Thyroid And Goiter
THYROID AND GOITER BY DR AARTI VYAS
The Thyroid Gland: A Key Player in the Endocrine System

The thyroid is a small, butterfly-shaped gland located just below the larynx (voice box), with lobes on either side of the trachea. It is an essential part of the endocrine system and plays a vital role in regulating various bodily functions. Despite its small size, the thyroid’s impact on metabolism, energy regulation, and overall health is significant.
Positioned in the front of the neck, the thyroid secretes hormones that control many body processes, including heart rate, metabolism, and body temperature. Its ability to influence such a wide range of functions makes it one of the most important glands in the human body.
Regulation of Thyroid Hormone Levels:
The levels of thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), are meticulously controlled through a feedback loop system involving several key components of the endocrine system. This regulation ensures that the body maintains appropriate hormone levels for optimal metabolic functioning. Here’s how it works:
- Hypothalamus:
The hypothalamus, located in the brain, serves as the command center for many bodily functions, including the regulation of hormone production. It monitors the body’s needs and responds by releasing thyrotropin-releasing hormone (TRH). TRH signals the pituitary gland to produce thyroid-stimulating hormone (TSH).
- Pituitary Gland:

The pituitary gland, a small pea-sized gland situated at the base of the brain just below the hypothalamus, plays a crucial role in hormone regulation. Upon receiving TRH from the hypothalamus, it releases thyroid-stimulating hormone (TSH) into the bloodstream. TSH then travels to the thyroid gland, stimulating it to produce and release T4 and T3.
- Thyroid Gland:
The thyroid gland, located in the front of the neck, responds to TSH by synthesizing and secreting the thyroid hormones T4 and T3. These hormones are responsible for regulating metabolism, energy production, and other essential bodily functions.
- Feedback Loop:
Once the levels of T4 and T3 in the bloodstream reach a certain threshold, they exert a negative feedback effect on the hypothalamus and pituitary gland. This feedback loop helps maintain hormone balance:
- High Levels of T4 and T3: When the levels of T4 and T3 are sufficiently high, they signal the hypothalamus to decrease TRH production and the pituitary gland to reduce TSH secretion. This results in lower stimulation of the thyroid gland, thus reducing the production of thyroid hormones.
- Low Levels of T4 and T3: Conversely, if T4 and T3 levels drop, the hypothalamus increases TRH secretion, prompting the pituitary gland to release more TSH, which stimulates the thyroid gland to produce more hormones.
Key Points About the Thyroid Gland:
- Feedback Loop Regulation: The levels of thyroid hormones, specifically triiodothyronine (T3) and thyroxine (T4), are regulated through a complex feedback loop. The hypothalamus releases thyrotropin-releasing hormone (TRH), which prompts the pituitary gland to secrete thyroid-stimulating hormone (TSH). TSH then stimulates the thyroid gland to release T3 and T4.
- Thyroid Hormones: T3 and T4 are often collectively referred to as “thyroid hormones.” While T4 is primarily inactive and does not directly impact cellular functions, T3 is the active form that exerts effects on metabolism and various bodily functions.
- Conversion of T4 to T3: After the thyroid releases T4, specific organs in the body convert it into T3, allowing it to influence cellular activity and regulate metabolism effectively.
- Calcitonin Production: In addition to T3 and T4, the thyroid gland also produces a hormone called calcitonin. This hormone helps regulate calcium levels in the blood by decreasing them. However, calcitonin is not classified as a “thyroid hormone” and does not play a role in metabolic regulation like T3 and T4.
The Impact of the Thyroid Gland on Emotions and Energy Levels:
The thyroid gland plays a crucial role in regulating various aspects of our emotional and physical well-being. It significantly influences how we feel and cope with daily challenges, affecting our energy levels, cravings, stress responses, mood swings, patience, anger, and anxiety.
Emotional and Physical Effects
- Energy Levels: Thyroid hormones are essential for regulating metabolism and energy production in the body. When hormone levels are balanced, individuals generally experience stable energy levels. Conversely, imbalances can lead to fatigue or hyperactivity.
- Cravings and Appetite: Thyroid function also affects hunger signals and metabolism. Individuals with thyroid issues may experience changes in appetite and food cravings, which can lead to weight gain or loss.
- Mood Swings: Thyroid hormones impact neurotransmitter activity, which plays a significant role in mood regulation. An underactive or overactive thyroid can contribute to mood swings, anxiety, and feelings of sadness or irritability.
- Stress Response: The thyroid gland influences how the body responds to stress. In times of great stress, the body demands more energy and resources. If the thyroid is unable to meet these increased demands, it can lead to symptoms of stress and anxiety.
Impact of Life Events
Various life events and emotional stimuli, such as:
- Great Stress
- Sadness
- Anger
- Grief
- Lifestyle Changes
can seriously burden the thyroid gland. These episodes can create an enormous nutritional need as the body works to cope with heightened demands. When faced with such stressors, the thyroid may require additional support in the form of nutrients, particularly iodine, selenium, and zinc, which are vital for hormone production and regulation.
The Role of the Thyroid Gland in Energy Production and Metabolism:
The thyroid gland is a critical player in regulating the body’s energy production, affecting nearly every cell. Each cell in the body has receptors for thyroid hormones, which underscores the widespread influence of these hormones on various physiological processes.
Key Functions of Thyroid Hormones
- Energy Production: The primary role of thyroid hormones—primarily thyroxine (T4) and triiodothyronine (T3)—is to control energy production within cells. They act as key regulators of metabolism, influencing how effectively the body converts food into usable energy.
- Cellular Metabolism: By controlling metabolic processes, thyroid hormones dictate how well cells utilize nutrients from the food we consume, including fats, sugars, and proteins. This process is vital for maintaining energy levels and overall health.
- Mitochondrial Function: Thyroid hormones play a crucial role in regulating the function of mitochondria, often referred to as the “powerhouses” of the cell. Mitochondria are responsible for converting nutrients into adenosine triphosphate (ATP), the energy currency of the cell. The amount of energy produced from food largely depends on how effectively mitochondria operate, which is influenced by thyroid hormone levels.
The Importance of the Hypothalamus-Pituitary-Thyroid Axis
The hypothalamus, pituitary gland, and thyroid gland work together in a complex hormonal feedback system known as the hypothalamus-pituitary-thyroid (HPT) axis. This system is crucial for regulating the production and release of thyroid hormones, including triiodothyronine (T3) and thyroxine (T4). However, any issues or dysfunctions within these components can lead to significant hormonal imbalances that affect overall health.
Key Components of the HPT Axis
- Hypothalamus: The hypothalamus is responsible for monitoring the body’s hormonal needs and releasing thyrotropin-releasing hormone (TRH). This hormone stimulates the pituitary gland to produce thyroid-stimulating hormone (TSH).
- Pituitary Gland: This small gland releases TSH in response to TRH from the hypothalamus. TSH then signals the thyroid gland to produce and release T3 and T4.
- Thyroid Gland: The thyroid produces T3 and T4, which regulate metabolism and energy production throughout the body.
Consequences of Dysfunction
If any part of this axis experiences dysfunction, it can lead to imbalances in T3 and T4 levels:
- Hypothalamic Issues: Damage or dysfunction in the hypothalamus can disrupt the release of TRH, leading to inadequate stimulation of the pituitary gland. This can result in low levels of TSH and consequently lower levels of thyroid hormones.
- Pituitary Gland Problems: Disorders affecting the pituitary gland, such as tumors or inflammation, can impair TSH production. This directly affects the thyroid’s ability to produce T3 and T4, potentially leading to hypothyroidism or hyperthyroidism.
- Thyroid Dysfunction: Issues within the thyroid gland itself, such as autoimmune diseases (e.g., Hashimoto’s thyroiditis or Graves’ disease), can alter the production of T3 and T4. This can result in symptoms of thyroid imbalance, such as fatigue, weight changes, mood swings, and metabolic disturbances.
Function of Thyroid Hormones: T4 and T3

Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), play critical roles in regulating various physiological processes throughout the body. Here’s how these hormones function and their significance:
- Release of Thyroid Hormones
Once the thyroid gland releases T4 into the bloodstream, it undergoes a conversion process in certain cells. This process, known as de-iodination, transforms T4 into T3, the more active form of thyroid hormone.
- Active vs. Inactive Form
- T4 (Thyroxine): While T4 is essential for overall thyroid function, it is generally considered the inactive form of thyroid hormone. Although it circulates in higher quantities in the bloodstream, T4 has a limited direct effect on cellular processes.
- T3 (Triiodothyronine): T3 is the active form of thyroid hormone, which is better utilized by cells with thyroid hormone receptors. T3 binds more effectively to these receptors, leading to a more significant impact on metabolism and energy production.
- Physiological Functions
The primary functions of thyroid hormones include:
- Regulation of Metabolism: T3 and T4 play a crucial role in regulating the body’s metabolic rate, influencing how efficiently the body converts food into energy. This affects everything from weight management to energy levels.
- Energy Production: By regulating mitochondrial function, thyroid hormones ensure that cells produce adequate energy (ATP) from the nutrients consumed, including fats, sugars, and proteins.
- Growth and Development: Thyroid hormones are vital for proper growth and development, particularly during childhood and adolescence. They support the development of the brain and other critical bodily systems.
- Heart Function: Thyroid hormones influence heart rate and cardiac output, contributing to overall cardiovascular health.
- Body Temperature Regulation: By controlling metabolism, thyroid hormones help maintain body temperature, ensuring the body remains at a stable temperature despite external changes.
- Mood and Cognitive Function: Adequate levels of T3 and T4 are essential for emotional well-being and cognitive function. Imbalances can lead to mood disorders and cognitive impairment.
Function of Thyroid Hormones: Conversion of T4 to T3:
Thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), are essential for regulating numerous physiological processes in the body. While T4 is released into the bloodstream by the thyroid gland, it is primarily converted into the more active T3 form in various tissues, glands, organs, and body systems. Here’s how this conversion takes place and its significance:
Key Tissues and Organs Involved in the Conversion of T4 to T3:
- Liver: The liver plays a crucial role in metabolizing and converting T4 into T3. It is a significant site for the conversion process, influencing overall thyroid hormone availability in the body.
- Kidneys: The kidneys are involved in the conversion of T4 to T3, ensuring that the body maintains adequate levels of the active hormone.
- Muscles: Muscle tissues can convert T4 to T3, allowing for localized regulation of metabolism and energy production, which is vital for muscle function and physical activity.
- Thyroid Gland: Although the thyroid gland primarily produces T4, it can also convert some T4 into T3, contributing to the overall supply of active thyroid hormone in the bloodstream.
- Pituitary Gland: The pituitary gland can convert T4 to T3, impacting its own function in regulating other hormones, including thyroid-stimulating hormone (TSH).
- Brown Adipose (Fat) Tissue: This specialized fat tissue is crucial for thermogenesis (heat production). Brown adipose tissue can convert T4 to T3, helping to maintain body temperature in cold conditions by generating heat.
- Central Nervous System: The brain and spinal cord can also convert T4 to T3, which is essential for regulating cognitive function, mood, and overall neurological health.
Importance of T3 in the Body
- Metabolic Regulation: T3 is the active form of thyroid hormone that regulates metabolism at the cellular level, influencing how the body utilizes nutrients for energy production.
- Energy Production: By promoting mitochondrial function, T3 ensures that cells can efficiently produce energy (ATP) from the food consumed.
- Development and Growth: T3 is vital for normal growth and development, particularly in the brain and nervous system.
- Thermoregulation: The conversion of T4 to T3 in brown adipose tissue supports thermoregulation, helping to maintain body temperature during exposure to cold.
- Mood and Cognitive Function: Adequate levels of T3 are essential for maintaining emotional well-being and cognitive abilities, as thyroid hormones influence neurotransmitter activity.
Functions of Thyroid Hormones (T3 and T4) in the Body:
Thyroid hormones, primarily triiodothyronine (T3) and thyroxine (T4), have far-reaching effects on nearly every cell and organ in the body. Their influence extends to multiple physiological processes, playing a crucial role in maintaining overall health and well-being. Here are the key functions of thyroid hormones:
- Regulating Metabolic Rate
Thyroid hormones are vital for regulating the metabolic rate, which determines how quickly the body uses calories (energy). This regulation is crucial for weight management, as it influences both weight loss and weight gain. An increase in thyroid hormone levels typically boosts metabolism, while lower levels can slow it down.
- Heart Rate Regulation
Thyroid hormones can influence heart rate by either speeding it up or slowing it down. This effect is essential for maintaining proper cardiovascular function and ensuring that the heart meets the body’s energy demands during various activities.
- Body Temperature Control
T3 and T4 play a significant role in regulating body temperature. They can raise or lower body temperature based on the body’s metabolic needs. Increased levels of thyroid hormones generally lead to a rise in body temperature, while lower levels may result in a decrease.
- Digestive Function
Thyroid hormones influence the speed at which food moves through the digestive tract. They can enhance the efficiency of digestion and nutrient absorption, affecting overall digestive health and metabolic processes.
- Brain Development
T3 and T4 are critical for brain development, particularly during prenatal and early postnatal stages. Adequate thyroid hormone levels are essential for proper neurological growth and function, influencing cognitive abilities and emotional health throughout life.
- Muscle Function
Thyroid hormones control the way muscles contract, affecting muscle strength and performance. This influence is vital for physical activity, exercise, and overall muscle health.
- Skin and Bone Maintenance
Thyroid hormones help manage skin and bone maintenance by regulating the rate at which the body replaces dying cells—a normal biological process. Adequate thyroid hormone levels ensure that tissues remain healthy, promoting skin elasticity and bone density.
Functions of Thyroid Hormones:
Thyroid hormones, primarily triiodothyronine (T3) and thyroxine (T4), are vital regulators of various physiological processes throughout the body. Their functions encompass a wide range of systems and activities, impacting overall health and well-being. Here’s a closer look at the key functions of thyroid hormones:
- Regulator of Metabolism
Thyroid hormones are fundamental in regulating metabolism, affecting every part of the body from the neck down. They play a crucial role in determining how efficiently the body uses energy, influencing overall metabolic rates and energy expenditure.
- Circulation
Thyroid hormones significantly impact circulation, and imbalances can lead to common symptoms such as cold hands and feet. Proper thyroid function ensures optimal blood flow and circulation, which is essential for maintaining body temperature and delivering nutrients to tissues.
- Sexual Function
Thyroid hormones influence sexual health and reproductive functions. Low levels can lead to symptoms such as:
- Decreased libido
- Hormonal imbalances
- Menstrual complaints
- Infertility
- Sexual dysfunction
These effects can create challenges for both men and women in achieving optimal reproductive health.
- Energy Regulation
Thyroid hormones are crucial for maintaining energy levels. Low thyroid hormone levels can result in fatigue, low energy, and a poor attitude, affecting daily functioning and overall quality of life.
- Weight Management

The resting metabolic rate is heavily influenced by thyroid hormone levels. If thyroid function is low, it can lead to a reduced metabolic rate, resulting in weight gain despite normal eating habits. This connection makes thyroid health an important factor in weight management.
- Muscle Development
Thyroid hormones are necessary for muscle development and performance. They support athletic performance by promoting lean muscle mass, making them essential for bodybuilders and athletes looking to enhance their physical strength and endurance.
- Immune Function
Thyroid hormones play a role in immune function, influencing how the body responds to infections and allergens. An imbalance can lead to an overreactive or underreactive immune system, potentially resulting in allergies or autoimmune diseases.
- Excretory Function
Thyroid hormones also contribute to the excretory system by facilitating the removal of waste products from the body. Proper thyroid function supports healthy kidney and liver activity, ensuring efficient waste elimination.
Responsibilities of the Thyroid Gland and Symptoms of Malfunction
The thyroid gland plays a crucial role in maintaining overall health by regulating various bodily functions through the production of thyroid hormones (primarily T3 and T4). When the thyroid malfunctions, it can lead to a wide array of symptoms that impact different systems in the body. Here’s a detailed look at the responsibilities of the thyroid gland and the symptoms associated with its dysfunction:
Responsibilities of the Thyroid Gland:
- Hormonal Regulation: The thyroid gland produces hormones that regulate metabolism, growth, and development. It influences the production of other hormones in the body, ensuring hormonal balance.
- Metabolic Control: It regulates the body’s metabolic rate, affecting how efficiently energy is used and stored.
- Temperature Regulation: Thyroid hormones help maintain normal body temperature by controlling metabolic activity.
- Cardiovascular Health: The thyroid influences heart rate and blood pressure, contributing to overall cardiovascular function.
- Mental Health: Thyroid hormones are essential for cognitive function and emotional well-being, influencing mood and mental clarity.
Symptoms of Thyroid Malfunction
- Hormonal Imbalance: A malfunctioning thyroid can lead to reduced production of all hormones, resulting in widespread hormonal imbalances that affect various bodily functions.
- Hair Changes: Individuals may experience hair loss, including more severe forms such as alopecia. This can occur due to the thyroid’s role in regulating hair follicle health.
- Skin Issues: Common skin symptoms include:
- Dark circles under the eyes
- Dry skin
- Acne outbreaks
- Darker spots on the skin
These symptoms reflect the thyroid’s influence on skin metabolism and hydration.
- Cognitive Effects: Malfunctioning thyroid glands can lead to cognitive issues, including:
- Mental sluggishness
- Poor memory
- Insomnia
- Depression
- Lack of focus
- Poor concentration
These symptoms indicate the significant impact of thyroid hormones on brain health and function.
- Vascular Symptoms: Thyroid dysfunction can cause fluctuations in blood pressure, leading to symptoms of both high and low blood pressure. Additionally, circulation issues may arise, affecting overall cardiovascular health.
- Fluid Retention: An underactive thyroid (hypothyroidism) can lead to fluid retention, resulting in swelling and bloating. This symptom reflects the thyroid’s role in regulating fluid balance in the body.
Diagnosis of Thyroid Disease:
Diagnosing thyroid disease typically involves a comprehensive evaluation that includes clinical assessments and laboratory tests. This process helps identify various thyroid disorders, such as hypothyroidism (underactive thyroid), hyperthyroidism (overactive thyroid), and other related conditions. Here’s a detailed overview of the diagnostic steps:
- Clinical Evaluation
Medical History
A thorough medical history is crucial for understanding the patient’s symptoms and risk factors associated with thyroid disorders. Physicians often inquire about:
- Symptoms: Patients may be asked about specific symptoms such as:
- Fatigue
- Weight changes (gain or loss)
- Heat or cold intolerance
- Hair loss or changes in hair texture
- Alterations in heart rate (palpitations or bradycardia)
- Menstrual irregularities (changes in cycle or flow)
- Family History: Any history of thyroid disease or autoimmune disorders in the family may be relevant, as these conditions can be hereditary.
Physical Examination
During a physical examination, healthcare providers assess various aspects related to thyroid function:
- Thyroid Size and Texture: The physician checks for an enlarged thyroid (goiter) or nodules by palpating the thyroid gland, which is located at the base of the neck.
- Skin and Hair Condition: Observations of skin texture (dryness or moisture), hair thinning, or changes can provide clues to thyroid health.
- Reflexes: The doctor may check reflexes to evaluate neurological function, as thyroid disorders can impact the nervous system.
- Heart Rate and Blood Pressure: Vital signs, including heart rate and blood pressure, are monitored, as thyroid function significantly affects cardiovascular health.
Neck Examination
A focused neck examination is crucial for identifying any abnormalities in the thyroid gland. The physician will palpate the gland to:
- Assess Size: Determine if the thyroid is enlarged (goiter) or if there are any noticeable nodules or irregularities.
- Check for Pain: Assess if there is any tenderness or discomfort in the thyroid area, which could indicate inflammation or other issues.
- Laboratory Tests
Following the clinical evaluation, laboratory tests are typically performed to assess thyroid function more objectively. Common tests include:

- Thyroid-Stimulating Hormone (TSH) Test: This test measures the level of TSH in the blood, which is produced by the pituitary gland to regulate thyroid hormone production. Abnormal TSH levels can indicate hypothyroidism (high TSH) or hyperthyroidism (low TSH).
- Free T4 and Free T3 Tests: These tests measure the levels of the active thyroid hormones (T4 and T3) in the bloodstream. Low levels of T4 and T3 can indicate hypothyroidism, while elevated levels may suggest hyperthyroidism.
- Thyroid Antibodies Tests: If autoimmune thyroid disease is suspected, tests for specific antibodies (such as anti-thyroid peroxidase and anti-thyroglobulin antibodies) may be conducted to determine if the immune system is attacking the thyroid.
- Thyroid Ultrasound: In cases where nodules or abnormalities are detected, a thyroid ultrasound may be performed to assess the structure of the thyroid gland and identify any cysts, solid masses, or other concerns.
- Radioactive Iodine Uptake Test: This test evaluates how well the thyroid takes up iodine, which is essential for hormone production. It helps determine if the thyroid is overactive or underactive.
Tests to Measure Thyroid Levels:
To assess thyroid function and determine how well the thyroid gland is working, several blood tests are commonly referred to as thyroid function tests. These tests measure the levels of various thyroid hormones and related substances in the bloodstream. Here’s a breakdown of the primary tests used to evaluate thyroid levels:
- Total T4 (Thyroxine) Test: The Total T4 test measures the overall level of thyroxine (T4) hormone in the blood, including both bound and free forms. T4 is produced by the thyroid gland and is crucial for regulating metabolism. Elevated levels may indicate hyperthyroidism, while low levels can suggest hypothyroidism.
- Free T4 (FT4) Test: The Free T4 test measures the unbound or free form of thyroxine in the blood. This is the active form that can enter cells and exert effects on metabolism. The FT4 test provides a more accurate assessment of thyroid function, as it is less affected by proteins in the blood that can bind to T4.
- Total T3 (Triiodothyronine) Test: The Total T3 test measures the total level of triiodothyronine (T3) hormone in the blood, including both bound and free forms. T3 is the most active thyroid hormone and is essential for regulating metabolism. Elevated Total T3 levels may indicate hyperthyroidism, while low levels can be associated with hypothyroidism.
- Free T3 (FT3) Test: The Free T3 test measures the unbound or free form of triiodothyronine in the blood. This test is important for evaluating thyroid function, especially in cases where symptoms of hyperthyroidism are present, even when TSH levels may be normal.
- Thyroid-Stimulating Hormone (TSH) Test: The TSH test measures the level of thyroid-stimulating hormone in the blood. TSH is produced by the pituitary gland and stimulates the thyroid gland to produce T4 and T3. A high TSH level usually indicates hypothyroidism, while a low TSH level can suggest hyperthyroidism.
- Thyroid Antibodies Tests: Although not directly measuring thyroid levels, tests for thyroid antibodies (such as anti-thyroid peroxidase and anti-thyroglobulin antibodies) can help confirm a diagnosis of autoimmune thyroid disorders, such as Hashimoto’s thyroiditis or Graves’ disease. The presence of these antibodies indicates that the immune system may be attacking the thyroid gland.
Additional Tests to Assess Thyroid Function
In addition to the standard thyroid function tests, several other assessments can provide valuable insights into thyroid health and help diagnose specific conditions. These tests include:
- Thyroid Antibodies Tests
Thyroid antibody tests measure the presence of specific antibodies in the blood that indicate autoimmune thyroid conditions. These tests are essential for identifying various thyroid disorders, including:
- Anti-Thyroid Peroxidase (Anti-TPO) Antibodies: Elevated levels of these antibodies are often found in individuals with Hashimoto’s thyroiditis, an autoimmune condition that can lead to hypothyroidism.
- Anti-Thyroglobulin Antibodies: The presence of these antibodies may also indicate autoimmune thyroid disease and can be associated with Hashimoto’s thyroiditis.
- TSH Receptor Antibodies: These antibodies are often elevated in Graves’ disease, an autoimmune disorder that causes hyperthyroidism.
- Thyroglobulin Test

The thyroglobulin test measures the level of thyroglobulin, a protein produced by the thyroid gland. This test has two primary uses:
- Diagnosis of Thyroiditis: Elevated thyroglobulin levels can indicate thyroid inflammation (thyroiditis), which can occur in various conditions, including autoimmune diseases and infections.
- Monitoring Thyroid Cancer Treatment: After the surgical removal of the thyroid gland due to cancer, thyroglobulin levels are monitored. Rising levels of thyroglobulin may suggest residual thyroid tissue or cancer recurrence, making it an important marker in managing thyroid cancer patients.
Diagnosis of Thyroid Disease
Early diagnosis and effective treatment of thyroid disease primarily rely on blood tests to evaluate thyroid function. These tests help identify various thyroid disorders, including hypothyroidism and hyperthyroidism. Here’s an overview of how thyroid disease is diagnosed, focusing on the significance of Thyroid Stimulating Hormone (TSH) and other thyroid hormone tests.
- TSH (Thyroid Stimulating Hormone) Test
The TSH test is a fundamental component of thyroid function evaluation. TSH is produced by the pituitary gland and regulates the production of thyroid hormones (T3 and T4) by the thyroid gland. Understanding the results of the TSH test is crucial for diagnosing thyroid conditions.
Interpreting TSH Results
- High TSH Levels:
- A high TSH result may indicate:
- Hypothyroidism: This condition occurs when the thyroid gland is underactive and fails to produce adequate thyroid hormones. As a result, the pituitary gland increases TSH production to stimulate the thyroid.
- Pituitary Gland Issues: A problem with the pituitary gland could lead to excess TSH production.
- Insufficient Thyroid Hormone Medication: If a patient on thyroid hormone replacement therapy has high TSH levels, it may suggest that the dosage is too low.
- Low TSH Levels:
- A low TSH result may indicate:
- Hyperthyroidism: This condition arises when the thyroid gland is overactive and produces excessive thyroid hormones, leading to suppressed TSH levels.
- Pituitary Gland Problems: Similar to high levels, a low TSH could indicate an issue with the pituitary gland.
- Excessive Thyroid Hormone Medication: Patients receiving too much thyroid hormone therapy may show low TSH levels.
The Feedback Loop
Understanding the relationship between TSH and thyroid hormones is vital:
- Thyroid Hormone Production: When thyroid hormone production falls (due to hypothyroidism), TSH levels rise. Conversely, when thyroid hormone levels become too high (as in hyperthyroidism), TSH levels fall.
- Thyroid Function Tests: T3 and T4
In addition to the TSH test, measuring the levels of thyroid hormones (T3 and T4) provides a comprehensive evaluation of thyroid function:
- Total T4 (Thyroxine) Test: Measures the total amount of T4 in the blood, including both bound and free forms. Low levels indicate hypothyroidism, while high levels suggest hyperthyroidism.
- Free T4 (FT4) Test: This test measures the unbound, active form of T4. It provides a more accurate reflection of thyroid function, as it is less affected by proteins that bind thyroid hormones.
- Total T3 (Triiodothyronine) Test: Measures the total level of T3, which is the most active thyroid hormone. Elevated T3 levels can indicate hyperthyroidism, while low levels may suggest hypothyroidism.
- Free T3 (FT3) Test: This test measures the unbound, active form of T3. It is particularly useful in diagnosing hyperthyroidism and assessing the effectiveness of treatment.
Patterns of Thyroid Function Test Results:
1. Normal TSH, Normal FT4, Normal FT3:
- This result indicates normal thyroid function. All hormone levels are within the expected ranges, meaning the thyroid is functioning properly.
2. High TSH, Normal FT4, Normal FT3:
- This pattern may suggest mild or sub-clinical hypothyroidism, where the thyroid gland is underactive but still producing normal amounts of T4 and T3. It can also indicate an acute illness affecting the body.
3. High TSH, Low FT4, Normal or Low FT3:
- This result indicates an underactive thyroid (hypothyroidism). The thyroid is not producing enough hormones (low FT4), leading to elevated TSH levels as the pituitary gland tries to stimulate the thyroid to produce more hormones.
4. Low TSH, Normal FT4, Normal FT3:
- This finding may indicate mild or sub-clinical hyperthyroidism. Although TSH is low, the thyroid hormone levels (FT4 and FT3) remain within normal ranges.
5. Low TSH, High FT4 or High FT3:
- This result suggests overt hyperthyroidism, where the thyroid gland is producing excessive amounts of thyroid hormones. The low TSH indicates that the pituitary gland is reducing its stimulation of the thyroid due to high hormone levels.
6. Low TSH, Low FT4, Low FT3:
- This pattern could indicate hypothyroidism resulting from an issue with the pituitary gland or hypothalamus that controls the thyroid gland. Both thyroid hormones are low, and the body is not receiving adequate stimulation from TSH.
Thyroid Antibodies:
Thyroid antibody tests are essential diagnostic tools used to identify various antibodies that can affect thyroid function and indicate specific thyroid conditions. Here’s a detailed look at the key types of thyroid antibodies and their implications:
1. Thyroid Peroxidase Antibodies (TPOAb):
- Function: TPOAb targets the enzyme thyroid peroxidase, which is crucial for the synthesis of thyroid hormones.
- Significance: Elevated levels of TPOAb are commonly associated with Hashimoto’s disease, an autoimmune disorder that leads to hypothyroidism. In this condition, the immune system mistakenly attacks the thyroid gland, resulting in inflammation and reduced hormone production.
2. Thyroglobulin Antibodies (TgAb):
- Function: TgAb targets thyroglobulin, a protein produced by the thyroid gland that is a precursor to thyroid hormones.
- Significance: High levels of TgAb are also indicative of Hashimoto’s disease. Like TPOAb, the presence of TgAb suggests that the immune system is involved in damaging the thyroid, potentially leading to hypothyroidism.
3. Thyrotropin Receptor Antibodies (TRAb):
- Function: TRAb interacts with the thyroid-stimulating hormone (TSH) receptor on the thyroid gland, which regulates thyroid hormone production.
- Significance: Elevated TRAb levels are often associated with Graves’ disease, another autoimmune condition characterized by hyperthyroidism. In this case, the antibodies stimulate the thyroid to produce excess hormones, leading to symptoms of hyperthyroidism.
Thyroglobulin
The thyroglobulin test measures the level of thyroglobulin, a protein produced by the thyroid gland. It serves two primary purposes in managing thyroid-related conditions:
- Monitoring Thyroid Cancer Treatment: The thyroglobulin test is particularly useful for patients who have been diagnosed with thyroid cancer. After treatment, particularly following thyroidectomy (surgical removal of the thyroid gland), regular monitoring of thyroglobulin levels can help assess how well the treatment is working.
- Detecting Recurrence: Elevated thyroglobulin levels in patients previously treated for thyroid cancer may indicate a recurrence of the disease. By tracking these levels over time, healthcare providers can identify any signs of cancer returning, allowing for timely intervention.
Non-Laboratory Tests
In addition to blood tests, non-laboratory tests are valuable tools for diagnosing and evaluating thyroid conditions. Here are two common non-laboratory tests:
1. Thyroid Scans:
- Purpose: This specialized imaging procedure is used to visualize the thyroid gland and identify abnormalities. It helps evaluate thyroid function and can pinpoint areas of overactivity (hyperfunctioning) or underactivity (hypofunctioning) within the thyroid.
- How it Works: A small amount of radioactive material is administered, and a gamma camera captures images of the thyroid gland. This scan can reveal nodules, goiters, or other issues affecting thyroid function.
2. Ultrasound:
- Purpose: Ultrasound is an imaging technique used to examine the thyroid for various abnormalities, including cysts, nodules, or tumors. It is non-invasive and does not involve radiation.
- How it Works: High-frequency sound waves are used to create images of the thyroid gland. Ultrasound can help assess the size, shape, and characteristics of any nodules or other structures, guiding further evaluation and management.
Calcitonin:
The calcitonin test measures the level of calcitonin, a hormone produced by the parafollicular cells (C cells) of the thyroid gland. This test is particularly significant in the context of thyroid health for the following reasons:
- Medullary Thyroid Cancer Detection: Elevated levels of calcitonin can be indicative of medullary thyroid cancer (MTC), a rare type of thyroid cancer that arises from the C cells. Since calcitonin is secreted by these cells, measuring its levels can help in diagnosing this specific cancer type.
- Monitoring Treatment and Recurrence: For patients diagnosed with medullary thyroid cancer, regular calcitonin testing can help monitor treatment effectiveness and detect any potential recurrence of the disease. Elevated calcitonin levels after treatment may suggest that cancer is still present or has returned.
Imaging Tests for Thyroid Evaluation:
Several imaging tests are essential in diagnosing and evaluating thyroid conditions. Here’s a detailed overview of the primary imaging tests used in thyroid assessment:
1. Thyroid Ultrasound:
- Purpose: This test employs sound waves to produce detailed images of the thyroid gland. It is particularly effective in identifying various abnormalities.
- What It Detects: Ultrasound can help visualize nodules, cysts, and goiters, allowing healthcare providers to assess the size, shape, and composition of these structures. It is a non-invasive and painless procedure that helps in making informed decisions about further evaluation or treatment.
2. Thyroid Scan:
- Purpose: This imaging test involves administering a small amount of radioactive iodine or technetium to create a visual representation of the thyroid gland.
- What It Assesses: A thyroid scan is instrumental in evaluating the function of thyroid nodules or detecting areas of hyperactive thyroid tissue. It helps distinguish between functioning (hot) nodules, which produce hormones, and non-functioning (cold) nodules, which do not.
3. Radioactive Iodine Uptake Test (RAIU):
- Purpose: The RAIU test measures how much radioactive iodine the thyroid absorbs over a specified period.
- What It Diagnoses: This test is crucial for diagnosing hyperthyroidism. A high uptake of radioactive iodine indicates an overactive thyroid, while low uptake may suggest hypothyroidism or other thyroid disorders.
4. Fine Needle Aspiration Biopsy (FNAB):
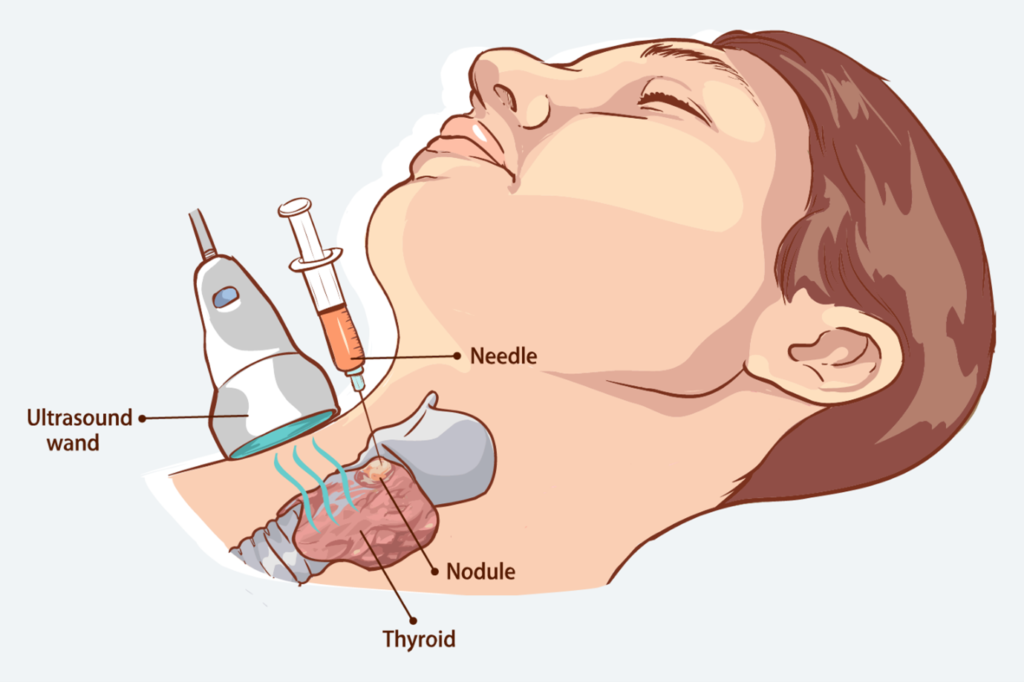
- Purpose: This procedure is performed when a nodule or mass is identified on the thyroid gland through ultrasound or physical examination.
- What It Determines: FNAB involves using a thin needle to extract tissue or fluid from the nodule. The collected sample is then examined under a microscope to determine whether the nodule is benign or malignant. This biopsy is a minimally invasive technique that helps guide treatment decisions.
Thyroid Self-Test: A Simple Guide to Checking Your Thyroid Health
Step 1: Identify the Thyroid Gland’s Location Begin by focusing on the area of your neck just below the Adam’s apple and immediately above the collarbone. This is where your thyroid gland is located.
Step 2: Use a Mirror and Adjust Your Head While concentrating on this area of your neck in the mirror, tilt your head slightly back. This position helps you see the gland more clearly.
Step 3: Take a Sip of Water Now, while your head is tilted back, take a sip of water and get ready to observe the movement of your neck.
Step 4: Observe for Any Unusual Bulges or Protrusions As you swallow the water, closely watch your neck in the mirror. Check for any noticeable bulges, lumps, or protrusions in the thyroid region. These could be signs of thyroid inflammation or nodules.
Step 5: Consult a Doctor if Needed If you spot any bulges or protrusions while swallowing, it’s crucial to consult with your healthcare provider immediately. Thyroid nodules and inflammation can sometimes be linked to thyroid disorders and may cause difficulties in swallowing.
Why Is This Important?
Thyroid problems, such as inflammation or nodules, can sometimes manifest as swelling or lumps in the neck. Early detection through a self-test like this can help in identifying potential thyroid issues that may require medical attention. Regular monitoring of your thyroid health can contribute to overall well-being.
Always remember to follow up with a healthcare professional if you notice any irregularities during the self-test.
Additional Evaluations for Thyroid Health
While the thyroid self-test is a simple and helpful way to check for potential issues with your thyroid, there are other important evaluations that can provide a more comprehensive picture of thyroid function. Here are two commonly used tests:
- Basal Body Temperature Test
One way to assess thyroid function, particularly hypothyroidism (an underactive thyroid), is by measuring basal body temperature. Hypothyroidism is often associated with a consistently lower body temperature. To conduct this test:
- Measure your body temperature immediately after waking up, before getting out of bed or starting any activity.
- A temperature consistently below the normal range of 97.8°F (36.5°C) could indicate hypothyroidism.
This method, although not a definitive diagnostic tool, can provide clues about your thyroid health, especially when used alongside other evaluations.
- Cholesterol and Lipid Profile
Thyroid dysfunction can have a significant impact on lipid metabolism. Both hypothyroidism and hyperthyroidism (overactive thyroid) can alter cholesterol and triglyceride levels in the blood. For example:
- Hypothyroidism often leads to higher cholesterol levels due to slower metabolism.
- Hyperthyroidism may lower cholesterol levels due to an increased metabolic rate.
As a result, a comprehensive lipid profile, which measures cholesterol (total, LDL, HDL) and triglycerides, may be performed to help evaluate thyroid function. Abnormal results, especially in the context of other thyroid symptoms, can guide doctors toward a more accurate diagnosis.
Why These Tests Matter
Both basal body temperature and lipid profiles offer valuable insights into how your thyroid is functioning. When combined with a thyroid self-test, these evaluations can help in detecting thyroid imbalances early, allowing for timely intervention and management of thyroid-related diseases. Consulting with a healthcare provider to discuss these tests can aid in creating a well-rounded approach to your thyroid health.
Conditions Related to Abnormal Thyroid Hormone Levels
The thyroid gland plays a critical role in regulating metabolism, energy production, and many bodily functions. When thyroid hormone levels become imbalanced, it can lead to a range of health conditions, many of which require medical attention. Below are some of the most common thyroid-related conditions:
- Hypothyroidism (Underactive Thyroid)
Hypothyroidism occurs when the thyroid gland produces insufficient thyroid hormones. This can slow down metabolism and lead to symptoms such as fatigue, weight gain, dry skin, cold intolerance, and depression. It is often diagnosed through blood tests showing low levels of thyroid hormones (T3, T4) and elevated thyroid-stimulating hormone (TSH). - Hashimoto’s Disease
Hashimoto’s disease is an autoimmune disorder in which the immune system attacks the thyroid gland, leading to hypothyroidism. Over time, the thyroid becomes damaged and produces less of the hormones needed for normal bodily functions. Symptoms are similar to those of hypothyroidism and may include goiter (thyroid enlargement). - Hyperthyroidism (Overactive Thyroid)
Hyperthyroidism occurs when the thyroid gland produces excessive thyroid hormones, accelerating the body’s metabolism. Symptoms include rapid weight loss, anxiety, rapid heartbeat, sweating, and irritability. Blood tests show elevated levels of thyroid hormones and suppressed TSH levels. - Graves’ Disease
Graves’ disease is another autoimmune condition, but in this case, it causes hyperthyroidism. The immune system produces antibodies that overstimulate the thyroid, leading to an overproduction of thyroid hormones. Patients may also experience eye-related symptoms like bulging eyes (Graves’ ophthalmopathy). - Thyroiditis (Thyroid Inflammation)
Thyroiditis refers to inflammation of the thyroid gland. This condition can lead to temporary hyperthyroidism followed by hypothyroidism as the inflammation damages the thyroid. Thyroiditis can be caused by infections, autoimmune diseases, or certain medications. - Thyroid Nodules
Thyroid nodules are small lumps or growths that develop in the thyroid gland. Most nodules are benign (non-cancerous), but some may produce excess thyroid hormones, causing hyperthyroidism. In rare cases, thyroid nodules can be cancerous, so medical evaluation is important. - Goiter (Enlarged Thyroid Gland)
Goiter refers to the abnormal enlargement of the thyroid gland. It can be associated with both hypothyroidism and hyperthyroidism. Goiters may be caused by iodine deficiency, autoimmune diseases like Hashimoto’s or Graves’ disease, or other thyroid disorders. - Thyroid Cancer
Thyroid cancer occurs when abnormal cells in the thyroid grow uncontrollably. The condition is generally diagnosed through biopsies of suspicious thyroid nodules. While it is less common compared to other thyroid conditions, early detection is key to effective treatment.
Managing Thyroid Conditions
The treatment for thyroid-related conditions depends on the underlying cause. Medications, hormone replacement therapies, and, in some cases, surgery may be recommended. Regular monitoring of thyroid hormone levels is essential to ensure proper management of these conditions and maintain overall health.
Common Causes of Thyroid Disorders
Thyroid disorders can arise due to various factors that affect the gland’s ability to function properly. These causes can lead to either an underactive (hypothyroidism) or overactive (hyperthyroidism) thyroid. Here are some of the most common causes of thyroid problems:
- Autoimmune Disorders
Autoimmune diseases are among the leading causes of thyroid dysfunction. In these conditions, the immune system mistakenly attacks the thyroid gland, either reducing or enhancing its hormone production.
- Hashimoto’s Thyroiditis: This autoimmune condition is the most common cause of hypothyroidism. The immune system attacks and damages the thyroid gland, resulting in decreased hormone production.
- Graves’ Disease: This autoimmune disorder is the leading cause of hyperthyroidism. In Graves’ disease, the immune system stimulates the thyroid gland to produce excessive thyroid hormones, speeding up metabolism.
- Iodine Deficiency or Excess
Iodine is a critical element that the thyroid gland uses to produce thyroid hormones. Imbalances in iodine levels can severely affect thyroid function.
- Iodine Deficiency: When there is insufficient iodine in the diet, the thyroid cannot produce enough hormones, leading to hypothyroidism. A lack of iodine can also cause goiter, an enlargement of the thyroid gland.
- Excessive Iodine Intake: Consuming too much iodine, whether through diet or supplements, can disrupt the balance of thyroid hormones. It may lead to either hypothyroidism or hyperthyroidism, depending on how the thyroid reacts.
- Thyroid Inflammation (Thyroiditis)

Inflammation of the thyroid, known as thyroiditis, can cause temporary or long-term thyroid dysfunction. Several factors can trigger thyroiditis:
- Viral or Bacterial Infections: Infections can cause acute or subacute thyroiditis, leading to temporary hyperthyroidism or hypothyroidism as the thyroid recovers from inflammation.
- Postpartum Thyroiditis: This condition occurs in some women after giving birth. It may initially cause hyperthyroidism, followed by hypothyroidism as the thyroid heals from the inflammation.
Other Contributing Factors
In addition to the above causes, other factors can also affect thyroid function, including:
- Radiation exposure: Radiation treatment to the neck area or exposure to environmental radiation can damage the thyroid gland, potentially leading to hypothyroidism or, in rare cases, thyroid cancer.
- Medications: Certain medications, such as lithium or amiodarone, can interfere with thyroid hormone production, leading to thyroid dysfunction.
- Genetics: A family history of thyroid problems increases the likelihood of developing a thyroid condition.
Understanding Types of Thyroid Diseases
Hypothyroidism
- Definition: Hypothyroidism occurs when the thyroid gland does not produce enough thyroid hormones. This deficiency can lead to a slowdown in the body’s metabolic processes.
- Common Causes: The most frequent cause of hypothyroidism is Hashimoto’s Thyroiditis, an autoimmune condition where the immune system attacks the thyroid gland, leading to decreased hormone production.
- Common Symptoms:
- Dry Skin: The skin may become rough and dry due to reduced metabolic activity.
- Weight Gain: Individuals may experience unexplained weight gain due to a slowed metabolism.
- Sensitivity to Cold: People with hypothyroidism often feel cold more easily than others because their bodies aren’t producing enough heat.
- Impaired Cognition: This can manifest as memory problems, difficulty concentrating, or feelings of depression.
Hyperthyroidism
- Definition: Hyperthyroidism occurs when the thyroid gland produces hormones in excessive amounts, leading to an accelerated metabolism.
- Common Causes: The most common cause of hyperthyroidism is Graves’ Disease, another autoimmune disorder where antibodies stimulate the thyroid to produce too much hormone.
- Common Symptoms:
- Bouts of Nervousness: Individuals may experience increased anxiety or restlessness.
- Weight Loss: Unexplained weight loss is common due to the heightened metabolic rate.
- Sensitivity to Heat: Those with hyperthyroidism often feel hot and may sweat more than usual.
- Increased Heart Rate: Palpitations or a racing heart are frequent symptoms of hyperthyroidism.
Hypothyroidism vs. Hyperthyroidism Symptoms
Hypothyroidism Symptoms
Hypothyroidism occurs when the thyroid gland does not produce enough thyroid hormones, leading to a variety of physical and mental symptoms:
- Cold Intolerance: Individuals often feel unusually cold due to a slowed metabolism.
- Decreased Sweating: Reduced hormone levels can lead to less perspiration.
- Depression and Irritability: Mental health can be affected, leading to mood changes.
- Weight Gain: A slower metabolism often results in weight increase.
- Constipation: Slowed bodily functions can affect digestion.
- Irregular and Heavy Periods: Hormonal imbalances may lead to menstrual irregularities.
- Slow Heart Rate: Lower thyroid hormone levels can reduce heart rate.
- Brittle Nails: Nails may become weak and break easily.
- Puffy Face: Fluid retention can lead to facial puffiness.
- Muscle or Joint Pain: Discomfort and pain may occur in muscles or joints.
Common Symptoms:
Both conditions can exhibit overlapping symptoms, which include:
- Fatigue: Persistent tiredness is common in both disorders.
- Insomnia: Difficulty sleeping can be a symptom in both conditions.
- Hair Loss: Thinning hair can occur in both hypothyroidism and hyperthyroidism.
Hyperthyroidism Symptoms:
Hyperthyroidism is characterized by an overproduction of thyroid hormones, leading to symptoms that indicate an accelerated metabolism:
- Weight Loss or Gain: Weight fluctuations are common, with many experiencing weight loss.
- Increased Sweating: Excess hormone levels can lead to heightened perspiration.
- Nervousness and Anxiety: Psychological effects may include heightened anxiety levels.
- Short and Light Periods: Menstrual cycles may become shorter and lighter.
- Puffy or Bulging Eyes: Some individuals experience eye changes, particularly in Graves’ disease.
- Racing Heart: An increased heart rate is typical due to elevated hormone levels.
- Heat Intolerance: Individuals may feel excessively warm or overheated.
- Nail Thickening and Flaking: Changes in nails may occur, becoming thicker or flaking.
- Muscle Weakness: Weakness in muscles can be a common complaint.
- Diarrhea: Increased bowel movements or diarrhea can result from the overactive metabolism.
Understanding Thyroid Cancer: Common Symptoms and Anatomy
Thyroid cancer is a type of cancer that develops in the thyroid gland, a butterfly-shaped gland located at the base of your neck, just below the Adam’s apple. The thyroid gland produces hormones that regulate your heart rate, blood pressure, body temperature, and weight. Recognizing the symptoms of thyroid cancer early can lead to better outcomes and more effective treatments.
Common Symptoms of Thyroid Cancer
The image provides a visual representation of the common symptoms associated with thyroid cancer. Here’s a detailed explanation of each symptom:
1. Thyroid Nodule
- Description: A thyroid nodule is a lump that can develop in the thyroid gland. While many thyroid nodules are benign, some can be cancerous.
- Signs: A noticeable lump or swelling in the neck.
2. Swollen Lymph Nodes
- Description: Lymph nodes are part of the body’s immune system and can become swollen when fighting infection or in response to cancer.
- Signs: Swelling or lumps in the neck area, particularly around the lymph nodes.
3. Pain in Front of Neck
- Description: Pain or discomfort in the front part of the neck can be a symptom of thyroid cancer.
- Signs: Persistent or recurring pain in the neck that does not subside.
4. Difficulty Swallowing
- Description: As thyroid cancer progresses, it can interfere with the ability to swallow.
- Signs: A feeling of food getting stuck in the throat or difficulty in swallowing food and liquids.
5. Difficulty Breathing
- Description: Enlarged thyroid nodules or tumors can press against the windpipe (trachea), leading to breathing difficulties.
- Signs: Shortness of breath or a wheezing sound when breathing.
6. Persistent Cough
- Description: A cough that does not go away can be a symptom of thyroid cancer, particularly if it is not related to a cold or other respiratory infection.
- Signs: A chronic cough that persists without any apparent reason.
Anatomy of the Thyroid Gland
Understanding the anatomy of the thyroid gland can help in comprehending how thyroid cancer develops and affects the body:
- Thyroid Cartilage: The thyroid cartilage, located above the thyroid gland, forms the front wall of the larynx and provides protection to the vocal cords.
- Thyroid Gland: This gland produces hormones that regulate various body functions. It is situated in the front of the neck and consists of two lobes connected by an isthmus.
- Trachea: Also known as the windpipe, the trachea is located just below the thyroid gland and is responsible for carrying air to and from the lungs.
- Nodule: A nodule is a growth or lump that can form within the thyroid gland. While most nodules are benign, some can be malignant, indicating thyroid cancer.
Causes of Hyperthyroidism:

Hyperthyroidism is a condition characterized by the overproduction of thyroid hormones, leading to an accelerated metabolism and various symptoms. Several underlying conditions can cause hyperthyroidism, each with distinct mechanisms. Here are the primary causes:
- Graves’ Disease
Graves’ disease is the most prevalent cause of hyperthyroidism. This autoimmune disorder occurs when the body’s immune system mistakenly attacks the thyroid gland. The immune system produces antibodies that stimulate the thyroid to produce excess hormones, particularly thyroxine (T4). As a result, individuals may experience symptoms such as rapid heartbeat, weight loss, and increased sweating.
- Thyroid Nodules
Thyroid nodules are abnormal growths or lumps that can develop on or within the thyroid gland. In some cases, these nodules can become overactive and produce thyroid hormones independently, leading to a condition known as toxic nodular goiter or multinodular goiter. These nodules can cause the overall hormone production of the thyroid to increase, resulting in hyperthyroidism.
- Pituitary Adenoma
A pituitary adenoma is a benign tumor of the pituitary gland that can lead to the overstimulation of the thyroid gland. This occurs because the pituitary gland produces thyroid-stimulating hormone (TSH), which signals the thyroid to produce more hormones. If the adenoma secretes excess TSH, it can cause the thyroid gland to become hyperactive, leading to hyperthyroidism.
- Subacute Thyroiditis
Subacute thyroiditis is a temporary inflammatory condition of the thyroid gland, often following a viral infection. This inflammation can cause the thyroid to release increased amounts of hormones into the bloodstream, leading to temporary hyperthyroidism. Symptoms may include pain in the neck, fatigue, and fever, but they often resolve on their own as the inflammation subsides.
Causes of Hypothyroidism
Hypothyroidism, or an underactive thyroid, is a condition where the thyroid gland does not produce enough thyroid hormones, leading to a variety of metabolic and physiological issues. Several underlying conditions and factors can contribute to the development of hypothyroidism. Here are the primary causes:
- Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is the most common cause of hypothyroidism. This autoimmune disorder occurs when the body’s immune system mistakenly attacks the thyroid gland, gradually destroying its ability to produce hormones. This leads to a deficiency in thyroid hormone levels, resulting in symptoms such as fatigue, weight gain, and sensitivity to cold.
- Postpartum Thyroiditis
Postpartum thyroiditis is an inflammatory condition of the thyroid that can occur after childbirth. It affects about 10% of women and may lead to either hyperthyroidism or hypothyroidism in the months following delivery. The condition is often temporary, but some women may experience long-term hypothyroidism.
- Removal of the Thyroid Gland
Surgical removal of the thyroid gland, known as a thyroidectomy, can result in hypothyroidism. This may be necessary for conditions such as thyroid cancer or severe hyperthyroidism. Additionally, some treatments for thyroid disorders, like radioactive iodine therapy, can chemically destroy thyroid tissue, leading to decreased hormone production.
- Medications
Certain medications can induce hypothyroidism as a side effect. One of the most notable is lithium, which is used to treat bipolar disorder. Other medications, such as some antiepileptics and amiodarone, can also impact thyroid function and lead to hypothyroidism.
- Congenital Defects
Hypothyroidism can also be present from birth due to congenital defects. These defects may affect the development of the thyroid gland or its ability to produce hormones, potentially leading to complications such as mental retardation, goiter, and short stature if left untreated.
- Iodine Deficiency
Iodine is an essential nutrient required for the production of thyroid hormones. A lack of iodine in the diet can diminish the thyroid gland’s ability to synthesize sufficient hormones, leading to hypothyroidism. This condition is less common in developed countries due to the iodization of salt, but it can still occur in areas where iodine intake is low.
Management of Thyroid Cancer
Thyroid cancer, although relatively rare, is highly treatable, particularly when detected early. The management of thyroid cancer involves a combination of surgical and therapeutic approaches tailored to the specific type and stage of the disease. Here are the key treatment modalities for thyroid cancer:
- Surgery
Surgery is the cornerstone of treatment for thyroid cancer. The most common surgical procedures include:
- Thyroidectomy: This involves the complete (total thyroidectomy) or partial removal (hemithyroidectomy) of the thyroid gland. The extent of surgery depends on the size and type of the tumor, as well as whether cancer has spread to nearby lymph nodes.
- Radioactive Iodine Therapy
After surgery, patients may undergo radioactive iodine therapy. This treatment is used to destroy any remaining thyroid tissue or cancer cells that were not removed during surgery. Radioactive iodine is taken orally and selectively targets thyroid cells, making it effective in treating thyroid cancer.
- Thyroid Hormone Therapy
Following the removal of the thyroid gland, patients will require lifelong thyroid hormone replacement therapy. This helps prevent hypothyroidism and maintains normal metabolic function. Additionally, suppressing thyroid-stimulating hormone (TSH) levels is crucial, as elevated TSH can promote cancer recurrence. Regular monitoring of hormone levels is necessary to adjust dosages accordingly.
- External Radiation Therapy and Chemotherapy
While surgery, radioactive iodine therapy, and hormone replacement are the primary treatments, external radiation therapy and chemotherapy may be employed in specific cases. These treatments are less commonly used and are typically reserved for advanced or aggressive forms of thyroid cancer that do not respond well to other therapies.
- Targeted Therapy
For patients with advanced thyroid cancer that is resistant to traditional treatments, targeted therapy may be an option. Drugs such as tyrosine kinase inhibitors (TKIs) specifically target molecular pathways involved in cancer growth and progression. This approach is tailored to the individual characteristics of the cancer and may provide additional treatment options.
Understanding Thyroiditis
Thyroiditis refers to the inflammation of the thyroid gland, which can be associated with either hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid). This condition can arise from various causes, including autoimmune disorders, infections, exposure to toxic substances, or may occur without a known cause (idiopathic).
Causes of Thyroiditis
1. Autoimmune Disorders:
- The most common form of thyroiditis is Hashimoto’s thyroiditis, where the immune system mistakenly attacks the thyroid gland, leading to its gradual destruction and resulting in hypothyroidism.
2. Infections:
- Viral or bacterial infections can cause inflammation of the thyroid gland, leading to temporary hyperthyroidism or hypothyroidism.
3. Chemical Exposure:
- Certain chemicals that are toxic to the thyroid can induce inflammation and alter its function.
4. Idiopathic:
- In some cases, the cause of thyroiditis remains unknown, categorized as idiopathic thyroiditis.
Hashimoto’s Thyroiditis (Autoimmune Hypothyroidism)
Hashimoto’s thyroiditis is a specific type of autoimmune thyroiditis where the body’s immune system targets the thyroid gland. Over time, this can lead to a decrease in thyroid hormone production, resulting in hypothyroidism.
Management of Hashimoto’s Thyroiditis
Effective management of Hashimoto’s thyroiditis primarily focuses on restoring normal thyroid function and addressing symptoms of hypothyroidism. Key approaches include:
1. Thyroid Hormone Replacement:
- Levothyroxine is the standard treatment for managing hypothyroidism caused by Hashimoto’s thyroiditis. This synthetic thyroid hormone helps normalize hormone levels, alleviating symptoms associated with low thyroid function.
2. Dietary Support:
- Some studies suggest that dietary modifications may benefit individuals with Hashimoto’s. Specifically, reducing gluten and avoiding foods that trigger autoimmune responses may help improve symptoms for certain individuals.
3. Monitor Antibody Levels:
- Regular monitoring through blood tests to measure thyroid antibodies (anti-TPO) and thyroid hormone levels is essential. This helps assess the progression of the disease and the effectiveness of treatment.
Understanding Graves’ Disease

Graves’ disease is an autoimmune disorder that leads to hyperthyroidism, a condition characterized by the excessive production of thyroid hormones. This overactivity of the thyroid gland can result in a range of symptoms and complications, making effective management crucial for maintaining overall health.
Management of Graves’ Disease
Managing Graves’ disease typically involves a multifaceted approach aimed at controlling hyperthyroidism, alleviating symptoms, and addressing any associated complications, such as eye problems. The primary management strategies include:
- Anti-Thyroid Medications or Radioactive Iodine Therapy
- Anti-Thyroid Medications: Medications such as methimazole or propylthiouracil are often prescribed to inhibit the production of thyroid hormones. These medications help normalize hormone levels and alleviate symptoms of hyperthyroidism.
- Radioactive Iodine Therapy: This treatment involves administering radioactive iodine, which is absorbed by the thyroid gland. It effectively reduces hormone production by destroying overactive thyroid cells. Radioactive iodine therapy is a common and effective treatment option for Graves’ disease.
- Surgery
- In certain cases, a thyroidectomy (partial or complete removal of the thyroid gland) may be necessary, especially if there is a large goiter, significant pressure symptoms, or if other treatments are not effective or suitable for the patient.
- Beta-Blockers
- Beta-blockers, such as propranolol, are often used to control symptoms associated with hyperthyroidism, including rapid heart rate, tremors, and anxiety. These medications can provide relief while the underlying thyroid hormone levels are being regulated.
- Eye Care
- Graves’ disease can lead to Graves’ ophthalmopathy, a condition characterized by inflammation and swelling of the eye muscles and surrounding tissues, resulting in symptoms like bulging eyes, double vision, or discomfort. Regular monitoring by an ophthalmologist is essential for individuals with Graves’ disease to assess and manage these eye-related complications.
- In severe cases, treatments may include corticosteroids to reduce inflammation or surgical interventions to relieve pressure and correct vision problems.
Factors Influencing Thyroid Dysfunction
Thyroid dysfunction can arise from various factors, some of which may be more significant in certain individuals. Here are some key contributors that can impact thyroid health:
- Pregnancy
- Pregnancy can trigger thyroid dysfunction in some women, particularly in those who may already be predisposed to thyroid issues. Hormonal changes and increased demands for thyroid hormones during pregnancy can lead to conditions such as hypothyroidism or hyperthyroidism. Regular monitoring of thyroid function is essential for pregnant women to ensure both maternal and fetal health.
- Stress
- Severe stress or illness can significantly affect thyroid function. Stress activates the body’s fight-or-flight response, which can disrupt the delicate balance of hormones, including those produced by the thyroid gland. Chronic stress may lead to fluctuations in thyroid hormone levels, potentially resulting in dysfunction.
- Environmental Factors
- Exposure to certain chemicals or pollutants can adversely impact thyroid health. Substances such as heavy metals, pesticides, and industrial chemicals may interfere with thyroid hormone production and regulation. Awareness of environmental exposures and taking preventive measures can be beneficial in maintaining thyroid health.
- Diet
- Diet plays a critical role in thyroid function. Consuming large amounts of goitrogens—substances found in certain foods (such as cruciferous vegetables, soy, and millet) that can interfere with thyroid hormone production—may lead to thyroid dysfunction, particularly in individuals with existing iodine deficiency. However, a balanced diet that includes adequate iodine and other essential nutrients is vital for optimal thyroid health.
Understanding Thyroid Nodules
Thyroid nodules are growths that can form on or within the thyroid gland, which is located at the base of the neck. These nodules can vary in size and may be classified as either benign (non-cancerous) or malignant (cancerous). In some cases, a condition known as toxic nodular goiter or multinodular goiter can occur, where multiple nodules cause the thyroid to overproduce hormones, leading to hyperthyroidism.
Characteristics of Thyroid Nodules
- Benign Nodules: These are non-cancerous lumps that do not pose significant health risks. They may not require immediate treatment and can often be monitored.
- Malignant Nodules: These nodules can be cancerous and may necessitate further investigation and treatment.
Management of Thyroid Nodules
The management of thyroid nodules depends on their characteristics, size, and whether they are causing symptoms. Here are the common approaches:
- Observation
- For small, benign nodules that do not cause symptoms, a watchful waiting approach may be taken. This involves regular monitoring through ultrasounds and thyroid function tests to ensure that the nodule remains stable and does not change over time.
- Fine Needle Aspiration (FNA) Biopsy
- If there is any suspicion that a nodule may be cancerous, a fine needle aspiration (FNA) biopsy is performed. This procedure involves using a thin needle to extract a sample of tissue from the nodule for pathological examination. The results help determine the nature of the nodule and guide further management.
- Radioactive Iodine or Surgery
- For nodules that are hyperfunctioning (producing excess hormones), treatment options may include:
- Radioactive Iodine Therapy: This treatment helps to shrink the overactive nodules by destroying thyroid tissue.
- Surgery: In some cases, surgical intervention may be necessary to remove the nodule if it is causing symptoms or if there is a risk of cancer.
- Thyroidectomy
- If there is a strong suspicion of cancer, or if the nodule is causing significant symptoms (such as difficulty swallowing), a thyroidectomy may be performed. This surgery involves removing part or all of the thyroid gland, depending on the extent of the nodules and the overall health of the thyroid.
Understanding Goiter

Goiter is a medical condition characterized by an unusually enlarged thyroid gland, which can lead to noticeable swelling in the neck. While goiters can vary in size, the most common symptom is the visible enlargement of the thyroid. In some cases, a very large goiter may cause additional symptoms, such as:
- A tight feeling in the throat
- Coughing
- Difficulty swallowing
- Difficulty breathing
Management of Goiter
The management of goiter is largely dependent on various factors, including its cause, size, associated symptoms, and whether it is linked to thyroid dysfunction (such as hypothyroidism or hyperthyroidism) or other medical conditions. Here is an overview of the common management strategies for goiter:
- Observation (Small, Non-Symptomatic Goiter)
- Monitoring: If the goiter is small and not causing any symptoms, healthcare providers may adopt a “wait and see” approach. This involves regular check-ups, during which physical exams and thyroid function tests are conducted to monitor the size of the goiter and the levels of thyroid hormones.
- Ultrasound: Periodic ultrasound examinations may also be performed to observe any changes in the size or structure of the thyroid gland. This helps ensure that the goiter remains stable and does not progress.
Management: Naturopathy Therapy for Thyroid Health
Naturopathy offers a holistic approach to managing thyroid conditions, focusing on detoxification, dietary modifications, and the use of herbal remedies. Below are key components of naturopathic management for thyroid health.
- Detoxification Protocols
Detoxification is essential for maintaining optimal hormone balance and supporting overall thyroid health. Several methods can aid in detoxification:
- Detox Teas:
- Dandelion Tea: Known for its liver-supporting properties, dandelion tea can help improve liver function, which is crucial for hormone metabolism and detoxification.
- Ginger Tea: Ginger is an anti-inflammatory herb that can enhance digestion and support liver function. Drinking ginger tea may aid in reducing inflammation and promoting better metabolism.
- Hydration and Detoxification
Proper hydration is vital for detoxification and metabolic function, especially for individuals with thyroid issues.
- Water: It is important to drink plenty of water throughout the day. Staying well-hydrated supports metabolic processes and detoxification pathways, which are essential for overall organ function, including the thyroid.
- Dietary Modifications
Diet plays a critical role in thyroid health, particularly in conditions such as hypothyroidism and goiter, which can be influenced by iodine levels. Here are some dietary tips:
- Iodine-Rich Foods: Incorporate foods high in iodine, such as seaweed, fish, dairy products, and eggs, to support thyroid function.
- Nutrient-Dense Foods: Emphasize a diet rich in whole foods, including fruits, vegetables, whole grains, and lean proteins. These foods provide essential vitamins and minerals necessary for thyroid health.
- Avoid Goitrogens: Limit intake of raw cruciferous vegetables (like broccoli, cauliflower, and kale) as they can interfere with iodine uptake. Cooking these vegetables can reduce their goitrogenic properties.
- Healthy Fats: Include sources of omega-3 fatty acids, such as fatty fish, flaxseeds, and walnuts, to reduce inflammation and support overall thyroid function.
- Balanced Weight Plan: Tailor the diet according to individual weight management goals, ensuring that caloric intake aligns with energy needs while supporting thyroid health.
Dietary Recommendations for Thyroid Conditions
Diet plays a crucial role in managing thyroid conditions such as hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid). Here are specific dietary guidelines for each condition.
For Hypothyroidism (Underactive Thyroid)
- Iodine-Rich Foods:
- Importance: Iodine is essential for the production of thyroid hormones.
- Sources: Include iodized salt, dairy products, eggs, seaweed, and fish in your diet to ensure adequate iodine intake.
- Sea Kelp: Commercially available sea kelp is a rich source of iodine.
- Caution: While iodine is crucial, too much can be harmful, especially for individuals with autoimmune thyroid diseases like Hashimoto’s thyroiditis. It is advisable for these individuals to avoid excessive iodine intake.
For Hyperthyroidism (Overactive Thyroid)
1. Avoid Iodine-Rich Foods:
- Reason: Excess iodine can stimulate the production of thyroid hormones, exacerbating hyperthyroidism.
- Limitation: Reduce intake of seafood, seaweed, iodized salt, and iodine-containing supplements.
2. Cruciferous Vegetables:
- Benefit: Foods such as broccoli, cabbage, kale, cauliflower, and Brussels sprouts can inhibit thyroid hormone production, potentially helping to manage hyperthyroidism.
- Note: This approach should be seen as supplementary and not a definitive cure.
3. Limit Caffeine:
- Impact: Hyperthyroidism can lead to symptoms like anxiety and rapid heart rate. Avoiding caffeine (found in coffee, tea, chocolate, and some sodas) may help alleviate these symptoms.
4. Avoid Goitrogenic Foods:
- Description: Goitrogens are substances in some foods that can interfere with thyroid function.
- Foods to Limit:
- Cruciferous Vegetables: Cabbage, broccoli, cauliflower, kale, and Brussels sprouts.
- Soy-Based Products: Soybeans, tofu, and soy milk.
- Millet and Cassava: These can inhibit thyroid function when consumed in large amounts.
- Cooking: Cooking goitrogenic foods often reduces their goitrogenic properties, so they may not need to be entirely avoided.
- Avoid Gluten (if necessary):
- Recommendation: Some individuals with hypothyroidism, particularly those with autoimmune conditions like Hashimoto’s thyroiditis, may benefit from reducing or avoiding gluten found in wheat and rye.
Supplements for Thyroid Health
Supplements can play a significant role in supporting thyroid function and overall health, particularly for individuals dealing with thyroid conditions. However, it is essential to use them under medical supervision, especially if you are receiving thyroid treatment. Here’s an overview of beneficial supplements for thyroid health:
- Vitamin D
- Role: Vitamin D deficiency has been associated with autoimmune thyroid diseases, making it crucial for thyroid health.
- Sources: Aim to spend time in the sun to increase your vitamin D levels naturally. If necessary, consider vitamin D supplements, particularly if your blood tests indicate low levels.
- Omega-3 Fatty Acids
- Benefits: Omega-3 fatty acids, found in fish oil and flaxseed, help reduce inflammation and support the immune system. This is particularly beneficial for those with autoimmune thyroid conditions.
- Sources: Incorporate fatty fish (such as salmon and sardines) or consider taking an omega-3 supplement.
- Probiotics
- Importance: Gut health is closely linked to thyroid function. A healthy gut microbiome can positively impact overall health and immune function.
- Sources: Include probiotic-rich foods like yogurt, kefir, sauerkraut, and kombucha in your diet to support gut health.
- B-Complex Vitamins

- Function: B vitamins, particularly B12, play a crucial role in energy production and overall metabolic health. They can also support thyroid health.
- Sources: Include a variety of B-vitamin-rich foods such as whole grains, legumes, eggs, and leafy green vegetables.
- Selenium
- Role: Selenium is essential for the conversion of thyroid hormones into their active forms, supporting overall thyroid function.
- Selenium-Rich Foods: Incorporate foods such as Brazil nuts, sunflower seeds, tuna, mushrooms, and eggs into your diet to ensure adequate selenium intake.
- Zinc
- Importance: Zinc plays a significant role in maintaining thyroid function and is essential for hormone production.
- Sources: Include zinc-rich foods like chickpeas, cashews, pumpkin seeds, and lentils to support your thyroid health.
- Apple Cider Vinegar Gargle
- Usage: While not a supplement in the traditional sense, apple cider vinegar can be used as a gargle to support oral health and may have beneficial effects on metabolism. However, it should be used in moderation and properly diluted.
Lifestyle Adjustments for Thyroid Health
Maintaining thyroid health requires a holistic approach that includes not only dietary considerations but also essential lifestyle adjustments. Stress and other lifestyle factors can significantly impact thyroid function. Here are some effective strategies for promoting thyroid health:
- Stress Management
- Impact of Stress: Chronic stress can exacerbate thyroid conditions by disrupting hormone balance and negatively affecting overall health.
- Techniques:
- Yoga: Practicing yoga can improve flexibility and strength while promoting relaxation.
- Meditation: Mindfulness and meditation techniques can help calm the mind, reduce anxiety, and enhance overall well-being.
- Deep Breathing Exercises: Engaging in deep breathing can reduce stress levels and promote relaxation.
- Tai Chi: This gentle martial art combines movement and meditation, making it an excellent option for stress reduction.
- Exercise
- Benefits: Regular physical activity supports overall health, aids in maintaining a healthy weight, and boosts metabolism—especially important for individuals with hypothyroidism.
- Recommendations:
- For Hypothyroidism: Incorporate moderate to vigorous exercise routines to help stimulate metabolism and energy levels. Activities may include jogging, cycling, or strength training.
- For Hyperthyroidism: Choose calming and less strenuous exercises such as yoga, walking, or light swimming to prevent overexertion and help manage symptoms.
- Adequate Sleep
- Importance of Sleep: Quality sleep is vital for hormone balance and optimal thyroid function. Inadequate sleep can lead to increased stress and exacerbate thyroid issues.
- Recommendations: Aim for 7-9 hours of uninterrupted sleep each night. Consider establishing a bedtime routine, limiting screen time before bed, and creating a comfortable sleep environment to improve sleep quality.
Herbal Remedies for Thyroid Health
Herbal remedies can play a supportive role in maintaining thyroid health, particularly for individuals with hypothyroidism. It is essential to consult with a healthcare provider before starting any herbal supplements, as they may interact with medications or cause unwanted side effects. Here are some herbs commonly associated with supporting thyroid function:
For Hypothyroidism:
1. Ashwagandha (Withania somnifera)
- Benefits: Ashwagandha is an adaptogenic herb known for its ability to help balance thyroid hormone levels, particularly in cases of hypothyroidism. It has been shown to support adrenal function and reduce stress, which is crucial for maintaining overall thyroid health.
- Usage: It can be taken in capsule form, as a powder mixed with water or milk, or in tincture form.
2. Guggul (Commiphora mukul)
- Benefits: Guggul has been traditionally used in Ayurvedic medicine to promote thyroid function and enhance metabolism. It is believed to help stimulate thyroid hormone production and may assist with weight management, making it beneficial for those experiencing weight gain due to hypothyroidism.
- Usage: Guggul can be taken in capsule or tablet form, and its extracts are commonly found in various herbal formulations for thyroid health.
3. Kachnar Guggul
- Benefits: Kachnar Guggul is a blend of several herbs, including Guggul, and is specifically used in Ayurvedic practices for thyroid health. It is believed to help in managing goiter and supporting overall thyroid function.
- Usage: This formulation is typically available in tablet form and may be recommended by a healthcare provider based on individual health needs.
Herbal Remedies and Essential Oils for Hyperthyroidism
Managing hyperthyroidism may involve a combination of conventional treatments and complementary approaches, such as herbal remedies and essential oils. It’s important to consult with a healthcare professional before incorporating these methods into your treatment plan, as they can interact with medications and affect thyroid function.
For Hyperthyroidism:
1. Ashwagandha (Withania somnifera)
- Benefits: Ashwagandha is known for its adaptogenic properties, which can help reduce anxiety and stress often associated with an overactive thyroid. Its calming effects make it a suitable herb for those experiencing heightened emotions due to hyperthyroidism.
- Usage: It can be consumed in tea form, which is a soothing way to incorporate this herb into your routine.
2. Shatavari (Asparagus racemosus)
- Benefits: Shatavari is traditionally used to address various female reproductive issues and may be beneficial in managing symptoms associated with sweating and hormonal imbalances linked to hyperthyroidism.
- Usage: This herb can be taken in powder or capsule form, or brewed as a tea.
3. Arjuna (Terminalia arjuna)
- Benefits: Arjuna is known for its ability to support heart health and can help calm heart palpitations and anxiety that often accompany hyperthyroidism.
- Usage: It is best consumed in tea form, providing a soothing beverage that may alleviate some symptoms.
Essential Oils
Essential oils can be a beneficial addition to the management of thyroid symptoms but should never replace conventional medical treatment. Here are some oils that may support thyroid health, particularly in hyperthyroidism:
1. Lavender Oil
- Benefits: Lavender oil is renowned for its stress-relieving properties and can promote relaxation, making it beneficial for those experiencing anxiety related to hyperthyroidism.
- Usage: Lavender oil can be used in a diffuser for inhalation or diluted in a carrier oil for topical application.
2. Lemongrass Oil
- Benefits: Lemongrass oil is believed to support thyroid health when applied topically, especially in the neck area.
- Usage: Always dilute lemongrass oil in a carrier oil (like coconut or olive oil) before applying it to the skin.
Hydrotherapy
- Technique: Hydrotherapy can be an effective adjunctive therapy for managing thyroid symptoms. Placing a wet warm compress (or “patti”) on the neck area for 20 minutes can help soothe discomfort and promote relaxation.
Complementary Therapies for Thyroid Health: Acupuncture and Reflexology
In addition to dietary modifications and herbal remedies, complementary therapies like acupuncture and reflexology may play a role in supporting thyroid health, particularly for conditions like hyperthyroidism. Here’s a closer look at how these therapies can contribute to thyroid wellness.
Acupuncture

- Overview: Acupuncture is a traditional Chinese medicine practice that involves inserting thin needles into specific points on the body to promote healing and balance.
- Benefits for Thyroid Health:
- Some studies suggest that acupuncture may help regulate thyroid function and balance hormone levels, particularly in cases of hyperthyroidism.
- By stimulating certain points, acupuncture may enhance circulation, reduce inflammation, and promote overall hormonal balance, potentially alleviating symptoms associated with thyroid dysfunction.
- Considerations: It’s important to seek treatment from a qualified and licensed acupuncturist who has experience in treating thyroid conditions.
Reflexology
- Overview: Reflexology is a holistic therapy that involves applying pressure to specific points on the feet, hands, or ears. These points correspond to different organs and systems in the body.
- Benefits for Thyroid Health:
- Practitioners of reflexology may target specific pressure points that correspond to the thyroid gland, which is believed to help promote thyroid health and balance hormone levels.
- This therapy aims to relieve stress, improve circulation, and encourage the body’s natural healing processes, which can be beneficial for individuals with thyroid disorders.
- Considerations: Reflexology can be a relaxing and supportive therapy, but it should be used in conjunction with traditional medical treatments and not as a standalone solution.
Regular Monitoring of Thyroid Health
Monitoring thyroid health is essential for individuals diagnosed with thyroid disorders, whether they are receiving treatment or managing their condition through lifestyle and dietary changes. Here’s why regular monitoring is important:
Importance of Regular Monitoring
- Track Thyroid Function: Regular blood tests to measure Thyroid Stimulating Hormone (TSH), T4, and T3 levels help healthcare providers assess how well the thyroid is functioning. These tests can identify any fluctuations in hormone levels that may require adjustments in treatment.
- Evaluate Treatment Efficacy: For those undergoing treatment for conditions like hypothyroidism or hyperthyroidism, regular monitoring allows healthcare providers to evaluate the effectiveness of medications or therapies. Adjustments can be made based on the results to ensure optimal management of the condition.
- Monitor for Complications: Regular imaging tests, such as ultrasounds, can help monitor the size of a goiter or the presence of nodules. This is crucial for identifying any changes that may indicate complications, including potential malignancy in nodules or changes in thyroid structure.
- Prevent Symptoms and Side Effects: By keeping a close watch on thyroid levels, healthcare providers can help prevent the development of symptoms associated with hypothyroidism or hyperthyroidism, such as fatigue, weight changes, and mood disturbances.
- Individualized Care: Regular monitoring facilitates personalized care plans. Based on test results, healthcare providers can make informed decisions tailored to each individual’s needs, ensuring comprehensive management of thyroid health.
Western Approach to Managing Thyroid Conditions
The management of thyroid conditions, including goiter, is often approached through conventional Western medicine. This involves a combination of medications, radioactive iodine therapy, and, in some cases, surgical intervention. Here’s a breakdown of these strategies:
- Medications
Levothyroxine (Thyroid Hormone Replacement)
- Indication: Used primarily for individuals with hypothyroidism (underactive thyroid) causing a goiter.
- Mechanism: This synthetic thyroid hormone helps reduce TSH levels, which can decrease the size of the goiter by ensuring adequate hormone levels in the body.
Anti-thyroid Medications
- Indication: Prescribed for patients with hyperthyroidism (overactive thyroid) that leads to goiter formation.
- Examples: Medications like Methimazole or Propylthiouracil (PTU) work by inhibiting the production of thyroid hormones, thereby potentially reducing the size of the goiter.
- Monitoring: Regular blood tests (TSH, T4, T3) are essential to adjust medication dosages and ensure effective thyroid function.
- Radioactive Iodine Therapy
- Indication: Effective for hyperthyroidism associated with conditions like Graves’ disease or toxic multinodular goiter.
- Mechanism: Radioactive iodine is administered orally and selectively absorbed by the thyroid gland. The radiation helps shrink the gland and reduce its hormone production.
- Risks: One of the potential side effects is the development of hypothyroidism post-treatment, necessitating lifelong thyroid hormone replacement therapy.
- Surgery (Thyroidectomy)
Indications for Surgery
- Surgical intervention may be recommended if the goiter is large and causing symptoms, such as:
- Difficulty swallowing
- Breathing problems
- Compression of nearby structures (e.g., trachea or esophagus)
- Surgery is also considered in cases where there is a suspicion of thyroid cancer or when the goiter is causing cosmetic concerns.
Types of Thyroidectomy
- Partial Thyroidectomy: Involves the removal of only a portion of the thyroid gland, typically when the goiter is localized.
- Total Thyroidectomy: Complete removal of the thyroid is performed in more severe cases or when cancer is suspected.
Post-Surgical Care
- Patients who undergo thyroidectomy generally require lifelong treatment with Levothyroxine to maintain normal thyroid hormone levels and prevent hypothyroidism.








