Respiratory System
Respiration: Understanding the Process that Fuels Life

Respiration is one of the most vital biological processes in the human body, responsible for providing our cells with the oxygen they need to generate energy and maintain bodily functions. In simpler terms, respiration is the process of inhaling oxygen and exhaling carbon dioxide, but it involves much more than just breathing. Let’s dive deeper into the concept and its types.
What is Respiration?
Respiration refers to the biochemical process through which organisms exchange gases with their environment. In humans, it is the mechanism by which oxygen from the air is brought into the body and transported to the cells, while carbon dioxide, a waste product of cellular metabolism, is expelled from the body.
The process of respiration is fundamental to sustaining life, as oxygen is essential for the production of adenosine triphosphate (ATP), the energy currency of cells. Without this energy, cells wouldn’t be able to perform their basic functions.
Types of Respiration:
There are two primary types of respiration:
- External Respiration: External respiration, often referred to as breathing, is the exchange of gases between the air in the lungs and the blood. It occurs in the alveoli, tiny air sacs in the lungs, where oxygen from the inhaled air diffuses into the bloodstream, and carbon dioxide diffuses out of the blood to be exhaled. This process ensures that the body constantly receives a fresh supply of oxygen while eliminating carbon dioxide.
- Internal Respiration: Internal respiration takes place at the cellular level, where gas exchange occurs between the blood and body tissues. Oxygen carried by the blood is delivered to cells, where it is used for metabolic processes that produce energy. In return, cells release carbon dioxide, a byproduct of metabolism, back into the bloodstream, which is then carried to the lungs to be expelled.
The Importance of Respiration:
Respiration is crucial for maintaining life because it:
- Supplies Oxygen to Cells: Oxygen is needed for the process of cellular respiration, which produces ATP, the energy molecule that powers cellular functions.
- Removes Carbon Dioxide: Carbon dioxide is a waste product of cellular metabolism. If it accumulates in the blood, it can lead to harmful conditions, so its removal is vital for maintaining the body’s pH balance.
- Supports Energy Production: Through the process of respiration, oxygen helps convert nutrients like glucose into ATP, which fuels activities ranging from muscle movement to nerve signal transmission.
Understanding the Respiratory System: The Track of Air Flow

The respiratory system plays a critical role in supplying oxygen to the body and removing carbon dioxide. It consists of a series of organs and structures that guide air into the lungs, where the exchange of gases takes place. The respiratory “track” refers to the path air follows from the outside environment into the lungs. Let’s break down the key components of this track and their functions.
1. Nasal Cavity: The nasal cavity is the first part of the respiratory system where air enters the body. It is lined with tiny hairs (cilia) and mucous membranes that filter, warm, and moisten the incoming air. This ensures that by the time the air reaches the lungs, it is clean and at an appropriate temperature. The nasal cavity also plays a role in detecting smells through olfactory receptors.
2. Pharynx: The pharynx, or throat, is a muscular tube that serves as a common passageway for both air and food. It connects the nasal cavity to the larynx and esophagus. The pharynx is divided into three parts: the nasopharynx (behind the nose), oropharynx (behind the mouth), and laryngopharynx (closest to the larynx). When we breathe, the pharynx directs air into the lower respiratory tract.
3. Larynx: Commonly known as the voice box, the larynx sits below the pharynx. Its primary role is to allow the passage of air while preventing food and liquids from entering the trachea (windpipe). The larynx contains the vocal cords, which vibrate as air passes through, producing sound for speech. The epiglottis, a small flap of tissue, covers the larynx during swallowing to ensure food goes into the esophagus instead of the respiratory tract.
4. Trachea: The trachea, or windpipe, is a tube made of rings of cartilage that keeps it open at all times for the smooth passage of air. It extends from the larynx down into the chest cavity, where it divides into the two main bronchi. The trachea is lined with cilia and mucus that trap dust and other particles, moving them up toward the throat to be coughed out or swallowed.
5. Bronchi and Bronchioles: The trachea splits into two large tubes called the bronchi (singular: bronchus), which lead into each lung. Once inside the lungs, the bronchi branch into smaller tubes called bronchioles, forming a tree-like structure. The bronchioles continue to divide and become smaller as they spread throughout the lungs, eventually leading to the alveoli, where gas exchange occurs. Like the trachea, the bronchi and bronchioles are lined with mucus and cilia to filter the air.
6. Lungs: The lungs are the primary organs of the respiratory system, consisting of spongy, elastic tissue. They are located on either side of the chest (thorax) and protected by the rib cage. The lungs house millions of tiny air sacs called alveoli, where the crucial process of gas exchange takes place. The right lung has three lobes, while the left lung has two, leaving room for the heart.
Alveoli: The Gas Exchange Hub: The alveoli are tiny, balloon-like structures at the end of the bronchioles. Each alveolus is surrounded by a network of capillaries (tiny blood vessels). When air reaches the alveoli, oxygen from the air passes through the alveolar walls and into the blood in the capillaries. At the same time, carbon dioxide, a waste product from the blood, moves into the alveoli to be exhaled. This exchange of gases is vital for supplying oxygen to the body’s cells and removing carbon dioxide from the blood.
Basic Steps Involved in Respiration
Respiration is a complex process that involves several stages to ensure the body gets the oxygen it needs and removes carbon dioxide efficiently. Below are the basic steps involved:
1. Inhalation and Exhalation: The first step in respiration is inhalation (breathing in) and exhalation (breathing out). During inhalation, air containing oxygen enters the respiratory system through the nose or mouth, travels through the trachea, bronchi, and bronchioles, and eventually reaches the lungs. Exhalation, on the other hand, expels carbon dioxide from the lungs, through the same path but in the opposite direction.
2. Exchange of Gases Between Alveoli and Alveolar Capillaries: Once air reaches the lungs, the oxygen moves into the alveoli, tiny air sacs where the exchange of gases takes place. The walls of the alveoli are very thin and surrounded by a dense network of alveolar capillaries. Here, oxygen from the alveoli diffuses into the blood in the capillaries, and carbon dioxide from the blood diffuses into the alveoli to be exhaled.
3. Transport of Gases to Body Tissues: After oxygen enters the blood, it is transported to various body tissues. Oxygen-rich blood travels from the lungs to the heart via the pulmonary veins. The heart then pumps this oxygenated blood throughout the body via the arteries, delivering oxygen to cells and tissues.
4. Exchange of Gases Between Oxygenated Blood and Body Tissues: As oxygen-rich blood reaches the body tissues, another gas exchange occurs. Oxygen is transferred from the blood to the cells of the tissues, and carbon dioxide, a waste product of cellular respiration, is transferred from the cells into the blood. This deoxygenated blood, now carrying carbon dioxide, travels back to the lungs through the veins.
5. Usage of Oxygen for Cellular Respiration and Releasing Carbon Dioxide: Inside the body’s cells, cellular respiration takes place. This process involves using oxygen to break down glucose and other nutrients to produce adenosine triphosphate (ATP), which is the primary source of energy for cellular functions. During cellular respiration, carbon dioxide is produced as a byproduct and is released into the blood to be carried back to the lungs for exhalation.
Importance of the Lungs: Vital Functions for the Body
The lungs are a crucial organ in the human body, responsible for several essential functions that support life and overall health. Let’s explore the importance of the lungs and the roles they play in maintaining bodily functions.
1. Role in Oxygenating Blood: The primary function of the lungs is to oxygenate the blood. During inhalation, oxygen from the air enters the lungs and moves into the alveoli. From there, it passes into the bloodstream via alveolar capillaries. The oxygen-rich blood is then transported to the heart, which pumps it to the rest of the body. Without the lungs’ role in this process, the body’s cells would be deprived of the oxygen needed to produce energy and function properly.
2. Removal of Carbon Dioxide: In addition to oxygenating the blood, the lungs play a vital role in removing carbon dioxide from the body. Carbon dioxide is a waste product of cellular respiration, which occurs in the body’s cells. The deoxygenated blood, carrying carbon dioxide, returns to the lungs, where the gas diffuses into the alveoli and is exhaled. This constant removal of carbon dioxide is critical for maintaining a balanced pH in the blood and avoiding toxicity.
3. Lungs Support Immunity: The lungs are also important for immune defense, acting as a first line of protection against harmful particles and pathogens. The respiratory system is lined with mucus and cilia that trap dust, bacteria, viruses, and other airborne pollutants. These particles are either expelled through coughing or sneezing or moved to the throat to be swallowed. The lungs also house immune cells that actively fight infections and prevent harmful substances from entering deeper into the body.
4. Importance of Lung Capacity in Physical Stamina and Energy Levels: The capacity of the lungs—the amount of air they can hold and effectively use—is a key factor in physical stamina and energy levels. Increased lung capacity allows for greater oxygen intake and more efficient oxygen delivery to muscles and tissues during physical activities. This is why athletes and physically active individuals often have well-developed lung capacity, which contributes to better endurance and performance. A healthy respiratory system ensures the body gets the oxygen it needs, especially during strenuous exercise or physical exertion.
5. Connection to Overall Wellbeing and Vitality: The health of the lungs is directly tied to overall wellbeing and vitality. When the lungs are functioning properly, the body remains energized, cells receive sufficient oxygen, and the brain functions optimally. Poor lung health, on the other hand, can lead to respiratory issues like asthma, chronic obstructive pulmonary disease (COPD), or lung infections, which can severely impact quality of life, limit physical activities, and drain energy. The lungs are vital to maintaining both physical and mental health, as well as supporting a strong immune system.
Understanding Asthma: A Comparative View of Normal and Asthmatic Lungs
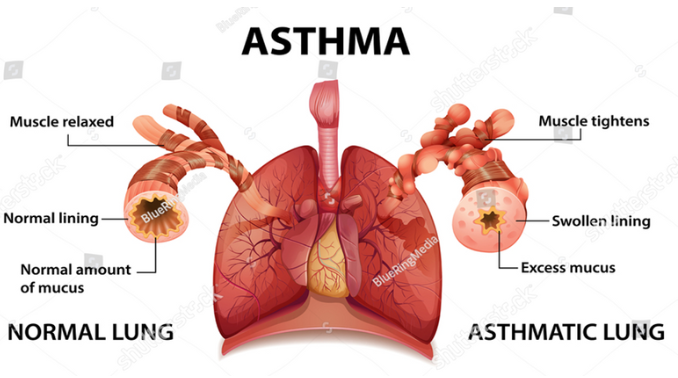
Asthma is a chronic respiratory condition that affects millions of people worldwide. It occurs when the airways become inflamed, leading to difficulty in breathing. This diagram provides a clear comparison between a normal lung and an asthmatic lung, highlighting the changes that occur during an asthma attack.
Anatomy of a Normal Lung:
In a healthy lung, the airways (bronchi) are clear, and the muscles around them are relaxed. Here are the key features:
- Relaxed Muscles: The muscles surrounding the bronchi are in a relaxed state, allowing air to flow freely into the lungs.
- Normal Lining: The inner lining of the bronchial tubes is smooth and thin, ensuring there is no obstruction.
- Normal Mucus Production: Mucus is naturally produced in the lungs, helping to trap dust, allergens, and other irritants. In a normal lung, this mucus is present in a balanced, healthy amount, preventing any blockage in the airways.
Overall, the normal lung functions smoothly, allowing oxygen to be efficiently transferred to the bloodstream.
Anatomy of an Asthmatic Lung:
In contrast, the asthmatic lung shows significant changes that make breathing difficult during an asthma attack. The following are the key features:
- Tightened Muscles: During an asthma attack, the muscles around the bronchi tighten and constrict, making it harder for air to pass through.
- Swollen Lining: The lining of the airways becomes inflamed and swollen. This swelling narrows the passage through which air can flow, causing shortness of breath and chest tightness.
- Excess Mucus Production: In response to inflammation, the lungs produce an excessive amount of thick mucus. This mucus further clogs the already narrowed airways, exacerbating breathing difficulties.
These changes in the asthmatic lung reduce the airflow, making it harder to breathe and often resulting in wheezing, coughing, and a feeling of tightness in the chest.
Diseases Related to the Respiratory System:
The respiratory system is vital for human survival, but it can be susceptible to a range of diseases that can affect its function. Here are some of the most common respiratory diseases:
1. Asthma: Asthma is a chronic condition that causes inflammation and narrowing of the airways in the lungs, making it difficult to breathe. Common symptoms include wheezing, shortness of breath, chest tightness, and coughing. Asthma can be triggered by allergens, respiratory infections, or environmental factors like pollution.
2. Chronic Obstructive Pulmonary Disease (COPD): COPD is a group of progressive lung diseases, primarily chronic bronchitis and emphysema, which cause airflow blockage and breathing difficulties. It is often caused by long-term exposure to irritants like tobacco smoke, air pollution, or dust. Symptoms of COPD include persistent cough, shortness of breath, and frequent respiratory infections. It is a leading cause of death worldwide.
3. Bronchitis: Bronchitis occurs when the bronchial tubes (which carry air to the lungs) become inflamed. Acute bronchitis is usually caused by viral infections and can result in coughing, wheezing, and chest discomfort. Chronic bronchitis, often linked to smoking, is a long-term condition characterized by frequent coughing and mucus production.
4. Pneumonia: Pneumonia is an infection that causes inflammation in the alveoli (air sacs) of the lungs, leading to the accumulation of fluid or pus. This can make it difficult for the lungs to absorb oxygen. Symptoms of pneumonia include cough, fever, difficulty breathing, and chest pain. Pneumonia can be caused by bacteria, viruses, or fungi, and it can range from mild to life-threatening.
5. Tuberculosis (TB): Tuberculosis is a bacterial infection caused by Mycobacterium tuberculosis, which primarily affects the lungs but can spread to other parts of the body. TB spreads through the air when an infected person coughs or sneezes. Symptoms include a persistent cough, weight loss, night sweats, and fever. While TB can be treated with antibiotics, drug-resistant strains have made treatment more challenging.
6. Emphysema: Emphysema is a progressive disease that damages the air sacs in the lungs, reducing their ability to expand and contract properly. This damage causes shortness of breath and a reduced ability to exchange oxygen and carbon dioxide. The most common cause of emphysema is long-term smoking, though environmental factors and genetic conditions can also contribute.
7. Respiratory Allergies (Hay Fever, etc.): Respiratory allergies occur when the immune system reacts to harmless substances like pollen, mold, or pet dander. Hay fever (allergic rhinitis) is the most common respiratory allergy and causes symptoms such as sneezing, runny nose, itchy eyes, and congestion. Although not typically life-threatening, respiratory allergies can significantly affect quality of life.
8. Lung Cancer: Lung cancer is one of the leading causes of cancer-related deaths worldwide. It is most commonly caused by smoking, but exposure to secondhand smoke, air pollution, or toxic chemicals can also increase risk. Early symptoms may include a persistent cough, chest pain, and shortness of breath, but the disease is often diagnosed in later stages when it becomes harder to treat. Lung cancer may spread to other parts of the body if not caught early.
COPD vs. Healthy Lungs: A Visual Guide:
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease that causes breathing difficulties. The condition is primarily caused by long-term exposure to harmful substances like cigarette smoke or pollutants. This diagram compares a healthy lung with a lung affected by COPD, highlighting the structural changes and how they affect breathing.
Anatomy of a Healthy Lung:
In a healthy lung, airways and alveoli (tiny air sacs) function normally, allowing efficient air exchange.
- Bronchioles: In healthy lungs, bronchioles (small branches of the airways) are open and free of obstructions, allowing air to move smoothly.
- Healthy Alveoli: The alveoli, responsible for the exchange of oxygen and carbon dioxide, are intact and properly shaped. This ensures that oxygen can be absorbed efficiently into the bloodstream, and carbon dioxide can be expelled from the body.
This clear and unobstructed airway structure allows for proper lung function, keeping the body oxygenated and healthy.
Anatomy of a Lung with COPD:
In contrast, the lung affected by COPD exhibits significant changes that impair breathing.
- Bronchioles Narrowed and Blocked with Mucus: One of the hallmark features of COPD is the narrowing of the bronchioles. Excessive mucus production clogs these airways, making it difficult for air to pass through. This causes symptoms like coughing, wheezing, and breathlessness.
- Emphysema (Alveolar Damage): In COPD, emphysema occurs, which leads to the breakdown of the alveolar membranes. These membranes are crucial for gas exchange. As they break down, the lung loses its elasticity, reducing its ability to exchange oxygen and carbon dioxide efficiently. This damage makes it increasingly harder for patients with COPD to breathe.
The Impact on Breathing:
The diagram shows how the changes in lung structure due to COPD significantly affect breathing. In healthy lungs, air flows in and out easily, and gas exchange occurs without issue. In COPD, the blocked and damaged airways and alveoli reduce the lung’s ability to take in oxygen and remove carbon dioxide, leading to symptoms like chronic breathlessness, frequent coughing, and fatigue.
Signs and Symptoms of Asthma:
Asthma is a chronic condition that affects the airways, causing them to become inflamed and narrow, leading to breathing difficulties. The symptoms can vary in intensity and may worsen in response to environmental factors or respiratory infections. Here are the key signs and symptoms of asthma:
1. Shortness of Breath: Asthma often causes difficulty in breathing, even during light physical activities or at rest. The sensation of being unable to take a full breath can be distressing, and shortness of breath tends to worsen during an asthma attack.
2. Chest Tightness or Pain: Many people with asthma experience a sensation of tightness in the chest, which can feel like a heavy weight pressing down. In some cases, this may also manifest as a dull or sharp chest pain. This symptom is especially noticeable during an asthma flare-up or attack.
3. Wheezing When Exhaling: Wheezing, a high-pitched whistling sound during breathing, is one of the most common signs of asthma, particularly in children. It usually occurs when exhaling and indicates that the airways are narrowed. Wheezing can also accompany shortness of breath and coughing, making breathing feel more labored.
4. Trouble Sleeping: Asthma symptoms, such as shortness of breath, coughing, or wheezing, often become more pronounced at night or early in the morning, making it difficult to sleep. Many asthma sufferers report waking up at night feeling breathless, leading to disturbed sleep patterns and fatigue.
5. Coughing or Wheezing Attacks Worsened by a Respiratory Virus: A common cold, the flu, or other respiratory viruses can significantly worsen asthma symptoms. People with asthma may experience prolonged coughing or wheezing episodes triggered by these viral infections. This is because respiratory viruses further inflame the already sensitive airways, leading to more intense symptoms.
Main Symptoms of Chronic Obstructive Pulmonary Disease (COPD)

COPD is a chronic lung disease that causes obstructed airflow from the lungs, making it difficult to breathe. It commonly includes conditions such as chronic bronchitis and emphysema. The symptoms of COPD can develop slowly and worsen over time. Here are the primary symptoms associated with COPD:
1. Shortness of Breath (Dyspnea): One of the hallmark symptoms of COPD is shortness of breath, especially during physical activities. As the condition progresses, even minimal exertion can cause difficulty breathing. Over time, individuals with COPD may feel breathless even at rest.
2. Cough with Sputum Production: A persistent cough that produces sputum (mucus or phlegm) is common in COPD. This cough, sometimes referred to as a “smoker’s cough,” may worsen in the morning and become more frequent as the disease progresses. The mucus produced is the body’s attempt to clear the airways, but it often leads to further irritation and blockage.
3. Wheezing or Chest Tightness: COPD can cause a wheezing sound when breathing, particularly when exhaling, due to narrowed airways. Along with wheezing, individuals may experience chest tightness or discomfort, which makes breathing feel restricted.
4. Fatigue or Tiredness: Due to the constant effort required to breathe, people with COPD often experience fatigue or a general sense of tiredness. The body uses more energy to compensate for the reduced airflow, leaving the person feeling exhausted, especially after physical activity.
5. Recurring Lung Infections: People with COPD are more prone to lung infections, such as acute bronchitis or pneumonia, because their lungs are weakened and more susceptible to bacteria and viruses. These infections can worsen COPD symptoms and lead to further lung damage. Frequent respiratory infections can cause flare-ups or exacerbations of the disease.
Types of Pneumonia: Understanding Lobe-Specific Inflammation

Pneumonia is a lung infection that causes inflammation in the air sacs (alveoli) and can affect different areas of the lungs. This diagram illustrates the three main types of pneumonia based on the location of inflammation within the lungs:
- Upper Lobe Pneumonia:
- Location: The inflammation is concentrated in the upper lobe of the lung.
- Symptoms: This type may present with more acute symptoms due to its proximity to larger bronchial passages. Symptoms often include fever, cough, chest pain, and difficulty breathing.
- Common Causes: Bacterial infections like Streptococcus pneumoniae, as well as viral infections, can cause upper lobe pneumonia.
- Middle Lobe Pneumonia:
- Location: The infection affects the middle lobe of the lung, which is typically seen in the right lung (due to lung anatomy). This part of the lung may be more prone to mucus accumulation.
- Symptoms: Symptoms are similar to other types of pneumonia but can sometimes be more subtle. Coughing, fever, and localized pain are common.
- Common Causes: Middle lobe pneumonia can be caused by bacteria, viruses, and sometimes fungal infections.
- Lower Lobe Pneumonia:
- Location: The infection primarily affects the lower lobes of the lungs.
- Symptoms: Because the lower lobes are closer to the diaphragm, lower lobe pneumonia can sometimes cause abdominal pain or discomfort, in addition to coughing and shortness of breath.
- Common Causes: Lower lobe pneumonia is frequently associated with aspiration (inhaling foreign material into the lungs) and infections by bacteria like Klebsiella or Haemophilus influenzae.
Signs and Symptoms of Pneumonia:
Pneumonia can range from mild to life-threatening, and its symptoms often depend on the underlying cause, the age, and the overall health of the individual. Below are the common signs and symptoms to watch out for:
1. Chest Pain:
- Individuals with pneumonia often experience chest pain when breathing or coughing. This occurs because the infection causes inflammation in the lungs, irritating the pleura (the thin lining around the lungs and chest wall).
2. Confusion or Changes in Mental Awareness:
- Particularly in older adults, pneumonia can cause confusion or sudden changes in mental alertness. This happens due to a lack of oxygen reaching the brain and is often a sign of severe infection.
3. Cough Producing Phlegm:
- One of the hallmark signs of pneumonia is a persistent cough, which may produce phlegm (mucus). This mucus can be clear, yellow, green, or even tinged with blood, depending on the type and severity of the infection.
4. Fatigue:
- People with pneumonia often feel extremely fatigued and exhausted. This is due to the body’s immune response to the infection, which drains energy reserves as it fights off the illness.
5. Fever, Sweating, and Shaking Chills:
- A high fever, along with sweating and shaking chills, are common signs of infection. These symptoms signal the body’s response to fighting off the pathogens causing pneumonia.
6. Lower-than-Normal Body Temperature:
- In older adults (over 65) or individuals with weakened immune systems, pneumonia may cause a lower-than-normal body temperature (hypothermia), which can be a serious sign of infection.
7. Nausea, Vomiting, or Diarrhea:
- Some individuals with pneumonia may experience nausea, vomiting, or diarrhea, especially if the infection is viral. These gastrointestinal symptoms can be particularly common in children.
8. Shortness of Breath:
- People with pneumonia often have shortness of breath, which can worsen with activity. The infection impairs the lungs’ ability to exchange oxygen, leading to difficulty breathing and feelings of breathlessness.
Signs and Symptoms in Newborns and Infants:
- Newborns and infants with pneumonia may not always exhibit typical signs. They may show subtle symptoms such as:
- Vomiting
- Fever and cough
- Restlessness or lack of energy
- Difficulty breathing and feeding
In some cases, they may appear tired or without energy, and breathing may become labored, which can lead to significant distress.
Signs and Symptoms of Tuberculosis (TB):
Tuberculosis (TB) is a potentially serious infectious disease caused by the bacterium Mycobacterium tuberculosis, primarily affecting the lungs, though it can spread to other parts of the body. TB symptoms can be subtle at first and worsen over time, especially if left untreated. Here are the main signs and symptoms:
1. Persistent Cough:
- A bad cough lasting longer than two weeks is one of the most common early signs of pulmonary TB. The cough may initially be dry but can progress to producing sputum (mucus).
2. Chest Pain:
- TB can cause pain in the chest, especially during deep breaths or coughing. This pain is typically due to inflammation in the lungs or the surrounding pleura (the thin tissue covering the lungs).
3. Coughing Up Blood or Sputum:
- As the infection progresses, people with TB may begin coughing up blood or blood-streaked sputum (mucus). This is a sign that the disease has caused damage to the lung tissue.
4. Fatigue or Weakness:
- People with TB often experience extreme fatigue or weakness. This is due to the body’s immune system working hard to fight off the infection, leaving little energy for daily activities.
5. Loss of Appetite:
- A significant symptom of TB is a loss of appetite. This can occur as a result of the body’s response to the infection, leading to a general decrease in hunger and food intake.
6. Weight Loss:
- Unintentional weight loss is a classic symptom of TB, often referred to as “consumption” in historical texts. Weight loss occurs because of a combination of loss of appetite and the body using more energy to fight the infection.
7. Chills:
- Chills or shivering may accompany fever and are signs that the body is fighting the infection. Chills are common in TB and may come in waves, especially at night.
8. Fever:
- Fever is a common symptom of TB, especially in the active phase of the disease. The fever may be mild, intermittent, or consistent, and it can lead to night sweats, which are particularly common in TB patients.
Understanding Allergic Rhinitis (Hay Fever)

Allergic Rhinitis, commonly known as hay fever, is an allergic reaction that primarily affects the nasal passages. It occurs when the immune system overreacts to environmental triggers like pollen, dust, pet dander, or mold. The first diagram outlines key symptoms of allergic rhinitis, while the second provides tips for avoiding allergic triggers.
Symptoms of Allergic Rhinitis:
- Sneezing, Stuffy Nose, and Runny Nose:
- These are the most common symptoms triggered by inhaled allergens. The body responds by releasing histamines, leading to nasal congestion and a runny nose.
- Mucus and Postnasal Drip:
- Postnasal drip refers to mucus running down the back of the throat, often leading to throat irritation, coughing, or a feeling of needing to clear the throat frequently.
- Sinus Pressure and Headaches:
- Inflammation caused by allergens can lead to sinus congestion, resulting in pressure around the forehead, eyes, and cheeks, sometimes accompanied by headaches.
- Dark Undereye Circles:
- Known as “allergic shiners,” these dark circles are a common side effect of nasal congestion, which affects blood flow around the eyes.
Tips for Avoiding Allergic Triggers:
- Wash Bedding Regularly:
- Washing sheets, pillowcases, and blankets in hot water helps reduce dust mites and allergens that accumulate on fabric surfaces.
- Dust Frequently:
- Keeping your home clean by regularly dusting surfaces can help minimize exposure to allergens such as dust and pet dander.
- Rinse Nasal Passages:
- Nasal irrigation with a saline solution can help flush out allergens and mucus, providing relief from congestion and postnasal drip.
- Wash Hands After Playing with Pets:
- Animal dander is a common allergen. Washing hands after handling pets can prevent allergens from spreading to your face or other surfaces.
- Shut Windows During Pollen Season:
- Keeping windows closed, especially during high-pollen seasons, can help limit the entry of outdoor allergens like pollen into your home.
- Avoid Smoke and Fragrances:
- Strong odors from smoke or fragrances can irritate the nasal passages and exacerbate symptoms of allergic rhinitis.
This diagram highlights the similarities and differences in symptoms between COVID-19 and hay fever (allergic rhinitis). Both conditions share certain symptoms, but key differences can help distinguish between them.
COVID-19 Symptoms:
- Fever or chills
- Loss of taste and smell
- Nausea, vomiting, or diarrhea
- Muscle or joint pain
- Loss of appetite
- Sore throat
Symptoms of Both (COVID-19 and Hay Fever):
- Cough
- Tiredness (fatigue)
- Runny or blocked nose
- Headache
- Shortness of breath (for some people, particularly those with asthma or pre-existing respiratory conditions)
Hay Fever Symptoms:
- Watery, itchy eyes
- Itchy nose
- Sneezing
Key Differences:
- Hay fever commonly involves itchy eyes and nose, which are absent in COVID-19.
- COVID-19 is more likely to cause systemic symptoms like fever, muscle aches, and loss of smell or taste, which are uncommon in hay fever.
- Shortness of breath can occur in both conditions but is typically related to asthma flare-ups in hay fever.
Understanding these differences is critical for correctly identifying the condition and taking appropriate action. If unsure, testing for COVID-19 can help confirm the diagnosis.
Understanding Lung Cancer Stages

Lung cancer is one of the most serious and common types of cancer, affecting millions of people worldwide. This article aims to explain the progression of lung cancer through its stages, as depicted in the provided image.
Healthy Lungs:
The first part of the image shows healthy lungs. Healthy lungs are characterized by a clear, spongy texture and are free of any tumors or abnormal growths. The bronchi (the main air passages into the lungs) and the alveoli (tiny air sacs where gas exchange occurs) are functioning normally, allowing for efficient oxygen intake and carbon dioxide expulsion.
Early-Stage Cancer:
In the middle section of the image, we see lungs affected by early-stage cancer. Early-stage lung cancer is often localized, meaning the cancerous cells are confined to a small area within the lung and have not yet spread to other parts of the body. In this stage, tumors are present, but they are typically small and fewer in number. These tumors may start to disrupt normal lung function but are often detected early enough for effective treatment options, such as surgery or localized therapies.
Late-Stage Cancer:
The final part of the image illustrates lungs with late-stage cancer. In late-stage lung cancer, the tumors have grown significantly larger and more numerous. This advanced stage often involves the spread of cancerous cells beyond the lungs to other parts of the body, a process known as metastasis. The extensive presence of tumors severely impairs lung function, leading to symptoms such as persistent cough, chest pain, shortness of breath, and frequent respiratory infections. Treatment at this stage becomes more complex, typically involving a combination of chemotherapy, radiation therapy, and palliative care to manage symptoms and improve the quality of life.
Symptoms of Lung Cancer:
Lung cancer can often go unnoticed in its early stages, but as the disease progresses, various symptoms may appear. These symptoms can vary depending on the size and location of the tumor, but here are the most common signs:
1. Chest Pain or Discomfort:
- People with lung cancer may experience chest pain or discomfort. This can occur when breathing deeply, coughing, or laughing, and it is usually caused by the tumor pressing on surrounding tissues or nerves.
2. Persistent Cough:
- A cough that doesn’t go away or worsens over time is a common early symptom of lung cancer. The cough may be dry or produce phlegm, and it is often mistaken for other respiratory issues.
3. Coughing Up Blood:
- Lung cancer may cause individuals to cough up blood (hemoptysis), either as streaks in the phlegm or more substantial amounts. This is a sign of advanced cancer affecting the lung tissue and blood vessels.
4. Trouble Breathing:
- As the tumor grows, it may obstruct the airways, leading to shortness of breath or difficulty breathing. This can be worsened by physical activity and may progress over time.
5. Wheezing:
- Wheezing, a high-pitched sound heard during breathing, can be another sign of lung cancer. It occurs when the airways become narrowed or blocked by the tumor.
6. Hoarseness:
- Lung cancer can affect the vocal cords, leading to hoarseness or a raspy voice. This is typically caused by pressure from the tumor on the nerves that control the vocal cords.
7. Loss of Appetite:
- Many lung cancer patients experience a loss of appetite, often leading to a decrease in food intake. This can occur due to a combination of the body’s response to the cancer and the impact on overall well-being.
8. Unexplained Weight Loss:
- Weight loss for no known reason is a common symptom of lung cancer. This is often due to a combination of factors, including reduced appetite, increased energy expenditure by the body, and the tumor’s effects on metabolism.
How Naturopathy Can Help Respiratory Health

Naturopathy offers a holistic approach to improving respiratory health by focusing on natural remedies, lifestyle adjustments, and stress management techniques. Below are some naturopathic methods that can support lung health and alleviate respiratory issues:
1. Dietary Changes:
- Anti-inflammatory foods play a crucial role in reducing inflammation in the respiratory system. Including ginger, turmeric, and green leafy vegetables in your diet can help to calm inflamed airways and strengthen the immune system. These foods also contain antioxidants that combat free radicals, which can aggravate respiratory issues.
2. Breathing Techniques:
- Pranayama, a yogic breathing practice, helps in strengthening lung capacity and improving oxygen intake. Techniques such as Anulom Vilom (alternate nostril breathing) and Kapalbhati (skull-shining breath) can enhance lung function, clear airways, and promote efficient breathing patterns.
3. Hydrotherapy:
- Steam inhalation is a natural way to clear blocked airways and reduce congestion. Adding essential oils like eucalyptus or peppermint to the steam can provide additional relief by soothing the respiratory tract and helping to break up mucus.
4. Herbal Remedies:
- Several herbs are known for their ability to support respiratory health:
- Tulsi (holy basil) helps reduce inflammation and acts as a natural expectorant.
- Licorice soothes the throat and helps with coughing.
- Eucalyptus is beneficial for decongesting the airways, making it easier to breathe.
These herbs can be consumed as teas, used in steam inhalations, or taken as supplements under the guidance of a naturopath.
5. Exercise:
- Yoga asanas that open up the chest and promote deep breathing are excellent for improving lung function. Postures such as Bhujangasana (cobra pose), Matsyasana (fish pose), and Ustrasana (camel pose) help to expand the chest, encourage deep breathing, and strengthen respiratory muscles.
6. Stress Management:
- Meditation and relaxation techniques help in managing stress, which can trigger or worsen respiratory issues. Practices like mindfulness meditation, guided visualization, and progressive muscle relaxation can lower stress levels, reduce anxiety, and, in turn, ease respiratory conditions that are exacerbated by stress.
How Naturopathy Can Help with Respiratory Health through Dietary Changes:
Dietary modifications play a crucial role in supporting lung health, particularly for individuals with respiratory conditions. Naturopathy emphasizes a balanced diet that nourishes the body while avoiding foods that can worsen lung function. Below are some dietary changes that can help improve respiratory health:
1. Limit Simple Carbohydrates:
- Simple carbohydrates, such as those found in sugary snacks, candies, and soft drinks, can contribute to weight gain and blood sugar spikes. Excess weight puts additional strain on the lungs, making it harder to breathe. By reducing the intake of processed sugars and refined carbs, individuals can help manage their lung function and overall health more effectively.
2. Limit Sodium:
- Sodium can cause fluid retention, which may lead to shortness of breath and increased strain on the heart and lungs. To reduce this burden, it’s recommended to keep sodium intake below 2,400 mg daily. Lowering sodium intake can make breathing easier by preventing excess fluid buildup around the lungs and heart.
3. Limit Mucus-Producing Foods:
- Certain foods can increase mucus production, which makes it more difficult to breathe, especially for individuals with lung conditions like asthma or COPD. These foods include:
- Dairy products (milk, cheese, yogurt)
- Fried foods
- Processed sugar
Reducing the consumption of these mucus-producing foods can help alleviate symptoms and improve lung function.
4. Eat Smaller Meals:
- Large meals can put pressure on the diaphragm, the muscle responsible for breathing, making it harder to take deep breaths. By opting for smaller, more frequent meals, you can relieve this pressure, supporting better lung function and easier breathing throughout the day.
5. Eat Foods Rich in Antioxidants:
- Antioxidant-rich foods help protect lung tissues from oxidative damage caused by free radicals. Free radicals can damage cells and worsen lung function. Including foods like:
- Berries (blueberries, strawberries)
- Leafy greens (spinach, kale)
- Colorful vegetables (carrots, bell peppers)
These foods provide essential nutrients that support healthy lung tissues and fight off inflammation.
6. Eat Foods Rich in Magnesium:
- Magnesium plays an important role in supporting lung function and relaxing bronchial muscles, which helps in easier and deeper breathing. Magnesium can also help reduce symptoms of asthma by preventing muscle spasms in the airways. Magnesium-rich foods include:
- Nuts (almonds, cashews)
- Seeds (pumpkin seeds, sunflower seeds)
- Leafy greens (spinach, kale)
- Seafood (salmon, mackerel)
Including these foods in your diet can promote lung relaxation and improve overall respiratory efficiency.
7. Eat More Fruits and Vegetables:
- Fruits and vegetables are packed with antioxidants, vitamins, and minerals that help reduce inflammation and oxidative stress in the lungs. These nutrients protect lung tissues from damage caused by free radicals, which can exacerbate respiratory issues. Additionally, the high water content in fruits and vegetables helps keep the respiratory tract moist, easing breathing.
- Aim to consume two servings of fruits and three servings of vegetables daily for optimal lung health.
8. Eat More Protein:
- Protein is vital for the strength and function of respiratory muscles. Maintaining adequate protein intake is essential for muscle repair and maintenance, which is especially important for individuals with lung conditions. Respiratory muscles are required for effective breathing, and ensuring sufficient protein intake can help maintain these muscles’ health and strength. Sources of protein include:
- Lean meats (chicken, turkey)
- Fish and seafood (salmon, tuna)
- Legumes (lentils, beans)
- Nuts and seeds
Aim to consume protein-rich foods twice a day to maintain lung and overall muscle function.
9. Eat More Fiber:
- A high-fiber diet not only promotes gut health but also has a positive effect on lung function. Fiber-rich foods like fruits, vegetables, whole grains, and seeds help reduce inflammation levels in the body, which may benefit the respiratory system by decreasing the risk of lung diseases. Fiber also helps regulate blood sugar levels, preventing the inflammatory effects of blood sugar spikes. Some high-fiber foods include:
- Whole grains (brown rice, quinoa, oats)
- Nuts and seeds (chia seeds, flaxseeds)
- Legumes (beans, peas)
A high-fiber diet can also promote better digestion, reducing overall inflammation in the body and improving lung function.
Home Remedies for Respiratory Health:
Naturopathy emphasizes natural, at-home remedies to support respiratory health and alleviate symptoms of common respiratory conditions such as colds, asthma, and allergies. The following home remedies can help relieve congestion, soothe irritated throats, and support overall lung function:
1. Steam Inhalation with Essential Oils:
- Steam inhalation is one of the most effective natural remedies for clearing the airways and relieving congestion. Adding essential oils such as eucalyptus or peppermint to the steam enhances the treatment. Both oils have decongestant properties that can help clear mucus and reduce inflammation in the respiratory tract. To use, place a few drops of essential oil in a bowl of hot water, cover your head with a towel, and inhale the steam deeply for 5–10 minutes.
2. Ginger and Turmeric Tea:
- Ginger and turmeric are both powerful natural anti-inflammatories that can help reduce inflammation in the respiratory system. Ginger also promotes better circulation and mucus clearance, while turmeric has strong antioxidant properties that protect the respiratory tissues from oxidative stress. To prepare, boil a small piece of ginger with a pinch of turmeric in water, strain, and sip the tea twice a day for soothing relief.
3. Honey and Warm Water:
- Honey is a natural demulcent that can help soothe sore throats and reduce coughs. It has antibacterial and anti-inflammatory properties that can help fight infections in the respiratory tract. Combine honey with warm water or herbal teas to alleviate throat irritation and improve cough symptoms. A spoonful of honey on its own can also provide immediate relief for a scratchy throat.
4. Garlic and Onion:
- Both garlic and onion are rich in sulfur compounds that have antimicrobial properties and can help fight infections. Garlic, in particular, is known for its ability to boost the immune system and act as a natural antibiotic. Eating raw garlic or onion may help alleviate symptoms of respiratory infections and promote better lung health. You can add these to your meals or chew on a small piece of garlic for maximum benefit.
5. Jaggery or Mint for Coughing:
- Jaggery (gur) is a traditional remedy in many cultures for easing coughs. It is said to have soothing properties that help to clear the respiratory tract. Alternatively, mint is another excellent option to chew on, as it can help reduce irritation in the throat and alleviate coughing. Mint also acts as a natural expectorant, helping to clear mucus from the airways.
6. Saltwater Gargles:
- Saltwater gargles are a simple but effective remedy for relieving throat irritation and soothing a sore throat. Salt helps to reduce inflammation and can kill bacteria in the throat. Dissolve half a teaspoon of salt in warm water and gargle several times a day to relieve discomfort and reduce inflammation.
7. Humidifiers:
- Humidifiers can help keep the airways moist, especially during dry weather or when the air is heavily conditioned. Moist air helps to soothe irritated nasal passages and bronchi, making it easier to breathe. Adding a few drops of essential oils like eucalyptus or lavender to the humidifier can further enhance the effect and promote relaxation and better lung function.
Naturopathy and Detoxification for Respiratory Health:
Naturopathy emphasizes detoxification as a vital process to improve overall health and reduce symptoms of lung diseases. By eliminating toxins and supporting the body’s natural cleansing mechanisms, naturopathy promotes better lung function and resilience. Below are some naturopathic methods used to detoxify the body and support respiratory health:
1. Detoxifying Herbs:
- Herbs are an integral part of naturopathy, and certain detoxifying herbs are known to support lung health by helping clear toxins from the body. These herbs can aid in reducing inflammation, boosting immunity, and promoting better oxygenation. Some common detoxifying herbs for lung health include:
- Multhi (Mullein): Known for its ability to soothe the respiratory tract and clear mucus from the lungs, mullein can be used to improve overall lung function.
- Tulsi (Holy Basil): A powerful adaptogen and anti-inflammatory herb that supports the immune system and helps clear toxins from the body. It also aids in reducing respiratory congestion.
- Ajwan (Carom Seeds): These seeds have antimicrobial properties and are often used in Ayurvedic practices to relieve respiratory ailments and detoxify the lungs.
- Ginger: A natural anti-inflammatory, ginger can support detoxification by improving circulation and reducing inflammation in the respiratory system.
- Pudina (Mint): Known for its soothing and cooling properties, mint helps in clearing congestion and providing relief from respiratory symptoms.
2. Fasting and Juicing:
- Fasting and juicing are common practices in naturopathy to promote detoxification. These methods help clear toxins from the body, reduce inflammation, and improve overall function, including in the respiratory system.
- Fasting: Periodic fasting can give the digestive system a break and allow the body to focus on detoxification. During fasting, the body starts eliminating stored toxins, which includes waste in the respiratory system.
- Juicing: Consuming freshly pressed juices from fruits and vegetables can flood the body with vitamins, minerals, and antioxidants that support the detoxification process. Green juices, rich in chlorophyll, can help oxygenate the blood and support lung health by removing toxins from the lungs and respiratory tissues.
3. Lymphatic Drainage:
- The lymphatic system plays a key role in removing toxins and waste from the body. In naturopathy, lymphatic drainage techniques are used to stimulate this system, promoting detoxification and reducing inflammation in the lungs.
- Dry Brushing: This technique involves gently brushing the skin in upward strokes, stimulating the lymphatic system and promoting the elimination of toxins. Regular dry brushing can improve circulation and help with overall detoxification.
- Lymphatic Massage: A specialized massage technique that targets lymph nodes and encourages the removal of waste and toxins. It can help reduce inflammation in the body and improve lung function by clearing the lungs of toxins.
Aromatherapy for Lung Health

Aromatherapy is a natural and effective way to support lung health and alleviate symptoms of respiratory conditions. Essential oils, derived from plants, are rich in therapeutic properties that can help relax the respiratory system, clear congestion, and reduce inflammation. Here are some essential oils commonly used in aromatherapy to promote better lung function:
1. Eucalyptus Essential Oil:
- Eucalyptus oil is widely known for its ability to open up the airways and improve breathing. It contains eucalyptol, a compound that has expectorant properties, helping to clear mucus and relieve congestion in the respiratory tract.
- How it helps: Eucalyptus oil is especially useful for conditions like asthma, bronchitis, and sinusitis. It helps to reduce inflammation and loosen mucus, making it easier to breathe.
- How to use: Add a few drops of eucalyptus oil to a bowl of steaming hot water for steam inhalation, or use a diffuser to disperse the oil into the air. You can also dilute it in a carrier oil and rub it on the chest to promote better breathing.
2. Peppermint Essential Oil:
- Peppermint oil is rich in menthol, which has a soothing effect on the respiratory system. It helps to calm irritated airways and acts as a natural decongestant, making it particularly beneficial during colds or seasonal allergies.
- How it helps: The menthol in peppermint oil helps open the airways, reduce swelling, and improve airflow. It also has cooling properties that can help relieve the discomfort of tightness in the chest.
- How to use: Diffuse peppermint oil in the room or apply it topically on the chest or neck, diluted in a carrier oil. Inhaling peppermint oil through steam inhalation or directly from a tissue can quickly clear the sinuses and reduce respiratory discomfort.
3. Lavender Essential Oil:
- Lavender oil is widely known for its calming and relaxing properties. Stress and anxiety can often trigger or worsen symptoms in respiratory conditions like asthma and COPD. Lavender oil can help reduce this stress and promote relaxation.
- How it helps: Lavender’s soothing effects can reduce the physical tension and anxiety that may lead to shallow breathing or chest tightness. It also has anti-inflammatory properties, helping to reduce lung inflammation.
- How to use: Diffuse lavender oil in your home to promote a calm atmosphere. You can also add a few drops to a warm bath or apply it to the temples and wrists for stress relief. Breathing in lavender oil before bed can also promote better sleep, which is essential for lung health.
Pranayama for Lung Health

Pranayama, the practice of controlled breathing exercises, is an ancient yogic technique that significantly enhances lung health and overall well-being. It strengthens the respiratory system, increases lung capacity, and helps oxygenate the body. Pranayama also supports detoxification, clears toxins, and promotes relaxation. Regular practice of pranayama can have a profound impact on the lungs, improving their function, and supporting the body in its natural healing processes.
1. Abdominal Breathing (Viashitha Pranayama)
- How it helps: This foundational breathing technique involves deep abdominal breathing, focusing on expanding the diaphragm and increasing lung capacity. It activates the lower lungs, which are often underused in shallow breathing.
- Benefits: Abdominal breathing helps increase oxygen intake, enhances lung function, and reduces stress by stimulating the parasympathetic nervous system. It also helps clear toxins from the body and promotes relaxation.
- How to practice:
- Sit comfortably with your spine straight.
- Place one hand on your abdomen and the other on your chest.
- Inhale deeply through your nose, letting your abdomen expand (not your chest).
- Exhale slowly and completely, drawing your belly button toward your spine.
- Practice for 5–10 minutes, focusing on deep, steady breaths.
2. Sectional Breathing Practices
- How it helps: Sectional breathing techniques help break down the breath into sections, allowing better control and deeper inhalation. These practices train the lungs to take in more air and improve their efficiency.
- Benefits: They enhance lung capacity, improve the ability to breathe deeply, and activate different regions of the lungs. This type of breathing also helps relieve stress and enhances overall respiratory health.
- How to practice:
- Start by practicing Abdominal Breathing and then move to Thoracic Breathing (expanding the chest).
- Finally, practice Clavicular Breathing (filling the upper lungs and collarbone area).
- Combine all three to create a full, deep breath.
3. Kapalbhati (Skull Shining Breath)
- How it helps: Kapalbhati is a powerful cleansing breath that involves forceful exhalations followed by passive inhalations. This technique helps clear toxins, enhance lung capacity, and energize the mind.
- Benefits:
- Improves lung function: The active exhalations help clear the lungs and improve their capacity.
- Clears nasal passages: It can help remove blockages and improve breathing.
- Detoxifies the respiratory system: It expels toxins and improves overall respiratory health.
- Purifies the mind: This technique also calms the mind, enhances mental clarity, and reduces stress.
- How to practice:
- Sit in a comfortable position with your spine straight.
- Take a deep breath in and exhale forcefully through the nose, while drawing the stomach in.
- Focus on quick, rhythmic exhalations and passive inhalations.
- Start with 20-30 repetitions and gradually increase.
4. Anulom Vilom (Alternate Nostril Breathing)
- How it helps: Anulom Vilom involves breathing alternately through the left and right nostrils, helping balance the body’s energy and promote better oxygenation. It improves lung capacity, clears the mind, and relaxes the body.
- Benefits:
- Balances the respiratory system: By clearing the nasal passages, it ensures better airflow through both nostrils.
- Reduces stress: This practice calms the nervous system and helps reduce anxiety and stress.
- Improves oxygenation: Alternating nostrils helps the body absorb more oxygen and improves the efficiency of the lungs.
- Enhances lung capacity: Regular practice improves the lungs’ ability to take in and utilize oxygen.
- How to practice:
- Sit comfortably with a straight spine and relaxed shoulders.
- Use your right thumb to close your right nostril.
- Inhale deeply through your left nostril.
- Close your left nostril with your ring finger, and exhale slowly through your right nostril.
- Inhale through your right nostril, then close it with your thumb, and exhale through your left nostril.
- This is one cycle. Continue for 5-10 minutes, focusing on the breath and the calming effects.
Bhastrika Pranayama (Bellows Breath)
- Benefits: Energizes the lungs, clears mucus, enhances oxygen flow, and strengthens lung capacity.
- How to practice: Inhale and exhale forcefully through the nose in a rhythmic manner, using the diaphragm. This technique helps to increase air intake and cleanse the respiratory system.
Ujjayi Pranayama (Ocean Breath)
- Benefits: Strengthens respiratory muscles, calms the nervous system, improves breath control, and clears congestion. It reduces the effort required to breathe and promotes relaxation.
- How to practice: Inhale and exhale deeply through the nose while constricting the throat slightly, creating a soft ocean-like sound.
Yoga Sat Kriya
- Benefits: Helps in detoxifying the body, improving lung function, and strengthening the core. It enhances overall vitality and clarity.
- How to practice: Sit in a comfortable position, and perform continuous rapid breathing while engaging the core and focusing on rhythmic movements.
Jal Neti
- Benefits: Clears the nasal passages, promotes easy breathing, and removes toxins.
- How to practice: Use a neti pot with warm saline water to flush out the nasal passages.
Sutra Neti
- Benefits: Similar to Jal Neti, this technique cleanses the nasal passages and sinuses.
- How to practice: Insert a soft, thin thread (sutra) through one nostril and pull it out from the other, gently cleaning the nasal passages.
Enhancing Lung Flexibility through Yoga:
Certain yoga poses are designed to stretch and expand the chest and ribcage, which helps in enhancing lung flexibility and capacity. These poses encourage deep inhalation and full lung expansion, improving respiratory function.
1. Camel Pose (Ustrasana):
- How it helps: This backbend opens the chest and stretches the front body, allowing for deeper breathing and increased lung capacity.
- Benefits: It expands the chest, enhances lung flexibility, and helps clear congestion by allowing full expansion of the lungs.
2. Bow Pose (Dhanurasana):
- How it helps: Dhanurasana is another backbend that stretches the chest, abdomen, and thighs while increasing airflow to the lungs.
- Benefits: It improves posture, opens the chest, and increases lung flexibility by encouraging full expansion during inhalation.
3. Cow Pose (Bitilasana):
- How it helps: This pose stretches the front of the body, especially the chest and diaphragm, which promotes better lung capacity.
- Benefits: It helps to open up the lungs, improves respiratory function, and encourages deep, relaxing breaths.
Incorporating these poses into your yoga practice can help improve lung function and flexibility, contributing to better overall respiratory health.
Asanas for Improving Posture and Respiratory Health:
1. Mountain Pose (Tadasana):
- How it helps: Tadasana encourages proper alignment of the spine, shoulders, and neck, which helps to open the chest and promote deeper breathing.
- Benefits: It improves posture by lengthening the spine and aligning the body, making it easier for the lungs to expand fully and for air to flow freely. This helps with better oxygen intake and lung function.
2. Warrior Pose (Virabhadrasana):
- How it helps: Warrior Pose opens the chest and stretches the entire front of the body, which enhances lung expansion.
- Benefits: By improving posture and aligning the spine, this pose allows for deeper breaths and increases oxygen intake, supporting better lung health.
Increasing Oxygen Circulation through Yoga:
Yoga not only helps improve posture but also emphasizes controlled breathing and mindful movement, which significantly enhances oxygen circulation throughout the body. By focusing on deep, conscious breaths, yoga helps deliver more oxygen to the tissues, which can:
- Boost energy levels: Increased oxygenation helps combat fatigue and provides more vitality.
- Support respiratory health: It aids conditions like asthma and COPD, by increasing lung capacity and improving airflow.
- Reduce symptoms: Regular yoga practice can help reduce shortness of breath, wheezing, and other respiratory symptoms by promoting optimal lung function and better oxygen circulation.
Promoting Relaxation Response through Yoga:
Yoga has the unique ability to stimulate the parasympathetic nervous system, which triggers the body’s relaxation response. This helps the body enter a state of calmness and balance, counteracting stress and tension.
- How it helps with respiratory conditions: The relaxation response can ease the symptoms of respiratory conditions like wheezing, shortness of breath, and chest tightness. By promoting relaxation, yoga helps reduce the physical and emotional stress that can worsen these symptoms, allowing for smoother and deeper breathing.
Boosting Immune Function with Yoga:
Regular yoga practice strengthens the body’s immune system, making it more efficient at defending against infections and illnesses, including respiratory conditions.
- How it helps with respiratory health: A robust immune system is crucial for preventing respiratory infections like pneumonia, bronchitis, and colds that can exacerbate conditions such as asthma and COPD.
- Benefits: By boosting immune function, yoga reduces the frequency of respiratory infections and aids in faster recovery from respiratory-related ailments, promoting long-term lung health and overall well-being.
By incorporating yoga into your daily routine, you not only enhance lung function but also promote relaxation and strengthen your immune system, ultimately improving your respiratory health and quality of life.
Supporting Lifestyle Modifications through Yoga:
Incorporating Yoga into a comprehensive treatment plan for respiratory conditions can significantly complement other lifestyle changes that improve overall health. Yoga not only enhances physical lung function but also encourages healthy habits and mindset shifts, which are crucial for managing respiratory conditions.
Key Lifestyle Modifications Supported by Yoga:
- Smoking Cessation:
- Yoga can help reduce stress and anxiety, often triggers for smoking. By promoting relaxation and mindfulness, it can serve as a healthy alternative to smoking and support the effort to quit.
- Maintaining a Healthy Weight:
- Yoga promotes physical fitness and helps maintain a healthy body weight, which reduces the strain on the respiratory system. It encourages mindful eating habits, supports digestion, and strengthens the lungs, allowing for more efficient breathing.
- Avoiding Environmental Triggers:
- Yoga enhances body awareness and mindfulness, which helps individuals become more attuned to environmental factors that trigger respiratory symptoms, such as pollutants or allergens. It also encourages practices that promote better air quality in living spaces (like keeping the air clean and using essential oils) for better lung health.
By integrating yoga into these lifestyle modifications, individuals can create a holistic approach to managing respiratory conditions and improve overall well-being.
Hydrotherapy for Respiratory Health

Hydrotherapy, or water-based treatments, offers several benefits for respiratory health by improving circulation, reducing inflammation, and enhancing lung function. These methods work to alleviate symptoms and support the body’s natural healing process.
1. Steam Inhalation:
- How it helps: Inhaling steam helps loosen mucus, relieve congestion, and soothe inflamed airways.
- Enhancement with essential oils: Adding eucalyptus or peppermint essential oils to the steam can enhance its decongestant and soothing effects, allowing for easier breathing and clearing of the respiratory passages.
2. Hot and Cold Compresses:
- How it helps: Alternating between hot and cold compresses applied to the chest can improve blood circulation to the lungs, helping to reduce inflammation and promote better oxygenation of the tissues.
- Potli Sayak: A traditional technique that involves applying a herbal bundle (Potli) soaked in hot water to the chest, further enhancing the soothing and healing effects.
3. Chest Packs:
- How it helps: Using a warm, wet towel or pack on the chest for 15-20 minutes helps break up mucus, making it easier to expel.
- Follow-up with cold compress: After using the warm pack, applying a cold compress stimulates circulation and helps reduce inflammation, improving overall lung function.
Incorporating hydrotherapy techniques like these into a respiratory health regimen can significantly support lung function, ease symptoms, and promote faster recovery from respiratory ailments.
Acupuncture and Acupressure for Respiratory Health:
Both Acupuncture and Acupressure are key therapeutic practices in naturopathy that focus on balancing the body’s energy flow (Qi) and improving overall health, including lung health.
Acupuncture for Lung Health:
- How it works: Acupuncture involves inserting fine needles into specific points on the body. These points are chosen based on their ability to stimulate energy flow and target specific health issues.
- Benefits for lung health: Acupuncture is particularly effective in managing respiratory conditions such as asthma, COPD, chronic bronchitis, and allergies. By enhancing Qi flow, acupuncture helps reduce inflammation, improve oxygen intake, and promote better lung function.
Acupressure for Respiratory Health:
- How it works: Acupressure involves applying pressure to specific points on the body, such as the lung meridian, which runs along the arms and chest.
- Benefits for lung health: By stimulating these points, acupressure helps relieve respiratory symptoms like wheezing, shortness of breath, and coughing. It promotes better breathing, reduces congestion, and supports overall lung function by encouraging energy flow and reducing stress.
Both acupuncture and acupressure provide holistic approaches to supporting lung health, addressing underlying energy imbalances, and improving the body’s natural ability to heal and function optimally.
Sunlight and Vitamin D for Lung Health

Exposure to natural sunlight plays a vital role in supporting overall health, especially in lung health. One of its primary benefits is the body’s ability to produce Vitamin D when exposed to sunlight. Vitamin D has been shown to significantly improve lung function and help reduce inflammation in individuals suffering from lung diseases.
How Vitamin D Supports Lung Health:
- Improved Lung Function: Vitamin D helps regulate the immune system and reduce inflammation, which is essential for optimal lung function. It has been linked to improved breathing and better respiratory health in conditions like asthma, COPD, and bronchitis.
- Reducing Inflammation: Vitamin D acts as an anti-inflammatory agent, helping to reduce the chronic inflammation that often exacerbates respiratory conditions. It may improve the function of immune cells in the lungs, supporting better responses to respiratory infections.
Ensuring Adequate Vitamin D:
- Natural sunlight: Spending around 10-30 minutes in direct sunlight (depending on skin type, time of day, and location) allows the skin to produce sufficient Vitamin D.
- Supplements: If sunlight exposure is limited, especially in winter or for individuals with darker skin, Vitamin D supplements can help maintain optimal levels and support lung health.
Lifestyle Modifications for Better Lung Health
Adopting healthy lifestyle habits is crucial in managing lung disease naturally and improving overall respiratory function. Naturopathy emphasizes a holistic approach to wellness, encouraging changes in diet, exercise, and mindset to support lung health.
1. Quit Smoking
- Why it matters: Smoking is the leading cause of lung disease, including conditions like COPD, chronic bronchitis, and lung cancer.
- Naturopathic approach: Naturopathy provides natural remedies like herbal treatments (e.g., lobelia and St. John’s wort) to ease nicotine withdrawal and reduce cravings, making it easier to quit smoking and start healing the lungs.
2. Stress Management
- Why it matters: Stress can worsen symptoms of lung diseases by tightening the chest, restricting breathing, and increasing inflammation.
- Naturopathic approach: Techniques such as yoga, meditation, and relaxation exercises help reduce stress, promote relaxation, and improve lung function. Regular deep breathing exercises can particularly support the relaxation of respiratory muscles.
3. Regular Exercise:
- Why it matters: Regular physical activity boosts lung capacity, strengthens the respiratory muscles, and enhances overall health. It also improves circulation, helping the body transport oxygen more efficiently.
- Naturopathic approach: Low-impact exercises like walking, swimming, or yoga are especially beneficial for lung health. These exercises are gentle on the body while improving lung function, endurance, and energy levels.
How to Strengthen Your Lungs and Breathe Better:
Maintaining strong and healthy lungs is crucial for overall well-being. The following tips, as depicted in the infographic, provide a comprehensive guide to improving lung health and enhancing respiratory function.
1. Invest in an Air Filter: Using an air filter in your home helps to remove pollutants and allergens from the air, ensuring that you breathe cleaner air. This can significantly reduce the risk of respiratory issues and improve lung health.
2. Exercise Regularly: Regular physical activity is essential for maintaining lung capacity and function. Activities such as walking, jogging, swimming, and aerobic exercises help to strengthen the respiratory muscles and improve oxygen intake.
3. Eat Healthy Foods: A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients that support lung health. Foods high in antioxidants, such as berries and leafy greens, help to protect the lungs from damage caused by free radicals.
4. Avoid Exposure to Air Pollutants:
Minimizing exposure to harmful air pollutants, such as industrial emissions, vehicle exhaust, and secondhand smoke, is vital for lung health. Wearing masks in polluted areas and using air purifiers indoors can help reduce exposure.
5. Stop Smoking: Smoking is one of the leading causes of lung damage and respiratory diseases. Quitting smoking can significantly improve lung function and reduce the risk of lung cancer, chronic obstructive pulmonary disease (COPD), and other respiratory conditions.
6. Perform Breathing Exercises: Breathing exercises, such as diaphragmatic breathing and pursed-lip breathing, can enhance lung capacity and efficiency. These exercises help to strengthen the diaphragm, increase oxygen intake, and improve overall respiratory function.
7. Get Regular Check-Ups: Regular medical check-ups are important for early detection and management of lung diseases. Routine lung function tests and screenings can help identify potential issues early, allowing for timely intervention and treatment.
8. Reduce Your Stress Levels: High stress levels can negatively impact respiratory health. Practicing stress-reducing techniques such as meditation, yoga, and deep breathing can help to calm the mind and improve breathing patterns.
Diagnostic Tests for Respiratory Health: Blood Tests and Imaging

When it comes to diagnosing respiratory conditions, a combination of blood tests and imaging procedures is essential to gain a comprehensive understanding of lung health. These diagnostic tools help identify underlying issues, guide treatment, and monitor progress over time. Below are some of the most commonly used blood tests and imaging methods for assessing lung function and overall respiratory health.
Blood Tests for Respiratory Health:
- Complete Blood Count (CBC): A Complete Blood Count (CBC) is a basic yet important blood test that helps evaluate overall health. It checks for infections, anemia, and other blood disorders. By measuring levels of red blood cells, white blood cells, and platelets, a CBC can identify signs of infection or inflammation, which could indicate an underlying respiratory condition.
- Arterial Blood Gas (ABG): An Arterial Blood Gas (ABG) test is crucial for assessing how well the lungs are functioning in terms of oxygenating the blood and removing carbon dioxide. The test measures the levels of oxygen (O2), carbon dioxide (CO2), and the pH balance of the blood. This is especially useful for people with lung diseases like COPD, asthma, or pulmonary fibrosis.
- Allergy Testing (IgE Levels): Allergy testing, particularly measuring Immunoglobulin E (IgE) levels, can help identify allergens that might be exacerbating respiratory symptoms. Allergens such as pollen, dust mites, mold, and pet dander can trigger or worsen conditions like asthma or allergic rhinitis. Knowing which allergens to avoid can help manage symptoms and improve lung function.
Imaging Procedures for Lung Health:
- Chest X-ray: A chest X-ray is one of the most common imaging tests used to diagnose lung conditions. It helps detect infections, fluid in the lungs, tumors, and structural abnormalities such as collapsed lungs or pleural effusion. X-rays provide a quick and effective way to examine the lungs, especially in acute conditions.
- Pulmonary Function Test (PFT): Pulmonary Function Tests (PFTs) are used to evaluate lung capacity and function. These tests measure how much air you can inhale and exhale, and how efficiently your lungs exchange gases like oxygen and carbon dioxide. PFTs are particularly useful for diagnosing chronic respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and restrictive lung diseases.
- CT Scan: A CT (computed tomography) scan offers detailed, cross-sectional images of the lungs. Unlike X-rays, CT scans provide more comprehensive information and can detect smaller abnormalities, including tumors, pulmonary embolisms, and interstitial lung diseases. If a chest X-ray reveals any suspicious findings, a CT scan may be recommended for further evaluation.
Arterial Blood Gas (ABG) Test: A Key Diagnostic Tool for Lung Health:
An Arterial Blood Gas (ABG) test is a crucial diagnostic tool for evaluating lung function and respiratory health. It provides detailed insights into the levels of oxygen and carbon dioxide in the blood, along with the blood’s pH balance. This test is especially important for individuals with respiratory conditions, offering essential data for diagnosing and managing lung diseases.
What is an Arterial Blood Gas (ABG) Test?
An ABG test involves drawing a blood sample from an artery, typically from the wrist or groin. The procedure is slightly more invasive than a standard blood test, which is why it is performed in clinical settings rather than during routine checkups.
This test measures the following parameters:
- Oxygen (O₂): The amount of oxygen in the blood, which indicates how well the lungs are transferring oxygen into the bloodstream.
- Carbon Dioxide (CO₂): The amount of carbon dioxide, which tells how efficiently the lungs are eliminating this waste gas.
- Blood pH (acidity): This measures the balance between acids and bases in the blood, which is crucial for overall body function. An abnormal pH level may suggest issues with lung or kidney function.
Purpose and Relevance to Lung Diseases:
The ABG test is primarily used to assess the effectiveness of the lungs in delivering oxygen to the blood and removing carbon dioxide. It’s an essential test for diagnosing and monitoring a range of lung diseases and conditions, including:
- Chronic Obstructive Pulmonary Disease (COPD): In COPD, the lungs become less efficient at exchanging gases, leading to lower oxygen levels and higher CO₂ levels in the blood.
- Asthma: Asthma can cause intermittent airflow restriction, affecting oxygen and carbon dioxide levels.
- Pulmonary Fibrosis: This lung disease involves the thickening and scarring of lung tissue, which can impede gas exchange.
- Emphysema: A type of COPD, emphysema leads to the destruction of air sacs in the lungs, reducing oxygen uptake and CO₂ elimination.
In emergency situations, an ABG test can help identify hypoxemia (low oxygen levels) and hypercapnia (high carbon dioxide levels), both of which are common in severe respiratory distress or failure.
How ABG Results Help in Diagnosis:
The results of an ABG test can offer critical clues about lung function and ventilation issues. Here’s how the results are interpreted:
- Low Oxygen Levels (Hypoxemia):
Hypoxemia indicates that the lungs are not effectively transferring oxygen into the bloodstream. This may be a sign of severe respiratory conditions like pulmonary edema, asthma exacerbations, or acute respiratory distress syndrome (ARDS). - High CO₂ Levels (Hypercapnia):
Elevated carbon dioxide levels suggest that the lungs are not able to remove CO₂ efficiently. This can occur due to hypoventilation (shallow or slow breathing), respiratory failure, or severe COPD. High CO₂ levels can lead to respiratory acidosis, a condition where the blood becomes too acidic. - Abnormal pH:
An abnormal pH (either acidic or alkaline) indicates an imbalance in the body’s chemistry. Respiratory acidosis or alkalosis can occur depending on the levels of oxygen and carbon dioxide in the blood, signaling that the lungs or other organs may not be functioning optimally.
C-Reactive Protein (CRP) Test: Understanding Inflammation in Lung Diseases:
The C-Reactive Protein (CRP) Test is an essential blood test used to detect levels of C-reactive protein, a substance produced by the liver in response to inflammation. This test plays a significant role in diagnosing and managing inflammatory conditions, including various lung diseases.
Purpose of the CRP Test:
The CRP test measures the amount of C-reactive protein in the blood, which increases when there is inflammation in the body. It helps healthcare providers assess whether inflammation is present, how severe it is, and whether it may be related to an underlying infection or chronic disease.
Relevance of CRP to Lung Diseases:
Elevated CRP levels are often found in individuals suffering from lung diseases that involve inflammation. Lung conditions such as asthma, chronic obstructive pulmonary disease (COPD), and chronic bronchitis can cause significant inflammation in the airways and lungs. In these cases, CRP levels rise as the body responds to the irritation and damage within the respiratory system.
Here’s how CRP testing relates to lung health:
- Asthma: During an asthma flare-up, the airways become inflamed, and CRP levels may spike, reflecting the increased inflammation.
- COPD: In individuals with COPD, especially during exacerbations, inflammation worsens, and CRP levels rise. Chronic inflammation in the lungs can lead to the progressive worsening of lung function.
- Chronic Bronchitis: This condition, characterized by ongoing inflammation and irritation of the bronchial tubes, can cause a persistent elevation of CRP levels.
Interpreting CRP Levels in Lung Conditions:
- High CRP Levels: Elevated CRP levels may indicate an ongoing infection, such as pneumonia or a bacterial respiratory infection, which can exacerbate conditions like asthma or COPD. CRP levels may also rise during acute lung inflammation or flare-ups of chronic lung diseases.
- CRP and Monitoring Treatment: CRP tests can be useful for monitoring how well treatment for inflammatory lung diseases is working. A reduction in CRP levels may suggest that inflammation is decreasing, and the body is responding well to therapies such as bronchodilators, corticosteroids, or antibiotics.
Why CRP Matters for Lung Health:
Tracking CRP levels can help doctors:
- Diagnose and confirm the presence of lung inflammation or infection.
- Monitor treatment progress for individuals with chronic lung conditions.
- Predict possible exacerbations of chronic conditions such as COPD or asthma, which can help guide adjustments to treatment plans.
Erythrocyte Sedimentation Rate (ESR) Test: A Marker for Lung Inflammation
The Erythrocyte Sedimentation Rate (ESR) Test is another blood test used to detect inflammation in the body. While it doesn’t pinpoint the exact cause of inflammation, it is helpful in diagnosing and monitoring conditions, including those that affect the lungs.
Purpose of the ESR Test
The ESR test measures how quickly red blood cells (erythrocytes) settle at the bottom of a test tube over a set period. Normally, red blood cells settle relatively slowly. However, when there’s inflammation in the body, proteins like fibrinogen cause the red blood cells to clump together, making them settle faster than usual.
Relevance of ESR to Lung Diseases
Like the C-Reactive Protein (CRP) test, the ESR test is a non-specific marker of inflammation, meaning it can indicate that inflammation is present but not what is causing it. In the context of lung diseases, elevated ESR levels are often associated with various respiratory conditions, particularly those involving significant inflammation.
Here’s how ESR relates to different lung conditions:
- Pulmonary Infections: Conditions like pneumonia or tuberculosis can cause a significant rise in ESR levels, indicating infection-related inflammation in the lungs.
- Sarcoidosis: An inflammatory disease that often affects the lungs, sarcoidosis can cause a high ESR, reflecting the inflammation present in the affected tissues.
- Pulmonary Fibrosis: In patients with pulmonary fibrosis, ESR can help monitor disease progression as this condition leads to scarring of lung tissues and chronic inflammation.
- Lung Cancer: Elevated ESR levels may also be seen in lung cancer, especially when the cancer is accompanied by inflammation or infection in the lung tissues.
Interpreting Elevated ESR Levels in Lung Disease:
- High ESR Levels: A faster-than-normal sedimentation rate generally points to inflammation. In the case of lung diseases, a high ESR may suggest infections (such as pneumonia), chronic inflammatory lung conditions (like sarcoidosis or pulmonary fibrosis), or lung cancer.
- Tracking Disease Activity and Treatment Response: ESR is often used in conjunction with other tests (like CRP) to monitor disease activity and the body’s response to treatment. For example, a decrease in ESR after starting therapy for conditions like pulmonary fibrosis or sarcoidosis may indicate that the treatment is working.
Why ESR Matters in Managing Lung Health:
The ESR test is particularly useful for:
- Detecting ongoing inflammation in individuals with lung diseases.
- Monitoring the progression of inflammatory lung conditions.
- Helping healthcare providers evaluate treatment effectiveness by comparing ESR levels over time.
D-dimer Test: Screening for Blood Clots in the Lungs:
The D-dimer test is a blood test that plays a crucial role in diagnosing and ruling out serious conditions related to blood clots. In particular, it is often used to detect pulmonary embolism (PE), a condition where a blood clot travels to the lungs and blocks blood flow, potentially leading to life-threatening complications.
Purpose of the D-dimer Test:
The test measures the level of D-dimer, a protein fragment that is produced when a blood clot dissolves in the body. Normally, D-dimer levels are very low in the bloodstream. However, if a clot is present and being broken down, D-dimer levels will rise.
Relevance of the D-dimer Test to Lung Disease:
- Pulmonary Embolism (PE): Elevated D-dimer levels suggest the presence of abnormal blood clotting, which could indicate a pulmonary embolism. A pulmonary embolism occurs when a clot from elsewhere in the body (often from a deep vein thrombosis, or DVT) travels to the lungs, causing chest pain, difficulty breathing, and reduced oxygen levels.
- Further Investigations: While elevated D-dimer levels may indicate the presence of clots, the test alone is not definitive. If D-dimer levels are high, healthcare providers often order further diagnostic tests, such as a CT pulmonary angiography, to confirm whether a blood clot has indeed lodged in the lungs.
Interpreting D-dimer Test Results:
- High D-dimer Levels: Elevated levels suggest the need for further testing to rule out blood clots, especially in the lungs.
- Normal D-dimer Levels: A normal result typically rules out the presence of significant blood clots.
Lactate Dehydrogenase (LDH) Test: Assessing Lung Damage and Disease:
The Lactate Dehydrogenase (LDH) test measures the amount of LDH, an enzyme found in nearly every tissue in the body, including the lungs. LDH is released into the blood when cells are damaged or destroyed, making it a valuable marker for assessing tissue damage and diseases, including those that affect the lungs.
Purpose of the LDH Test:
LDH levels rise when tissue damage occurs, so this test can help in detecting and monitoring lung damage or the presence of lung diseases. It is particularly useful in assessing the severity of the condition and in diagnosing complications that may arise from lung diseases.
Relevance of LDH to Lung Diseases:
- Pneumonia: LDH levels are often elevated in pneumonia, a lung infection that causes inflammation and damage to lung tissue.
- Pulmonary Fibrosis: Patients with pulmonary fibrosis (scarring of the lungs) may have higher-than-normal LDH levels due to ongoing lung tissue damage.
- Lung Cancer: In cases of lung cancer, elevated LDH can be an indicator of lung cell destruction or metastasis (cancer spreading to other parts of the body).
- Pleural Effusion: LDH is also important in diagnosing pleural effusion, a condition where fluid builds up around the lungs. Testing LDH levels in the pleural fluid helps determine whether the effusion is due to infection, cancer, or other conditions.
Interpreting LDH Test Results:
- Elevated LDH Levels: High levels of LDH may point to lung damage or diseases like pneumonia, pulmonary fibrosis, or lung cancer.
- Pleural Effusion Diagnosis: In patients with fluid around the lungs, the LDH test can help differentiate between different causes of pleural effusion, whether it’s infection-related or due to more severe issues like cancer.
Alpha-1 Antitrypsin (AAT) Deficiency Test: Detecting Genetic Risks for Lung Disease
The Alpha-1 Antitrypsin (AAT) deficiency test is a blood test that measures the levels of alpha-1 antitrypsin, a protein produced by the liver that helps protect the lungs from damage caused by inflammation and irritants like cigarette smoke.
Purpose of the AAT Deficiency Test:
This test is particularly important in diagnosing genetic AAT deficiency, which increases the risk of developing serious lung diseases, including chronic obstructive pulmonary disease (COPD) and emphysema, especially in individuals who have never smoked or have minimal exposure to lung irritants.
Relevance of AAT Deficiency to Lung Disease:
- Chronic Obstructive Pulmonary Disease (COPD): AAT deficiency is one of the leading genetic causes of early-onset COPD. If the body has low levels of this protein, the lungs become more vulnerable to damage, resulting in conditions like emphysema.
- Emphysema: People with AAT deficiency are at a much higher risk of developing emphysema at an early age, even without smoking. This condition involves the destruction of the air sacs in the lungs, leading to difficulty breathing.
- Bronchiectasis: This test can also help diagnose bronchiectasis, a condition where the airways become abnormally widened due to inflammation, often linked to AAT deficiency.
Testing for AAT deficiency is particularly recommended for younger individuals (under 45) with unexplained lung problems or a family history of lung disease.
Interpreting AAT Deficiency Test Results:
- Low AAT Levels: Suggest a hereditary predisposition to lung disease. This finding indicates that the person may be at higher risk for developing COPD, emphysema, or bronchiectasis.
- Normal AAT Levels: Typically rule out AAT deficiency as a cause of lung problems.
Allergy Testing (IgE Levels): Identifying Triggers for Respiratory Conditions:
Allergy testing, specifically measuring Immunoglobulin E (IgE) levels, helps identify allergic reactions that may worsen or trigger lung conditions such as allergic asthma.
Purpose of the IgE Allergy Test:
IgE is an antibody produced by the immune system in response to allergens such as pollen, dust mites, or pet dander. The test helps determine if high IgE levels are contributing to respiratory issues by identifying specific allergens.
Relevance of IgE Levels to Lung Disease:
- Allergic Asthma: Elevated IgE levels are commonly found in people with allergic asthma, a form of asthma triggered by allergens. Identifying the specific allergen responsible can help manage asthma by avoiding those triggers or through treatments like allergy shots.
- Allergic Reactions: High IgE levels may indicate sensitivity to environmental allergens such as pollen, mold, animal dander, or dust mites, all of which can worsen respiratory symptoms or contribute to chronic lung conditions like asthma.
- Managing Exacerbations: For individuals with asthma or other allergic respiratory conditions, IgE testing helps healthcare providers identify specific triggers and tailor the treatment plan to avoid allergen exposure and minimize flare-ups.
Interpreting IgE Allergy Test Results:
- High IgE Levels: Indicate an allergic response. If high levels are detected, additional testing (such as skin prick tests) can help pinpoint specific allergens responsible for worsening respiratory conditions.
- Normal IgE Levels: Suggest that allergies are not a major factor in the person’s respiratory issues.
Procalcitonin Test: Identifying Bacterial Lung Infections
The Procalcitonin test measures the levels of procalcitonin, a protein that increases in the body during bacterial infections. This test is especially useful in distinguishing between bacterial and viral infections.
Purpose of the Procalcitonin Test
Procalcitonin levels rise significantly during bacterial infections but remain low in most viral infections. This makes it a critical tool for diagnosing bacterial lung infections like pneumonia or sepsis related to lung conditions.
Relevance of Procalcitonin to Lung Disease
- Bacterial Pneumonia: Elevated procalcitonin levels can indicate the presence of bacterial pneumonia, helping healthcare providers determine whether antibiotics are necessary. This is especially important in distinguishing community-acquired bacterial pneumonia from viral causes of respiratory illness.
- Sepsis: In cases where a lung infection leads to sepsis (a potentially life-threatening systemic infection), procalcitonin levels can help identify the bacterial origin of the infection.
- Antibiotic Stewardship: By using procalcitonin levels to differentiate bacterial from viral infections, healthcare providers can avoid unnecessary antibiotic use, which helps prevent antibiotic resistance.
Interpreting Procalcitonin Test Results
- Elevated Procalcitonin Levels: Suggest a bacterial infection, such as bacterial pneumonia or sepsis. This finding may warrant antibiotic treatment.
- Low Procalcitonin Levels: Likely indicate a viral infection or non-infectious cause of lung symptoms, helping avoid unnecessary antibiotics.
Serum Electrolytes: Monitoring Acid-Base Balance in Lung Disease
Serum electrolyte tests measure the levels of key electrolytes—sodium (Na+), potassium (K+), chloride (Cl-), and bicarbonate (HCO₃-)—that are crucial for maintaining fluid balance, acid-base equilibrium, and proper lung function.
Purpose of the Serum Electrolytes Test
This test helps monitor the body’s electrolyte levels, which are essential for regulating acid-base balance and ensuring proper function of muscles and nerves, including the muscles involved in breathing.
Relevance of Electrolytes to Lung Disease
- Respiratory Acidosis: In lung diseases like chronic obstructive pulmonary disease (COPD) or asthma, impaired lung function can lead to respiratory acidosis, where excess carbon dioxide (CO₂) builds up in the blood, lowering pH levels. The body compensates by increasing bicarbonate (HCO₃-) levels to neutralize the acidity.
- Respiratory Alkalosis: In contrast, hyperventilation (over-breathing) caused by conditions like asthma attacks can result in respiratory alkalosis, where CO₂ levels drop, causing the blood to become too alkaline. This can disrupt electrolyte balance, particularly chloride and bicarbonate.
- Fluid and Electrolyte Imbalances: Lung diseases can also impact fluid regulation, leading to abnormal sodium and potassium levels. For example, hypokalemia (low potassium) can occur in individuals using certain medications, such as diuretics, to manage lung conditions.
Monitoring these electrolytes helps healthcare providers assess how lung disease is affecting overall acid-base balance and fluid regulation, allowing for targeted interventions.
Interpreting Serum Electrolytes Test Results
- Low Bicarbonate Levels: May indicate respiratory alkalosis, often seen in hyperventilation.
- High Bicarbonate Levels: May point to respiratory acidosis, commonly associated with lung diseases like COPD.
- Abnormal Sodium or Potassium Levels: Can signal an electrolyte imbalance that may require correction, particularly in patients with chronic lung diseases.
Sputum Culture and Sensitivity: Diagnosing Respiratory Infections
The Sputum Culture and Sensitivity test examines mucus (sputum) from the lungs to identify whether a bacterial, viral, or fungal infection is present. This test is particularly useful for diagnosing infections deep within the respiratory system that may not be detected through a simple throat or nasal swab.
Purpose of the Sputum Culture and Sensitivity Test
The test isolates and identifies the microorganisms present in the sputum and determines which antibiotics or antifungal treatments will be most effective.
Relevance of Sputum Culture to Lung Disease
- Tuberculosis (TB): This test is crucial for diagnosing tuberculosis, a serious bacterial infection that affects the lungs. Sputum samples can reveal the presence of the Mycobacterium tuberculosis bacteria.
- Pneumonia: In cases of pneumonia, particularly in patients who do not respond to initial treatments, a sputum culture can help pinpoint the exact cause of the infection, such as Streptococcus pneumoniae, and determine the most effective antibiotic.
- Chronic Bronchitis: Chronic lung conditions like bronchitis often involve bacterial infections. A sputum test helps detect ongoing infections, allowing for targeted treatments to prevent worsening symptoms.
- Sensitivity Testing: The test also performs a sensitivity analysis, helping healthcare providers choose the correct antibiotics to combat the specific strain of bacteria. This is vital to prevent antibiotic resistance.
Interpreting Sputum Culture Results
- Bacterial Growth: Indicates a bacterial infection, such as TB or pneumonia, that requires targeted antibiotics.
- No Growth: May suggest that the infection is viral or fungal, or that a deeper diagnostic approach is needed.
Lung Cancer Biomarkers: Early Detection and Monitoring

Lung cancer biomarkers are substances or proteins found in blood, urine, or other tissues that may indicate the presence of lung cancer. These markers play a pivotal role in early detection, diagnosis, and monitoring the progression of the disease.
Purpose of Lung Cancer Biomarkers Test
The test measures the levels of specific proteins or substances that are commonly associated with lung cancer cells. The presence of these markers helps confirm a lung cancer diagnosis and offers insights into the prognosis and effectiveness of treatment.
Relevance of Biomarkers to Lung Disease
- Carcinoembryonic Antigen (CEA): Elevated levels of CEA can suggest the presence of certain types of lung cancer, such as adenocarcinoma. Monitoring CEA levels over time helps assess the effectiveness of cancer treatment or detect recurrence.
- Neuron-Specific Enolase (NSE): NSE is particularly important in diagnosing small cell lung cancer (SCLC), a fast-growing form of lung cancer. High NSE levels can indicate advanced or metastatic disease.
- Prognosis and Treatment: Elevated biomarker levels provide important clues about the stage of lung cancer, enabling healthcare providers to choose appropriate treatment strategies like chemotherapy or targeted therapies. By monitoring these markers during treatment, providers can assess the response and make necessary adjustments.
Interpreting Lung Cancer Biomarker Results
- Elevated Biomarkers: Suggest the presence of lung cancer, prompting further diagnostic steps such as imaging (CT scan) or biopsy.
- Normal Biomarkers: May suggest that cancer is not present, or it is in an early stage, requiring additional testing to confirm.
Blood tests are crucial in evaluating lung health, offering key insights into diagnosing, monitoring, and managing various lung diseases. These tests help assess vital factors such as oxygen levels, detect inflammation or infection, track lung function, and even identify genetic predispositions to certain lung conditions. When combined with other diagnostic tools like chest X-rays, CT scans, and pulmonary function tests, they provide a comprehensive view of the patient’s lung health and the root causes of their condition.
As a naturopathy practitioner, our focus is on restoring balance and promoting the body’s inherent healing abilities. By fostering a healthy environment — through lifestyle modifications, holistic treatments, and stress management — we allow the body to heal from within. Blood tests and modern diagnostic tools complement naturopathic approaches by giving us a clearer understanding of what needs support, allowing us to guide our patients toward better respiratory health naturally.
Chest X-rays
Purpose: A chest X-ray is a quick, non-invasive diagnostic tool used to detect various lung issues. It’s often the first imaging test ordered when lung disease is suspected.
What It Shows:
- Pneumonia
- Chronic Obstructive Pulmonary Disease (COPD)
- Lung Cancer
- Pleural Effusion (fluid around the lungs)
- Tuberculosis (TB)
- Pneumothorax (collapsed lung)
Advantages:
- Fast and Convenient: Provides results quickly, making it ideal for urgent situations.
- Low Cost: More affordable compared to advanced imaging techniques like CT scans.
- Low Radiation Exposure: While it does involve radiation, the levels are much lower than those in more detailed imaging methods.
Limitations:
- Limited Detail: Chest X-rays may not provide enough detail to identify small lesions or detect early-stage diseases.
- Less Sensitivity: Small abnormalities or subtle changes in the lungs can be missed, making it less effective for early diagnosis in some cases.
Overall, chest X-rays are a useful tool for an initial assessment of lung health but are typically followed by more detailed tests (like CT scans) if further evaluation is needed.
CT Scan for Lungs
Purpose: A CT (Computed Tomography) scan provides detailed, cross-sectional images of the lungs, offering a more accurate diagnosis than standard X-rays.
What It Shows:
- Lung Cancer
- Pulmonary Embolism (blood clots in the lungs)
- Interstitial Lung Disease
- Emphysema
- Bronchiectasis
- Small Lung Nodules
Advantages:
- High Detail: Offers much higher resolution compared to standard X-rays, making it ideal for detecting small lesions and early-stage diseases.
- Early Disease Detection: CT scans can identify issues that may not be visible on a chest X-ray, aiding in the early detection of lung diseases.
- 3D Imaging: Provides a more comprehensive view of the lungs in three dimensions, helping doctors to visualize the area better for treatment planning.
Limitations:
- Higher Radiation: CT scans expose patients to more radiation than standard chest X-rays, which can be a concern, especially with repeated tests.
- More Expensive: Due to the advanced technology, CT scans tend to be more costly than X-rays.
- Less Accessible: Not always available in every healthcare setting, especially in remote or underserved areas.
Blood tests, imaging techniques like chest X-rays and CT scans, and other diagnostic tools play an essential role in understanding and managing lung diseases. Blood tests provide valuable insights into oxygen levels, infections, inflammation, organ function, and genetic predispositions, helping healthcare professionals assess lung health and tailor treatment plans. Imaging techniques like chest X-rays offer a quick and effective way to detect various lung conditions, while CT scans provide highly detailed and precise images that aid in diagnosing complex diseases.
From a naturopathic perspective, it’s crucial to understand that these diagnostic methods serve as the foundation for managing lung health, but the true healing begins from within. Naturopathy emphasizes achieving balance through natural remedies, lifestyle modifications, and holistic approaches. By combining conventional medical testing with naturopathic principles, we can offer comprehensive care that supports the body’s ability to heal itself, ultimately fostering long-term respiratory health and well-being.