GOUT, ARTHRITIS, SPONDYLITIS PART 1
Understanding Joint Inflammation and Its Impact on Flexibility
Joint inflammation is a prevalent issue that can lead to significant discomfort, particularly for individuals suffering from arthritis. This article outlines the key aspects of joint inflammation, its causes, symptoms, and its impact on flexibility.
1. Joint Inflammation and Arthritis
- Joint inflammation is commonly associated with arthritis, a condition characterized by inflammation and swelling of the joints.
- Individuals with arthritis often experience elevated uric acid levels, leading to additional pain and swelling due to the formation of uric acid crystals in the joints.
2. Reduction in Joint Flexibility
- Inflammation can result in a noticeable decrease in joint flexibility.
- Patients frequently report difficulties in gripping objects or making quick movements.
3. Impact on Mobility and Circulation
- Pain and swelling associated with inflammation hinder mobility and restrict blood circulation around the affected area.
- This restriction exacerbates the loss of flexibility, creating a cycle of increased discomfort.
4. Wear and Tear on Cartilage
- Over time, the ongoing wear and tear on cartilage and surrounding tissues can lead to additional stiffness in the joints.
- This stiffness further contributes to reduced flexibility and mobility.
5. Cycle of Pain and Stiffness
- The relationship between reduced flexibility and less movement can create a detrimental cycle:
a.Reduced Flexibility
b.Less Movement
c.Increased Stiffness
d.More Discomfort
6. Everyday Challenges
- Individuals often find their focus consumed by pain and mobility limitations, making everyday activities increasingly challenging.
- Some patients may also hear clicking or cracking sounds in their joints, which can be disconcerting and is often linked to underlying arthritis.
By recognizing the effects of joint inflammation on flexibility and mobility, individuals can take proactive steps toward managing their condition effectively.
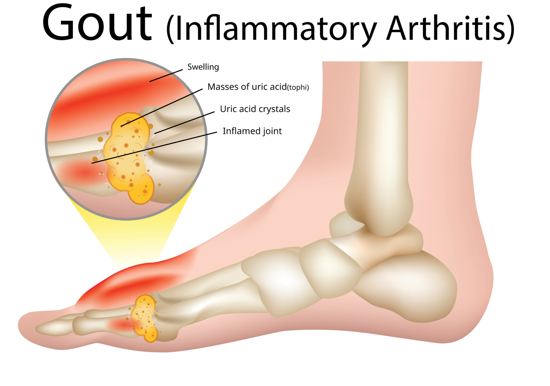
Understanding Uric Acid Crystals and Arthritis: Key Differences
High uric acid levels can lead to the deposition of uric acid crystals in the joints, causing improper joint movement and friction. This article explores the implications of these crystals on joint health and distinguishes between osteoarthritis and rheumatoid arthritis.
Uric Acid Crystals and Joint Movement
1. Crystal Deposition: Elevated uric acid levels result in the formation of uric acid crystals in the joints.
2.Movement Restrictions: The presence of these crystals can restrict proper joint movement, leading to discomfort.
3. Physical Examination: During a physical checkup, bending affected joints may produce crackling or cracking sounds.
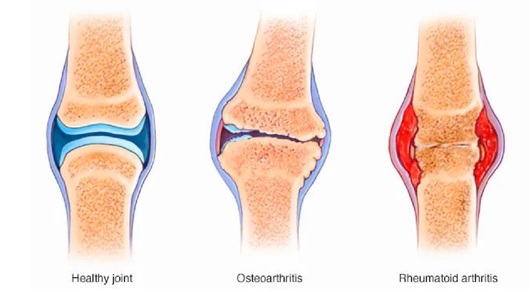
Differentiating Arthritis Types
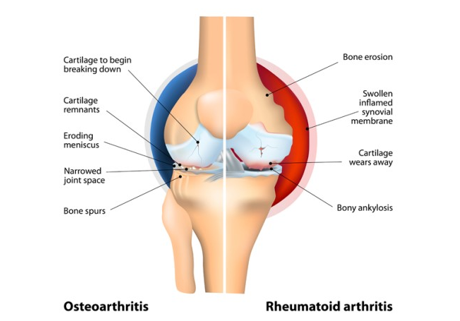
1.Osteoarthritis
- Asymmetry: Osteoarthritis typically affects one side of the body. For example, if the right knee is affected, the left knee may remain unaffected.
- Localized Impact: The condition does not necessarily impact both joints simultaneously.
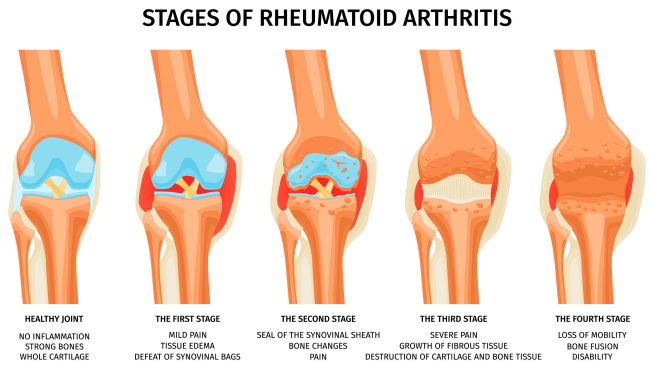
2.Rheumatoid Arthritis
- Symmetrical Impact: Unlike osteoarthritis, rheumatoid arthritis affects both joints equally. If the right knee is impacted, the left knee is likely to be affected as well.
- Systemic Nature: This form of arthritis has a more widespread impact on the joints.
Understanding the Causes and Risk Factors of Osteoarthritis
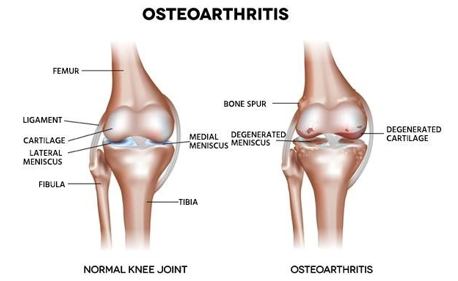
Osteoarthritis is a complex condition with no specific cause identified to date. Various factors contribute to its development, and understanding these can aid in prevention and management. Below are key observations regarding the causes and risk factors associated with osteoarthritis.
Key Causes of Osteoarthritis
1. Genetic Predisposition
Family history plays a significant role in the likelihood of developing osteoarthritis. Studies indicate that if family members, such as grandparents or parents, have had osteoarthritis, there is a 90% chance that subsequent generations may also experience the condition.
2. Job-Related Stress
Certain occupations that involve prolonged standing or repetitive joint stress can increase the risk of osteoarthritis. Examples include roles in sales, security, and other fields requiring long hours on one’s feet.
3. Athletic Activities
Athletes often face repeated stress and injuries to their joints, which can lead to osteoarthritis over time. Specific sports, such as running and jumping, put excessive pressure on joints, leading to wear and tear on ligaments and cartilage.
4. Autoimmune Diseases and Infections
A small percentage of arthritis cases may be linked to autoimmune diseases or viral infections that complicate diagnosis. These conditions can spread rapidly through the body, making timely diagnosis and treatment challenging.
Risk Factors for Osteoarthritis
1. Age
As individuals age, the likelihood of developing osteoarthritis increases significantly. By the age of 70 or 80, many individuals are at a higher risk due to the natural aging process affecting joint elasticity and function.
2. Lifestyle Choices
Lifestyle factors are critical in the development of osteoarthritis, including diet, rest, stress management, and exercise routines. Poor lifestyle habits, such as late-night eating and lack of physical activity, can contribute to the condition.
3. Mobile Device Use
The modern trend of excessive mobile device usage is leading to an increase in joint problems, particularly in the fingers. Prolonged scrolling and typing can strain finger joints, leading to early signs of arthritis.
4. Weight Management
Excess body weight places additional stress on weight-bearing joints, increasing the risk of developing osteoarthritis.
Understanding Osteoarthritis and Rheumatoid Arthritis
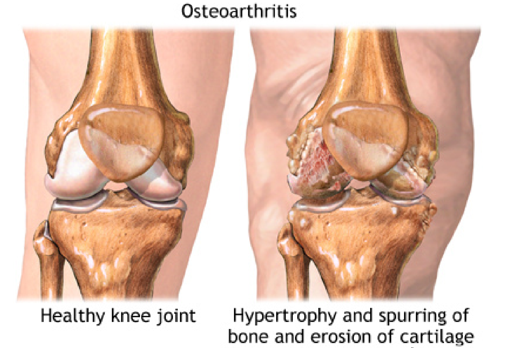
1.Osteoarthritis Overview:
- Gender Prevalence:
While it is commonly believed that osteoarthritis affects females more, research indicates that males are more affected globally. - Injuries as Risk Factors:
Accidents and injuries at any age can trigger osteoarthritis.Incomplete recovery from such injuries increases the risk of developing arthritis later in life. Ensuring complete recovery from injuries is critical to preventing long-term joint issues. - Weight Management in Treatment
a.If a patient with osteoarthritis is overweight or obese, doctors typically recommend weight reduction before considering further treatments, including surgery.
b.Excessive body fat puts additional pressure on the cartilage, bones, and joints, worsening osteoarthritis symptoms.
c.Weight reduction has been shown to significantly reduce symptoms such as pain and inflammation.
d.Losing 8-10 kg can cause immediate relief from inflammation, with pain gradually subsiding as well.
e.Weight is a major risk factor for osteoarthritis, with symptoms often improving when excess weight is lost.
2.Rheumatoid Arthritis Overview
- Definition:
Rheumatoid arthritis (RA) is a chronic autoimmune and inflammatory disease that affects the joints. - Medical Treatment:
Current treatments focus on managing symptoms with injections and painkillers.However, these treatments do not cure the autoimmune condition itself. - Naturopathy and Alternative Therapies:
Alternative treatments focus on slowing disease progression rather than achieving full recovery, as RA is a lifelong condition.The goal is to manage symptoms and halt the autoimmune response. - Self-Care for Patients:
Patients with RA must follow specific lifestyle changes and restrictions to manage their symptoms effectively.
3.Key Differences Between Osteoarthritis and Rheumatoid Arthritis:
- Joint Involvement:
Osteoarthritis often affects a single joint, while rheumatoid arthritis usually impacts multiple joints symmetrically. - Common Areas Affected:
RA commonly affects the fingers, wrists, knees, and ankles.There is an increase in RA cases linked to the extensive use of laptops and mobile devices, affecting the fingers and hands.
4.Risks Associated with Modern Lifestyles:
The increased use of technology has led to a rise in repetitive strain injuries, particularly in the hands and fingers, contributing to the growing prevalence of rheumatoid arthritis.
The Impact of Rheumatoid Arthritis: Risks and Complications

Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects the joints, but its
consequences can extend beyond just joint pain and swelling. Here’s a breakdown of how RA affects the
body and the importance of early intervention to prevent severe complications.
1. Joint Damage and Impaired Mobility
- RA targets joints, leading to pain, swelling, stiffness, and reduced mobility.
- Individuals may find it especially challenging to perform daily tasks without proper use of their hands and legs.
- People with RA in their hands, wrists, or fingers may struggle with grip strength, severely limiting their ability to handle objects or perform tasks like writing.
2. Difficulties in Daily Activities
- For individuals whose professions involve manual dexterity, such as writers, tremors and finger stiffness can make it impossible to work.
- Everyday tasks, such as holding utensils, bowls, or feeding oneself, become challenging due to the lack
of grip and hand coordination.
3. Systemic Risks of Untreated Rheumatoid Arthritis
- Heart: If RA is not treated properly, inflammation can spread to other organs, raising the risk of heart-related issues, including heart attacks, strokes, and blockages.
- Kidneys: The kidneys play a key role in detoxifying the body. If they are affected, the risk of developing conditions such as gout increases due to a buildup of uric acid. Kidney dysfunction leads to further complications.
- Lungs: Inflammation in the lungs impairs the body’s ability to properly process oxygen, resulting in
increased carbon dioxide levels. This leads to breathing difficulties and further systemic damage.
4. Widespread Complications
- If RA remains untreated or is poorly managed, it can affect the entire body, leading to significant health risks.
- Conditions like toxemia, which is poisoning of the blood by toxins, may develop due to the body’s inability to eliminate waste products properly.
5. The Importance of Early and Effective Treatment
- Early intervention is critical in managing RA and preventing these severe complications.
- Proper medical care and therapies can help mitigate the risks of systemic damage to vital organs and maintain a better quality of life.
Rheumatoid Arthritis (RA) is a chronic autoimmune disorder that affects joints and can have a profound
impact on daily life. Here’s an overview of the symptoms, causes, and key factors affecting RA.
1. Symptoms of RA
- Joint Pain and Swelling: RA typically affects both sides of the body, causing pain, swelling, and stiffness in joints. It commonly affects fingers, toes, wrists, and knees.
- Deformity of Joints: Over time, affected joints may become deformed, especially in the fingers and toes.
- Additional Symptoms: Patients often experience weakness, fatigue, fever, and prolonged morning stiffness.
2. Chronic Impact on Joints
- Deformed Joints: RA may lead to bent or misaligned fingers and toes. This occurs due to prolonged inflammation, which damages the joint structures.
- Tenderness: Despite adequate rest and nutrition, patients often experience joint tenderness because of the autoimmune nature of the disease.
3. Fatigue and Fever
- Fatigue: A common symptom, fatigue can be overwhelming for RA patients and impacts their overall
quality of life. - Low-Grade Fever: Many patients experience mild fever around 99°F, indicating ongoing
inflammation in the body.
4. Morning Stiffness
- Pain After Sleep: Unlike healthy individuals who wake up refreshed, RA patients often wake up with joint pain and stiffness, particularly after prolonged periods of inactivity such as sleep.
5. Causes of Rheumatoid Arthritis
- Genetic Factors: RA is believed to have a genetic component, where certain genes increase the likelihood of developing the disease.
- Hormonal and Environmental Triggers: Hormonal changes, particularly in women, and
environmental factors may trigger the onset of RA.
6. Hormonal Influence on RA
- Prevalence in Women: RA is more common in women, especially those in post-menopause, due to the significant hormonal changes during this time.
- Male RA Patients: While men can also develop RA, other factors like age and stress play a more substantial role in disease onset.
7. Ages Commonly Affected
- Typical Onset: RA commonly begins between the ages of 30 and 60. In younger adults, it may start earlier, while in older individuals, onset may occur after age 60.
8. Customized Treatment for RA
- Tailored Treatment Plans: Treatments, such as hot and cold therapy, should be customized based on the patient’s age, symptoms, and level of inflammation. Overgeneralized treatment approaches can sometimes worsen symptoms.
9. Prevention and Care
- Regular Health Checkups: Routine medical evaluations, especially for those over 40, are essential for early detection and management of RA. Women in their pre- and post-menopausal stages should be especially vigilant.
- Mental Health: Stress and hormonal imbalances can worsen RA symptoms, so managing mental health is a critical aspect of RA care.
10. Importance of Counseling for Women
- Mental Health Support: For women, particularly those going through menopause, counseling can be helpful in managing RA. Hormonal changes and mood swings can aggravate RA symptoms, making mental health care an important component of treatment.
By understanding the symptoms, causes, and individualized care needed for RA, patients can better manage their condition and improve their quality of life.
Understanding Septic Arthritis: Causes, Diagnosis, and Management
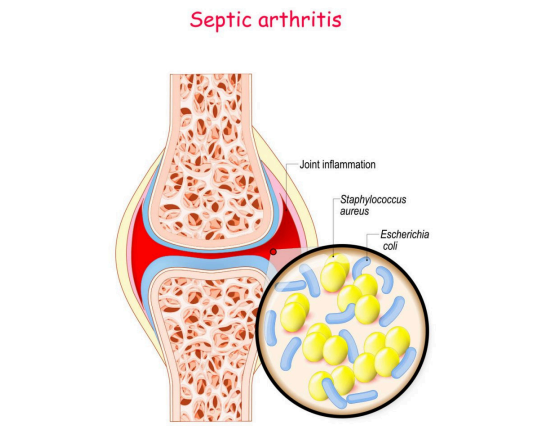
Septic arthritis, also referred to as juvenile or childhood arthritis, is a rare but serious condition. It occurs when the immune system mistakenly attacks the tissues surrounding the joints. This article explores septic arthritis, its causes, diagnosis, and management.
Causes of Septic Arthritis
- Immune System Malfunction: Septic arthritis occurs when the body’s immune system begins to attack its own joint tissues.
- Genetic Predisposition: The presence of the HLA-B27 gene can make individuals more susceptible to septic arthritis.
- Bacterial Infections: In some cases, bacterial infections, especially those caused by Staphylococcus bacteria, can trigger septic arthritis.
- No Known Cure: Despite ongoing research, there is no definitive cure for septic arthritis.
Diagnosis of Septic Arthritis
Diagnosing septic arthritis involves a comprehensive process, including a review of symptoms, physical examination, and diagnostic testing. The steps typically include:
1.Symptom Observation: Recognizing symptoms such as pain, stiffness, and swelling in the joints.
2.Physical Examination: A thorough physical assessment that examines:
- Joint movements
- Posture
- Pain levels
3.Family History: Taking into account the individual’s family history of arthritis or related conditions.
4.Imaging Tests: X-rays and MRI scans are often used to visualize joint damage and inflammation.
5.Blood Tests: To check for deficiencies linked to arthritis, including:
- Calcium
- Vitamin B12
- Vitamin D3
- Hemoglobin
Managing Septic Arthritis Symptoms
Management of septic arthritis focuses on reducing symptoms and improving joint function.
- Physiotherapy: This is a key component of arthritis management. It helps with:
a.Improving joint movement
b.Enhancing blood circulation
c.Reducing stiffness - Effectiveness of Physiotherapy: For individuals with mild to moderate symptoms, physiotherapy has shown improvement in approximately 50% of cases.
While there is no cure for septic arthritis, timely diagnosis and appropriate management can significantly improve the quality of life for those affected.
Naturopathic Approaches to Managing Arthritis
Naturopathy offers various strategies to manage arthritis, emphasizing tailored therapies and dietary adjustments. Below are key points outlining effective practices for managing arthritis through naturopathic methods.
1. Naturopathic Therapies
Application with Physiotherapy: Naturopathic therapies, when combined with physiotherapy, can significantly alleviate symptoms. While there are limited dietary recommendations, therapies and exercises can lead to about a 70% improvement in conditions.
2. Hot and Cold Therapy
Tailored Applications: The application of hot and cold therapy varies based on symptoms, age, body structure, and ongoing medications.
Recommended Duration: Generally, apply heat for 10 minutes followed by cold for another 10 minutes, adjusted according to the patient’s comfort and capacity.
3. Dietary Considerations
Diet is crucial for managing arthritis, focusing on individual needs based on Prakruti (constitution) and lifestyle.
a. Customizing Diet
Individualized Approach: The diet must be tailored to the patient’s unique constitution and lifestyle. Meal Timing: Consuming food according to the body’s biological clock optimizes digestion and minimizes symptom aggravation.
b. Meal Timing Guidelines
Digestive Gaps: Allow a gap of about 30 hours between meals to enable thorough digestion and waste elimination.
c. Foods to Avoid
For rheumatoid arthritis patients, the following should be avoided:
- Fermented and leftover foods
- Cold drinks and chilled water
- Highly salty, spicy foods
- White sugar and white flour Bakery products
d. Monitoring Food Reactions
Observational Approach: Track how patients respond to specific foods. If certain foods worsen symptoms like stiffness or pain, they should be avoided. If patients tolerate them well, they can remain in their diet.
4. Important Considerations
Food Allergies: Completely avoid any foods or drinks to which the patient is allergic, irrespective of their nutritional benefits.
Protein Sources: Recommend avoiding non-fish protein sources and specific legumes. Instead, include easily digestible proteins from options like moong (green gram) and wholesome grains.
5. Fiber and Hydration
a. Fiber Intake
Alternatives to Raw Vegetables: Many patients may struggle with raw salads; suggest roasted or cooked vegetables to provide sufficient fiber without discomfort.
b. Fluid Intake
Encouraging Healthy Liquids: Promote vegetable juices and soups, which can assist in managing symptoms. Recommended soups include:
- Drumstick soup
- Pumpkin soup
- Broccoli soup
6. Timing and Alternatives
Late-Night Options: For those craving late-night snacks, a glass of warm water is a simple and effective alternative, particularly for diabetic patients.
Naturopathy Therapies for Health and Wellness

Naturopathy offers various therapies that can significantly improve health, particularly for joint and bonerelated conditions. Below are some effective naturopathic treatments:
1. Sun Bathing
- Benefits: Sun bathing enhances joint, bone, and cartilage health.
- Recommendation: 5 to 10 minutes of sun exposure daily can boost Vitamin D levels, improve body warmth, and enhance oxygen levels.
2. Mud Therapy
- Benefits: Mud therapy effectively reduces inflammation and pain.
- Application: Apply mud to the affected areas for 20 minutes. The mud contains calcium and minerals that aid in healing.
3. Yoga and Pranayama
- Yoga: Yoga should be tailored to the patient’s comfort level, avoiding overstretching.
- Pranayama: Regular deep breathing exercises enhance lung health, oxygen circulation, and overall body regeneration.
4. Herbal Remedies
- Punarnava: Known for its tissue regeneration properties, particularly beneficial for arthritis.
- Turmeric (Haldi): Possesses anti-inflammatory and pain-relieving properties, beneficial when incorporated regularly in cooking.
- Tulsi: Acts as a blood purifier, with a recommendation to chew 8 to 10 leaves daily.
- Giloi: Boosts immunity and is especially useful for autoimmune conditions like rheumatoid arthritis.
- Alfalfa: Rich in calcium and fiber, it improves hemoglobin and mineral levels, making it useful for patients with deficiencies.
By incorporating these naturopathic therapies into daily routines, individuals can promote healing and improve their overall health.