen enlargement may occur
Both organs lie on opposite sides of the abdomen but function in coordination. Disturbed bile secretion and increased internal pressure can affect not only the liver but also the spleen and nervous system.
Non-Alcoholic Steatohepatitis (NASH)
NASH (Non-Alcoholic Steatohepatitis) is a progressive form of non-alcoholic fatty liver disease where:
- Inflammation develops in the liver
- Liver cells are damaged
- Fibrosis may begin
If untreated, NASH can progress to cirrhosis and liver failure.
Non-Alcoholic vs Alcoholic Liver Disease
Liver diseases are broadly classified into alcoholic and non-alcoholic conditions. Alcoholic liver disease occurs due to excessive consumption of alcohol. However, many people who do not consume alcohol are often surprised when they are diagnosed with liver disorders such as fatty liver, liver disease, or liver cirrhosis.
A common question patients ask is:
“I am a non-alcoholic. I do not drink alcohol. Why do I have a liver problem?”
The answer lies in Non-Alcoholic Steatohepatitis (NASH), a condition where liver damage occurs without alcohol consumption. In fact, people who consume alcohol are at a higher risk, but non-alcoholic individuals can still develop serious liver diseases due to metabolic and lifestyle factors.
Portal Hypertension and Enlarged Blood Vessels
In advanced liver conditions such as NASH, portal hypertension develops. This means there is an increase in pressure within the portal vein, which carries blood to the liver.
Due to increased pressure:
- Blood vessels enlarge
- Thin-walled veins develop (especially where nerve support is absent)
- Blood flow becomes congested and sluggish
These changes lead to multiple internal and external complications.
Progression of Liver Disease Symptoms
In the early stages, symptoms may be mild and often ignored. However, if these warning signs are not addressed, liver disease starts to manifest externally.
External Visible Signs of Liver Disease
As the condition progresses, visible changes appear on the body, including:
- Red palms (Palmar erythema) – excessive redness of the palms
- Yellow discoloration of the eyes – a classic sign of jaundice
- Changes in skin texture and color
Persistent jaundice and visible skin changes indicate worsening liver function.
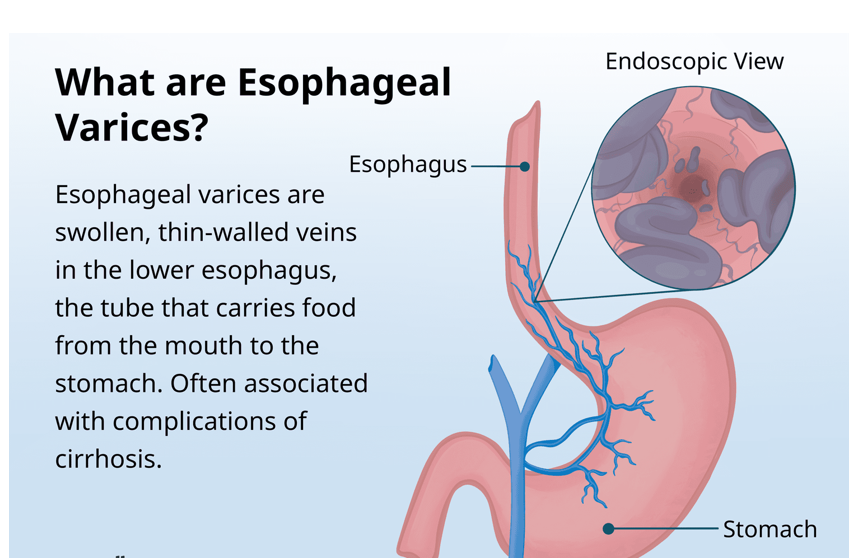
Esophageal Varices and Life-Threatening Bleeding
One of the serious complications of advanced liver disease is the development of esophageal varices.
The esophagus, or food pipe, develops swollen veins due to increased portal pressure. These veins can:
- Become fragile
- Rupture easily
- Cause severe internal bleeding
Initially, mild blood may appear during coughing or throat infections. However, continuous bleeding from the mouth, especially during spitting or vomiting, indicates rupture of esophageal veins and is a medical emergency.
Hepatic Encephalopathy: Liver–Brain Connection
Another critical complication of liver failure is hepatic encephalopathy, which occurs due to the accumulation of ammonia and other toxins in the blood.
Symptoms of Hepatic Encephalopathy
As ammonia levels rise:
- Confusion begins
- Drowsiness increases
- Speech becomes unclear
- Consciousness may be altered
This condition highlights the direct connection between the liver and the brain. When the liver fails to detoxify ammonia effectively, toxins reach the brain, affecting:
- Brain cells
- Neural pathways
- Cognitive and motor functions
The collective symptoms of confusion, altered speech, and drowsiness are clinically termed hepatic encephalopathy.
Advanced Complications of Liver Disease
If liver disease is not detected and treated in time, it can progress to:
- Liver cirrhosis
- Liver cancer
These represent the final and most dangerous stages of liver damage.
Non-Alcoholic Fatty Liver Disease: Causes, Stages, Symptoms, and Life-Threatening Complications
Many people believe that liver disease occurs only in those who consume alcohol. However, a large number of patients suffering from liver problems are non-alcoholic. When such individuals are diagnosed with fatty liver, cirrhosis, or liver disease, the first question that arises in their mind is: “I don’t drink alcohol—why did this happen to me?”
This condition is known as Non-Alcoholic Fatty Liver Disease (NAFLD). Although alcohol consumption can cause liver damage, non-alcoholic individuals can also develop serious liver disorders due to lifestyle factors, metabolic issues, and long-term neglect of early symptoms.
What Is Fatty Liver?
Fatty liver occurs when an abnormal amount of fat accumulates in the liver cells. This excessive fat deposition in liver tissues is medically known as steatosis.
The liver cells have a limited capacity to store fat. When fat exceeds this capacity, it begins to damage liver cells, disturb liver function, and gradually impair the liver’s ability to detoxify the body.
Early Changes and Internal Warning Signs
In the early stages, liver disease may not cause noticeable pain. However, several internal changes begin silently. One important change is portal hypertension, where pressure increases in the portal vein system. This leads to enlargement of blood vessels beneath the skin, although these vessels do not contain nerves.
As a result, bloating and discomfort may begin, and multiple symptoms can slowly appear. These early signs act as warning indicators of liver disease, whether it is fatty liver or another chronic liver condition.
External Signs of Liver Disease
When liver problems are ignored, symptoms begin to appear externally and become visually noticeable. Common signs include:
- Red palms, medically called palmar erythema, where the palms become extremely red
- Yellowing of the eyes, a common sign of jaundice
- Changes in skin appearance, especially on the upper body
These visible signs indicate that the liver is no longer functioning optimally.
Serious Complications of Untreated Liver Disease
If liver disease continues without treatment, it can lead to severe and life-threatening complications.
Esophageal Varices
Increased pressure in liver circulation causes swollen veins in the esophagus (food pipe). These veins can rupture suddenly, leading to internal bleeding, which is a medical emergency.
Sometimes blood may appear during coughing. Occasional blood due to throat infection may not be serious, but repeated blood in spit or vomiting blood is a dangerous sign of ruptured veins.
Hepatic Encephalopathy
Another major complication is hepatic encephalopathy, caused by the accumulation of ammonia in the blood due to poor liver detoxification.
Symptoms include:
- Confusion
- Drowsiness
- Slurred or unclear speech
- Difficulty recognizing surroundings
This condition directly affects the brain, brain cells, and nerves, showing the strong connection between liver health and brain function.
Progression to Cirrhosis and Liver Cancer
When liver damage becomes long-standing and chronic, it may progress to:
- Liver cirrhosis (permanent scarring of the liver)
- Liver cancer
These conditions develop gradually over time if early symptoms are ignored.
End-Stage Liver Failure: A Life-Threatening Condition
Liver failure is the end stage of liver disease and is extremely life-threatening.
The progression typically follows this pattern:
- Fatty liver (reversible stage)
- Liver inflammation and damage
- Liver cirrhosis
- Liver failure
In the early stages, fatty liver can be easily reversed by removing excess fat and correcting lifestyle habits. However, ignoring bodily signals allows the disease to worsen over years.
Studies show that 5–12% of non-alcoholic fatty liver patients may progress to cirrhosis over time if left untreated.
Liver failure does not occur suddenly—it is the result of long-term neglect, improper treatment, genetic factors, or continued lifestyle mistakes.
Three Main Stages of Non-Alcoholic Liver Disease
- Non-Alcoholic Fatty Liver Disease (NAFLD)
Fat accumulation in the liver without inflammation or significant damage. At this stage, there may be no symptoms, and reversal is possible.
- Non-Alcoholic Steatohepatitis (NASH)
If fatty liver remains untreated, inflammation and liver cell damage begin. This stage is more serious and requires proper intervention.
- Liver Cirrhosis and Liver Failure
Permanent liver damage occurs, leading to loss of liver function and possible liver failure.
Impact on Other Organs
Liver failure not only affects the liver but is also associated with cardiovascular diseases. Poor liver health directly impacts heart function, increasing overall health risks.
Role of Naturopathy in Liver Health
With the help of naturopathy, it is possible to prevent and reverse liver damage at early stages. While complete reversal of cirrhosis is challenging, early intervention can significantly slow progression and improve quality of life.
The key lies in early detection, timely treatment, lifestyle correction, and listening to the body’s warning signs.
Management, Diagnosis, and Naturopathic Approach to Non-Alcoholic Fatty Liver Disease
Reversibility and Prevention in Liver Disease
In the initial stages of fatty liver, the condition can be easily reversed with proper naturopathic treatment, appropriate therapies, and a well-planned diet. Early intervention plays a crucial role in restoring liver health.
However, once the disease progresses beyond a certain stage, complete reversal may not be possible. Even then, effective management can prevent further progression, especially at the stage of liver cirrhosis. With timely care, it is possible to stop the condition from advancing to liver failure, which causes permanent and life-threatening damage.
Managing advanced liver disease requires extreme care, patience, and consistency. It involves proper food combinations, long-term therapies, and individualized treatment plans. No single therapy or diet suits every patient. Each treatment approach must be customized according to the patient’s unique condition.
Importance of Individualized Treatment in Chronic Liver Conditions
Liver disease management cannot follow a generalized approach. Chronic patients often have associated health problems, allergies, or metabolic disorders. Additionally, male and female body structures differ, which further influences treatment planning.
According to traditional health principles, individuals differ in their Prakriti (body constitution) and Dosha balance—Vata, Pitta, and Kapha. Diet, daily routine, and therapy must be designed based on these factors.
Therefore, while treating chronic liver disease, multiple aspects must be taken into consideration:
- Body constitution
- Existing medical conditions
- Allergies and sensitivities
- Digestive strength and metabolism
- Lifestyle and stress levels
Such a personalized approach is essential, especially once the disease enters the chronic stage.
Diagnosis of Liver Disease
Role of Symptoms and Physical Signs
Although physical signs and symptoms provide important clues, they are not 100% reliable for diagnosis. Similar symptoms can occur in other diseases as well. Therefore, confirmatory investigations are necessary to reach an accurate diagnosis.
Blood Investigations for Liver Assessment
The first step in diagnosis should be blood investigations. These tests help detect liver dysfunction even before severe symptoms appear.
Liver Function Test (LFT)
LFT provides valuable information about liver health by assessing:
- Bilirubin levels
- Liver enzymes
- Albumin levels
These parameters help identify early liver damage and functional impairment.
Liver Enzymes
Tests such as SGPT and SGOT, along with bilirubin ratios, indicate the extent of liver cell injury and inflammation.
Complete Blood Count (CBC)
CBC is essential in almost all diseases. It helps assess:
- Hemoglobin levels
- White blood cell count
- Platelets
- Overall immune status
ESR levels further indicate ongoing inflammation in the body.
Hepatitis Screening
Blood tests for Hepatitis B and Hepatitis C are necessary to rule out viral causes of liver damage.
Protein and Globulin Levels
Evaluating protein and globulin levels helps understand liver synthesis capacity and nutritional status.
Metabolic and Associated Tests
Blood Sugar Tests
- Fasting Blood Sugar
- HbA1c (average blood sugar over 3 months)
These tests help assess glucose regulation. Liver health and diabetes are closely interconnected, and abnormal blood sugar levels can worsen liver disease.
Lipid Profile
Lipid profile evaluates:
- Triglycerides
- HDL
- LDL
Since fatty liver is directly related to fat metabolism, this test plays a crucial role in diagnosis and monitoring.
Imaging Studies
Ultrasound of the Abdomen
Ultrasound is a useful imaging procedure that provides a clear picture of liver size, fat accumulation, and structural changes. It helps confirm fatty liver and assess disease severity.
Holistic Approach to Liver Care
A combination of early diagnosis, personalized naturopathic treatment, dietary correction, and lifestyle management can significantly improve liver health. While early stages are reversible, even advanced stages can be managed effectively to prevent complications and improve quality of life.
Diagnostic Imaging and Treatment Approach in Fatty Liver Disease
Role of Imaging in Fatty Liver Diagnosis
When a patient is suspected of having fatty liver, the first and most commonly used investigation is an ultrasound. Ultrasound imaging helps clearly identify:
- Fatty liver
- Grade 1 and Grade 2 fatty liver changes
These grades are easily visible through ultrasound and help confirm the presence of fat deposition in the liver.
However, when there is a confirmed diagnosis of liver disease—such as fatty liver, steatohepatitis, or other chronic liver conditions—it becomes important to assess how much the liver size, shape, and internal structure are affected. In such cases, more advanced imaging techniques are required.
Advanced Imaging Techniques
CT Scan and MRI
A CT scan or MRI is advised when there is a need for a more detailed assessment of liver damage. These imaging techniques help evaluate:
- Structural changes in the liver
- Alterations in liver size and shape
- Extent of internal damage
They are especially useful when ultrasound findings are inconclusive or when disease progression is suspected.
Assessment of Liver Stiffness and Fibrosis

To assess the stiffness of liver tissue and the degree of fat accumulation, a test known as Transient Elastography is commonly used. This test helps determine:
- Fat content in liver tissues
- Degree of fibrosis (hardening of liver tissue)
Different techniques of elastography may be used depending on whether the condition is:
- NAFLD (Non-Alcoholic Fatty Liver Disease)
- NASH (Non-Alcoholic Steatohepatitis)
These tests are performed by trained technicians, and clinicians can suggest them based on the patient’s condition.
MR Elastography
MR Elastography is an advanced imaging procedure that combines MRI technology with elastography. It provides:
- Highly accurate assessment of liver tissue stiffness
- Detailed visualization of fibrosis and inflammation
This test is recommended when:
- Diagnosis is unclear
- Disease severity is difficult to assess
- Doctors feel that standard tests are not capturing the complete picture
Liver Biopsy
When there is strong suspicion of liver cancer or advanced disease, or when imaging results remain inconclusive, a liver biopsy may be advised.
In this procedure:
- A small tissue sample is taken from the liver
- The sample is examined under a microscope
- It helps confirm conditions like advanced fibrosis, cirrhosis, or cancer
Liver biopsy is usually reserved for specific cases and is not required for every patient.
Modern Medical Perspective on Fatty Liver Disease
According to modern medicine, fatty liver disease is often associated with:
- Obesity
- Insulin resistance
- Metabolic syndrome
These conditions significantly increase the risk of cardiovascular diseases as well.
Doctors do not prescribe a single universal medicine for fatty liver. Treatment is always individualized, depending on the underlying cause. This principle is also helpful for naturopaths, who focus on correcting root causes rather than prescribing medications.
Treatment Strategy Based on Underlying Cause
Fatty Liver Associated with Obesity
If fatty liver is primarily due to obesity, the main treatment goal is:
- Weight reduction
- Improving overall body composition
In such cases, fatty liver can often be completely reversed through weight management alone, without the need for medications. Once body weight normalizes, the liver can return to its healthy state.
Fatty Liver Associated with Insulin Resistance
When fatty liver is linked to insulin resistance or diabetes, treatment focuses on:
- Controlling insulin levels
- Maintaining stable blood sugar levels
Proper glycemic control helps prevent further liver damage and supports liver recovery.
Fatty Liver and Metabolic Syndrome
If fatty liver is part of metabolic syndrome, the primary focus is on:
- Improving metabolic health
- Regulating lipid levels
- Preventing progression to diabetes
Metabolic syndrome can worsen liver disease and also lead to diabetes if not addressed in time.
Understanding the Liver: Its Functions, Diseases, and Natural Management
The liver is one of the most vital organs in the human body, often referred to as a powerhouse and storage center. It plays a central role in metabolizing fats, carbohydrates, and proteins, ensuring that the body can absorb essential nutrients efficiently. The liver also regulates enzymes and hormones, maintains homeostasis, and stores critical vitamins such as A, D, E, K, B12, and minerals, which are essential for overall health.
Liver Functions and Importance
Digestion begins in the mouth with saliva, which is highly alkaline and the first step in the digestive process. However, proper enzyme activation throughout the digestive tract, supported by the liver, is critical for nutrient absorption. If the liver does not function optimally, even a nutritious diet may fail to provide health benefits.
The liver is responsible for regulating blood glucose, which is why diabetes is often considered a metabolic disorder linked to liver dysfunction. Maintaining a healthy liver ensures proper hemoglobin A1c levels, indicating effective blood sugar regulation. Additionally, the liver synthesizes plasma proteins, cholesterol, triglycerides, and lipoproteins. Its storage capacity prevents deficiencies in essential vitamins and minerals, supports clotting via vitamin K, and maintains electrolyte balance, which is crucial for hydration and overall strength.
Detoxification and Liver Health
From a naturopathy perspective, detoxification is essential for maintaining liver health. Fasting is considered the most effective, active, and result-oriented therapy to cleanse the liver. Depending on the patient’s age, health, and capacity, fasting for one to five days can significantly improve liver function without the need for expensive herbs or medications. Regular detoxification every three months is recommended to maintain metabolism, digestion, and overall wellness.
Liver Diseases: Common and Rare
Liver diseases range from common conditions such as fatty liver, jaundice, and alcoholic liver disease to rarer conditions like Wilson’s disease, Gilbert’s syndrome, and hepatic encephalopathy. While rare conditions are important to know, focusing on the common diseases provides the most practical benefit for treatment.
Fatty Liver and Non-Alcoholic Fatty Liver Disease (NAFLD): Often asymptomatic in the initial stages, fatty liver can be detected via ultrasound. It is frequently associated with central obesity, dyslipidemia, hypertension, and insulin resistance. If untreated, fatty liver can progress to non-alcoholic steatohepatitis (NASH), liver cirrhosis, and eventually liver failure.
Alcoholic Liver Disease: Excessive alcohol consumption can lead to liver damage, cirrhosis, and failure. Portal hypertension may cause enlarged blood vessels and other complications, such as esophageal varices, which can be life-threatening.
Hepatic Encephalopathy: Accumulation of ammonia due to liver dysfunction can impair brain function, causing confusion, drowsiness, and in severe cases, permanent neurological damage.
Symptoms and Early Detection
Early detection is crucial in preventing chronic liver damage. Key symptoms to monitor include fatigue, weakness, disturbed sleep, mood fluctuations, abdominal discomfort (particularly in the upper right side), red palms (palmar erythema), and yellowing of the eyes (jaundice). These symptoms indicate potential liver dysfunction and should prompt immediate consultation with a healthcare professional.
Diagnostic Approach
Accurate diagnosis requires a combination of physical examination, blood tests, and imaging studies:
- Blood Tests: Liver function tests (bilirubin, albumin), complete blood count (CBC), electrolytes, hepatitis B and C markers, liver enzyme tests (SGPT, SGOT), fasting blood sugar, haemoglobin A1c, and lipid profile.
- Imaging: Ultrasound for fatty liver grading, CT scan or MRI for assessing liver size, shape, and tissue integrity, transient elastography, and MR elastography for detailed evaluation.
- Liver Biopsy: Reserved for suspected cancer or advanced disease.
Treatment of liver disease, particularly fatty liver, requires a multi-faceted approach:
- Weight Management: Obesity is a primary contributor to fatty liver. Controlling body weight can often reverse early-stage fatty liver.
- Blood Sugar and Insulin Control: For patients with insulin resistance or diabetes, regulating glucose levels is critical to protect liver health.
- Cardiovascular Health: In cases associated with hypertension or metabolic syndrome, monitoring cholesterol, triglycerides, and HDL is necessary.
- Customized Diet: Dietary changes are essential. Nutrient-dense, antioxidant-rich foods help reduce fat accumulation, correct deficiencies, and support overall metabolism.
- Lifestyle Modifications: Consistent sleep, rest, exercise, behavioral adjustments, and even considerations like clothing choices under extreme temperatures contribute to liver health.
- Naturopathy and Alternative Therapies: Fasting, herbal therapies, and other naturopathic interventions can support liver detoxification and regeneration. Each treatment must be personalized, taking into account allergies, gender, age, and individual constitution (doshas).
Preventing Complications
Early intervention can prevent the progression from fatty liver to cirrhosis and liver failure. At initial stages, naturopathy and lifestyle adjustments can reverse fatty liver. Even in later stages, while reversal may not be possible, proper care can prevent progression to permanent damage. Chronic liver diseases also affect cardiovascular health and overall metabolism, highlighting the importance of holistic treatment.
Lifestyle and Dietary Measures to Support Liver Health
Maintaining a healthy liver requires a combination of dietary changes, physical activity, and behavioral modifications. Antioxidants play a key role in naturally detoxifying the liver, and the best sources of antioxidants are fresh fruits and vegetables. By integrating more of these nutrient-rich foods into your daily diet, you can support liver function and reduce fat accumulation. Remarkably, positive changes in diet can produce noticeable improvements in just three to four days, as the body begins to respond and symptoms start to subside.
Exercise: A Free and Effective Tool
Regular exercise is essential for liver health and overall well-being. Exercise stimulates metabolism, improves insulin sensitivity, and supports fat reduction. It can take many forms—walking, yoga, pranayama, aquatic exercises, or other forms of physical activity—tailored to your age, body type, and lifestyle.
While morning exercise is traditionally recommended, it is not mandatory. What matters most is consistency. For those unable to exercise in the morning due to work schedules or other commitments, evening exercise—at least four to five hours after lunch—is equally effective. The key is to maintain an empty stomach during exercise to maximize its benefits.
Behavioral and Mental Well-being
Behavioral modification plays a crucial role in liver health. Maintaining calmness, reducing anxiety, and promoting relaxation positively influence the gut-liver-brain axis. Practices such as deep breathing, yoga, and mindfulness can enhance digestion, normalize bile secretion, and shift the body toward an alkaline state, which is essential for optimal cellular and hormonal function.
Adopting a “let-go” attitude, patience, and positivity is equally important. This mindset supports recovery, reduces stress-related liver strain, and enhances the effectiveness of dietary and lifestyle interventions.
Improving Insulin Sensitivity
Insulin resistance is directly linked to fatty liver. Improving insulin sensitivity through diet, exercise, and lifestyle modifications helps reduce liver fat and prevents disease progression. This approach is universally recommended across medical systems, including allopathy, naturopathy, Ayurveda, and homeopathy.
Key Dietary Recommendations
- Avoid Refined Carbohydrates: The liver’s primary function includes carbohydrate metabolism. Excess refined carbohydrates burden the liver, contributing to fat accumulation and metabolic stress. Minimizing foods such as white bread, pastries, sugary drinks, and processed snacks is critical.
- Increase Nutrient-Dense Foods: Include fresh fruits, vegetables, and foods rich in antioxidants to support detoxification and repair.
- Balanced Diet: Focus on adequate protein, healthy fats, and fiber to maintain stable blood sugar, support digestion, and improve liver enzyme function.
By combining dietary improvements, regular exercise, behavioral modifications, and stress management, liver health can be effectively preserved and even restored. Early and consistent attention to these factors helps prevent progression to serious conditions such as non-alcoholic steatohepatitis (NASH), cirrhosis, and liver failure.
Foods to Avoid and Nutrient-Dense Choices for Liver Health
When managing liver health, it is crucial to eliminate certain foods that place excessive burden on the liver. These include:
Foods to Avoid
- Refined Sugars and Sweets:
Ready-made sugar products such as candies, biscuits, pastries, and plain flour (maida) should be completely avoided. These foods overload the liver and disrupt metabolism. Soda, aerated drinks, ice creams, and similar sweetened beverages should also be eliminated. - Fried and Processed Foods:
Foods like French fries, packaged snacks, sausages, mayonnaise, and other ready-to-eat items are highly processed and detrimental to liver health. Even though convenient, these products are often high in harmful fats, additives, and preservatives, making them toxic for the liver. - High Saturated Fat Foods:
Foods rich in saturated fats, combined with refined carbohydrates, increase liver stress and contribute to fatty liver and other metabolic issues. - Commercially Processed Dry Fruits:
While dry fruits are generally healthy, commercially roasted and salted varieties should be avoided. Plain, unprocessed dry fruits are acceptable in moderation.
The principle is simple: the less processed the food, the better it is for your liver. Whenever possible, prepare meals at home with fresh ingredients and hygienic cooking methods. Even deep-fried foods prepared at home are easier to digest and healthier than commercially processed options. Using fresh oil only once and cooking in controlled conditions significantly reduces harmful compounds and cancer risks associated with reused oil.
Nutrient-Dense Foods to Include
- Fruits and Vegetables:
Incorporate at least one fruit and a variety of vegetables daily. These provide antioxidants that naturally detoxify the liver. - Nuts and Seeds:
Include at least three different types of nuts and one type of seed in your routine. These nutrient-dense foods support liver function, metabolism, and overall health. - Homemade, Freshly Cooked Meals:
Preparing meals at home ensures freshness, hygiene, and controlled use of oil and spices. Homemade versions of popular foods like aloo tikki, nuggets, or fritters are preferable to ready-made processed alternatives.
Weight Management and Liver Health
Weight loss is a central strategy for managing fatty liver, particularly for those who are overweight, obese, or super obese. Shedding even 10–15 kg can lead to visible and measurable improvements in liver function, gut health, mood, behavior, and overall confidence. Positive changes in body composition reinforce healthy lifestyle choices and help maintain long-term liver wellness.
Takeaway
Avoid refined carbohydrates, sugars, fried foods, and processed products. Emphasize fresh, nutrient-dense foods, homemade meals, and consistent weight management. By making these dietary changes, you can support liver function, reverse fatty liver at early stages, and improve overall health and vitality.
Antioxidant-Rich Foods and Herbs for Liver Health
Incorporating antioxidant-rich foods into your daily diet is essential for liver health, disease prevention, and overall wellness. Seasonal, regional, and naturally grown fruits and vegetables are the most effective sources of antioxidants, vitamins, and minerals for your body.
Seasonal and Regional Fruits
Fruits grown locally and in-season provide the best nutritional support. Red fruits, such as berries, cherries, plums, and peaches, are particularly rich in antioxidants and should be included regularly in your diet. While exotic fruits like dragon fruit, kiwi, and avocado can be consumed occasionally, they should not replace locally grown fruits. Using regional produce not only benefits your health but also supports local farmers and sustainable agriculture.
Vegetables and Nuts
Certain vegetables and nuts have exceptional therapeutic properties:
- Bitter Gourd (Bitter Melon): Known for its liver-supportive properties, bitter gourd is excellent for managing fatty liver and promoting detoxification.
- Garlic: A staple in Asian cuisine, garlic supports liver function and aids in reducing inflammation. Incorporate garlic in cooking or as a part of traditional chutneys.
- Broccoli: Rich in antioxidants, minerals, and proteins, broccoli helps in detoxifying the liver and supporting overall metabolic health.
- Walnuts: High in essential fatty acids and antioxidants, walnuts contribute to liver protection and cardiovascular health.
Consuming these foods as part of your regular diet helps prevent liver disorders and can support the reversal of early-stage liver disease.
Traditional Herbs for Liver Health
Several herbs are particularly effective in managing liver disease and supporting liver function:
- Punarnava: Known for its ability to rejuvenate cells, Punarnava is effective in reducing water retention, swelling, and liver-related pain.
- Tinospora (Giloy): A powerful immune booster, Giloy supports liver detoxification and enhances overall immunity.
Incorporating these herbs into treatment plans, along with a balanced diet of antioxidant-rich foods, provides natural support for liver health, aids in managing liver disorders, and can help in the prevention and reversal of liver-related conditions.
Herbs, Spices, and Yoga for Liver Health and Detoxification
Maintaining liver health involves not only diet and lifestyle but also the use of traditional herbs, spices, and therapeutic practices like yoga. Many of these approaches have been used for centuries in Indian tradition and are now supported by modern research for their beneficial effects on liver function, detoxification, and overall wellness.
Traditional Herbs and Spices
- Turmeric (Haldi):
Turmeric is a golden spice widely used in Indian cuisine and cultural rituals. Its active compound, curcumin, has been extensively studied for its anti-inflammatory, antioxidant, and anti-cancer properties. Turmeric supports liver detoxification, purifies the blood, and protects liver cells from damage. - Amla (Indian Gooseberry):
Amla is rich in vitamin C and antioxidants. It helps balance the doshas, supports liver detoxification, and strengthens overall immunity. Traditional practices include consuming fresh amla or incorporating it into herbal preparations. - Tulsi (Basil):
Tulsi is a potent herb with antibacterial, antifungal, and antioxidant properties. Consuming fresh tulsi leaves or decoctions in the morning can help protect liver cells, improve immunity, and support detoxification. - Wheatgrass:
Wheatgrass contains 16 essential nutrients and has a pH level similar to the human body, making it an excellent supplement for detoxification and liver support. It can be consumed fresh or as powder/tablets. - Aloe Vera:
Aloe vera supports gut health, aids digestion, purifies the blood, and helps remove toxins from deep tissues. It is widely used beyond the beauty industry and is a powerful natural aid for liver health. - Tinospora (Giloy):
Tinospora is an immune-boosting herb that supports liver detoxification and overall health.
Using a combination of these herbs—such as wheatgrass, tulsi, aloe vera, and tinospora—can produce noticeable improvements in liver function and overall health within a few days. Fresh forms are preferred, but high-quality dried herbs and tablets are also effective. Organic sources, such as those cultivated by Saffron4Health, ensure quality and purity.
Yoga for Liver Support
Yoga can enhance liver function, aid detoxification, and reduce stress levels. Certain asanas (postures) are particularly beneficial for chronic patients:
- Paschimottanasana (Seated Forward Bend)
- Ek Pada Pavan Muktasana (Single Leg Wind-Relieving Pose)
- Ardha Matsyendrasana (Half Spinal Twist)
- Savasana (Corpse Pose) – essential for relaxation and stress reduction
These postures, when practiced under the guidance of a qualified yoga trainer, help improve circulation, stimulate internal organs, and support the body’s natural detoxification processes. Proper alignment and breathing techniques are critical, especially for chronic patients.
Integrating Herbs and Yoga
Combining a diet rich in antioxidant-packed herbs with yoga practices creates a holistic approach to liver health. This approach supports detoxification, protects liver cells, balances the doshas, and improves overall well-being. Regular practice and consistency are key to achieving noticeable results, with improvements visible within a few days when combined with proper lifestyle and dietary adjustments.

Naturopathy Therapies and Fasting for Liver Health
For beginners, practicing advanced yoga postures such as Ekpadasana, Pavan Muktasana, and Ardha Matsyendrasana may be challenging due to limited body flexibility and strength. These asanas require not only elasticity but also the ability to hold specific positions. Performing them correctly often requires guidance from a qualified yoga trainer to prevent injury and maximize therapeutic benefits.
Detoxification and Fasting
Detoxification is a cornerstone of naturopathy, particularly for liver health. Fasting is one of the most effective therapies for cleansing the liver and supporting overall detoxification. Several fasting techniques can be tailored to a patient’s capacity and health condition:
- Complete Fasting: Abstaining from all food for one to two consecutive days.
- Liquid Fasting: Consuming only one type of liquid (such as fruit juice or herbal decoctions) for a day.
- Mono Diet: Eating a single type of food once a day, with water allowed between meals.
These fasting methods can help reduce liver load, improve metabolic functions, and support detoxification. Patients with high blood sugar or other chronic conditions should follow these fasting protocols under guidance.
Internal Cleansing Therapies
- Enemas: Warm water enemas are highly effective for intestinal cleansing. Three consecutive sessions are often sufficient for initial detoxification.
- Steam Baths: Steam baths help remove toxins through the skin. A duration of five to ten minutes is recommended. For patients with cardiovascular issues or hypertension, it is essential to cover the head and chest with wet, cold napkins during the session to prevent complications.
- Gastrohepatic Packs: These are therapeutic hot and cold packs applied to the abdomen and back. A typical session involves placing a hot water bag on the back and a cold pack on the abdomen for about 20 minutes. For patients with renal complications, the placement can be reversed. This therapy supports liver function and improves circulation.
- Tub Bath Therapy: Alternating between hot and cold water in the lower abdomen for 10 minutes each is another effective method. Always perform this on an empty stomach for maximum benefit.
Sunlight, Pranayama, and Natural Healing
Exposure to natural sunlight not only aids detoxification but also provides vitamin D, which is complementary to liver health and overall wellness. Performing yoga, pranayama, and exercises outdoors in natural light enhances the effects of these therapies. The body, composed of Panchamahabhuta (the five elements), responds positively to natural therapies and sunlight, supporting holistic healing.
Practical Tips for Liver Health: Herbs, Gastrohepatic Packs, and Exercise
For patients managing liver disease, incorporating natural therapies, herbal remedies, and lifestyle adjustments can greatly support liver function and overall health.
Optimal Environment for Exercise
If you have access to a terrace or balcony, it is ideal to perform exercises in open-air spaces to ensure proper ventilation. In high-rise apartments or urban areas such as Mumbai, avoid exercising under air conditioning. Instead, open windows and curtains to allow fresh air circulation, which enhances the effectiveness of physical activity.
Hot and Cold Packs (Gastrohepatic Therapy)
Gastrohepatic packs are a simple yet effective naturopathy therapy for supporting liver function. They involve alternating hot and cold applications on the body:
- Hot Pack: Can be a traditional hot water bag, rubber bag filled with hot water, or an electric heating pad.
- Cold Pack: Gel or ice packs kept in the freezer.
Procedure:
- Place the patient in a lying position on a mat or bed.
- Apply the hot pack on the back and the cold pack on the abdomen for 20–30 minutes.
- For patients with renal disorders, reverse the placement—hot pack on the abdomen and cold pack on the back—to ensure proper organ support.
Daily practice of gastrohepatic packs on an empty stomach is highly recommended for detoxification and improving liver circulation.
Herbal Remedies for Liver Health
Herbs are an integral part of supporting liver function. Recommended combinations include Wheat Grass, Basil, Aloe Vera, and Tinospora (Giloy). Dosages for fresh ingredients are:
- Wheat Grass: 40 grams
- Aloe Vera: 3–4 inches of fresh gel
- Basil: 15–20 fresh leaves
- Giloy Juice: 100 ml
These ingredients can be blended, filtered, and consumed as a juice. If using dry powders, mix equal parts and consume with water or honey. Tablets should be taken according to the manufacturer’s recommended dosage.
Example for Grade One Fatty Liver:
- Wheat Grass Powder/Tablets: 1 tablespoon of powder twice daily, or 2 tablets twice daily.
- Detox Juice: 100 ml at night, approximately 30–40 minutes after dinner.
General Guidelines
- Follow fresh and seasonal herbs and vegetables wherever possible.
- Maintain a consistent routine for therapies, including exercise, yoga, and gastrohepatic packs.
- For beginners in yoga, guidance from a qualified yoga trainer is recommended to safely perform asanas such as Ekpadasana, Pavan Muktasana, and Ardha Matsyendrasana.
- Ensure proper ventilation and environmental conditions during exercises for safety and efficacy.
By combining these therapies—herbs, fasting, yoga, exercise, and gastrohepatic packs—patients can effectively support liver detoxification, improve liver function, and promote overall wellness.
Additional Guidance for Liver Health and Therapy Practices
Visual and Physical Assessment
Observing certain physical signs, such as the palm color, can provide insights into a patient’s general health. Healthy individuals with good hemoglobin levels typically have evenly colored palms. In contrast, dark red patches or uneven coloration may indicate underlying issues and require further assessment.
Safety Considerations for Hot and Cold Therapy
Hot and cold packs, also known as gastrohepatic packs, are safe and effective when applied correctly. However, care must be taken to avoid thermal shock, especially in individuals with preexisting conditions:
- Adjust the temperature according to the patient’s tolerance; never use extremely hot or cold packs.
- Patients with heart conditions, pacemakers, or other systemic illnesses should exercise caution and consult a healthcare provider before therapy.
- Proper placement is crucial: for liver issues, the hot pack is placed on the back and the cold pack on the abdomen; for renal conditions, this is reversed.
With proper precautions, this therapy can be highly effective for liver detoxification and improving organ function.

For students and practitioners, it is important to note that while live lectures provide extensive explanations, not all visual content may have accompanying text or written material. Study resources may include:
- Pointers and summaries of lecture content.
- Access to study materials and articles related to the topics discussed.
- Additional references for independent reading or research, as complete transcription of live sessions is often not feasible.
Institutes such as Saffron and Saffron Educational and Medical Foundation ensure that students receive comprehensive guidance, combining live teaching with supplementary resources to support learning.
Embracing Online Learning and Social Media Resources
In the modern era, online platforms provide a wealth of health-related knowledge. While not all instructors use social media extensively, students and practitioners can benefit from the vast amount of educational content available online, including detailed video lectures, research articles, and interactive discussions.
Commitment to Comprehensive Education
At Saffron Institute, a dedicated panel of 18 expert doctors work to deliver high-quality, informative sessions. The combination of live lectures, practical demonstrations, and study materials ensures that learners receive well-rounded training in naturopathy, liver health, and related therapies.
Advanced Insights into Naturopathy and Liver Health
Education and Knowledge Level
For students and practitioners, the course content is designed to provide a comprehensive understanding equivalent to nursing programs or early MBBS studies, particularly in the second and third years. The curriculum includes:
- Diagnostic systems relevant to naturopathy.
- Fundamental knowledge of anatomy and physiology.
- Functional understanding of organs, systems, and their interrelations.
This ensures that learners with prior medical or health-related education can quickly grasp the concepts. Participants are encouraged to share queries via email to help the instructors improve course delivery and content quality.
Leveraging Digital Tools
Modern tools such as ChatGPT can support learning by providing detailed explanations, downloadable PDFs, and step-by-step guidance on naturopathy treatments. While the course integrates digital support, it is designed to reinforce practical and experiential learning alongside online resources.
Alkaline Foods and Their Role
Alkaline foods play a significant role in liver health and overall well-being. Key points include:
- Proper diet can influence saliva pH and digestive balance.
- Foods like dry grapes, amla, and dry ginger can help maintain an alkaline environment in the body.
- Alkaline foods contribute to faster recovery in cases of liver dysfunction and improve general health.
- Alongside diet, factors like sound sleep and emotional well-being are essential to enhance natural healing and maintain healthy saliva levels.
The guiding principle remains: “Food is medicine.” Starting with the right nutrition can substantially improve liver function and overall wellness.
Access to Learning Resources
Students can access course content through multiple formats:
- Audible podcasts in Hindi, English, and Gujarati.
- Video lectures available on the institute’s YouTube channel.
- Written articles and study materials accompanying the lectures.
This multi-format approach ensures learners can access information in the format that suits them best, whether through listening, reading, or watching demonstrations.
Sharing Practical Experience
The course emphasizes practical experience gained over years of clinical practice. Knowledge shared includes:
- Effective use of supplements and natural remedies.
- Observations from long-term patient treatments in naturopathy.
- Integrating lifestyle guidance with herbal and dietary interventions for optimal results.
Students and participants are encouraged to share their experiences, fostering an interactive learning environment where real-world application of knowledge complements theoretical understanding.
Conclusion
The liver is one of the most vital organs of the human body and plays a central role in maintaining overall health and internal balance. As the largest internal organ and the body’s biggest chemical factory, it performs hundreds of essential functions every moment, many of which are critical for survival. From digestion and metabolism to detoxification and hormone regulation, the liver works silently and continuously to keep the body functioning smoothly. Because of its extensive responsibilities, the liver directly or indirectly influences almost every organ and system in the body.
A healthy liver ensures proper digestion by producing bile, which helps in the absorption of fats and fat-soluble vitamins. It regulates blood sugar levels by storing and releasing glucose as needed, maintains protein metabolism, and plays a key role in blood clotting by producing essential clotting factors. Additionally, the liver filters toxins, drugs, alcohol, and harmful chemicals from the blood, converting them into less harmful substances that can be safely eliminated from the body. This detoxifying function alone highlights why the liver is indispensable to life.
Liver diseases often develop slowly and silently. In the early stages, symptoms may be mild or completely absent, allowing damage to progress unnoticed. Factors such as unhealthy dietary habits, excessive intake of processed foods, alcohol consumption, sedentary lifestyle, chronic stress, infections, environmental toxins, and long-term medication use can gradually weaken liver function. When the liver is overloaded or damaged, the entire body begins to suffer, leading to fatigue, digestive disturbances, hormonal imbalance, reduced immunity, and metabolic disorders.
Understanding liver diseases is not limited to learning their names or clinical features; it also involves recognizing the lifestyle patterns that contribute to liver stress and damage. From a preventive and naturopathic perspective, liver health depends greatly on daily habits. Natural foods, adequate hydration, regular physical activity, proper sleep, and mental relaxation are essential in maintaining optimal liver function. Avoiding unnecessary chemicals, minimizing toxin exposure, and supporting the body’s natural detoxification processes can significantly reduce the risk of liver disorders.
One of the most remarkable qualities of the liver is its regenerative capacity. Even after significant injury, the liver has the ability to heal and regenerate if given proper care and support. This makes early awareness, timely intervention, and natural management especially important. When the root causes are addressed and healthy habits are restored, the liver can recover and resume its vital functions effectively.
In conclusion, the liver is not just an organ but the foundation of metabolic health and vitality. Protecting liver health means protecting the entire body. Through education, awareness, and natural lifestyle practices, liver diseases can be prevented, managed, and in many cases reversed. A healthy liver leads to a healthier body, clearer mind, stronger immunity, and improved quality of life, making liver care an essential aspect of holistic health and long-term well-being.