LUMBAR DISC PROLAPSE
LUMBAR DISC PROLAPSE
Lumbar disc prolapse, also known as a herniated or slipped disc, is a condition that occurs when the soft inner core of a spinal disc leaks out through a tear in the outer layer. This can lead to compression or irritation of the nearby spinal nerves, causing pain, numbness, or weakness in the lower back, buttocks, legs, or feet.
The spinal discs act as cushions between the vertebrae, providing flexibility and absorbing shock during movement. However, with age or injury, these discs can degenerate or weaken, making them more prone to herniation. Other factors such as improper lifting, sudden twisting movements, or obesity can also increase the risk of disc prolapse.
Symptoms of lumbar disc prolapse can vary depending on the location and severity of the prolapsed disc. Common symptoms include localized or radiating pain in the lower back, buttocks, thighs, or legs (sciatica), numbness or tingling sensation in the legs or feet, weakness in the legs, and difficulty in walking or standing for long periods.
Diagnosis of lumbar disc prolapse typically involves a physical examination to assess the range of motion, reflexes, and muscle strength, along with imaging tests such as X-rays, MRI, or CT scans to visualize the location and extent of the prolapse.
Treatment options for lumbar disc prolapse aim to relieve pain, reduce inflammation, and improve mobility. Mild cases can often be managed with rest, physical therapy, and pain medications. In more severe cases where conservative treatments fail to provide relief, corticosteroid injections or surgical procedures such as discectomy or laminectomy may be recommended to remove or repair the prolapsed disc.
In conclusion, lumbar disc prolapse is a common spinal condition that can cause significant discomfort and impairment in daily activities. Understanding the causes, symptoms, and treatment options can help individuals manage the condition effectively and improve their quality of life. If you suspect you have a lumbar disc prolapse, it is important to consult with a healthcare professional for proper diagnosis and personalized treatment plan.
Understanding the Anatomy and Function of the Intervertebral Disc:
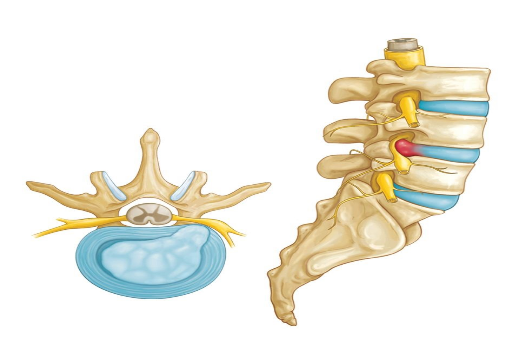
The intervertebral disc is a crucial component of the spine, playing a vital role in supporting spinal motion, providing stability, and contributing to the overall height of the spinal column. Comprised of two main parts, the annulus fibrosus and the nucleus pulposus, the intervertebral disc serves as a link between adjacent vertebral bodies, enabling smooth and controlled movement of the spine.
Function:
- Allows Spinal Motion and Provides Stability: One of the primary functions of the intervertebral disc is to facilitate spinal motion. The disc acts as a cushion between vertebrae, allowing for flexibility and mobility of the spine while also providing stability and support.
- Links Adjacent Vertebral Bodies Together: The intervertebral disc acts as a link between adjacent vertebral bodies, helping to maintain proper alignment of the spine and distribute the forces exerted on the spine during various activities such as walking, running, or lifting.
- Responsible for 25% of Spinal Column Height: The intervertebral disc contributes significantly to the height of the spinal column. It accounts for approximately 25% of the overall height of the spinal column, highlighting its importance in maintaining proper spinal alignment and function.
Parts:
- Annulus Fibrosus: The annulus fibrosus is the tough, outer layer of the intervertebral disc. It is made up of strong, fibrous tissue that surrounds and encases the softer inner core, providing strength and stability to the disc. The annulus fibrosus also helps to contain the nucleus pulposus and maintain the overall shape of the disc.
- Nucleus Pulposus: The nucleus pulposus is the soft, gel-like inner core of the intervertebral disc. It is primarily composed of water and proteoglycans, which give it its gel-like consistency and ability to absorb shock and distribute pressure evenly across the disc. The nucleus pulposus also helps to maintain the flexibility and resilience of the disc.
In conclusion, the intervertebral disc is a critical structure in the spine, responsible for supporting spinal motion, providing stability, and contributing to the overall height of the spinal column. Understanding the anatomy and function of the intervertebral disc can help individuals maintain a healthy spine and prevent or manage spinal conditions related to disc degeneration or injury.
Understanding Lumbar Disc Herniation: A Comprehensive Overview:
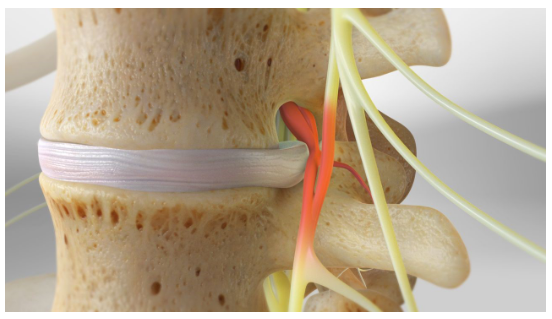
Lumbar disc herniation is a common spinal condition characterized by the displacement of the inner core of the intervertebral disc, known as the nucleus pulposus, through its outer fibrous ring, called the annulus fibrosus. This displacement typically occurs in the posterolateral region of the disc and can lead to compression and irritation of the lumbar nerve roots and the dural sac, resulting in the characteristic pain known as sciatica.
Mechanism of Lumbar Disc Herniation: The intervertebral discs serve as cushions between the vertebrae, providing flexibility and absorbing shock during spinal movements. With age or injury, the discs may degenerate or weaken, making them more susceptible to herniation. When the nucleus pulposus herniates through the annulus fibrosus, it can press against nearby structures, such as the nerve roots or the dural sac, leading to pain, numbness, or weakness in the lower back, buttocks, legs, or feet.
Clinical Presentation: The symptoms of lumbar disc herniation can vary depending on the location and severity of the herniation. Common symptoms include:
- Sharp or shooting pain in the lower back, buttocks, thighs, or legs (sciatica)
- Numbness or tingling sensation in the legs or feet
- Weakness in the legs or difficulty in walking
- Pain that worsens with certain movements, such as bending, lifting, or sitting for long periods
Diagnosis and Treatment: Diagnosing lumbar disc herniation typically involves a physical examination to assess the range of motion, reflexes, and muscle strength, along with imaging tests such as X-rays, MRI, or CT scans to visualize the herniated disc and its effects on the surrounding structures.
Treatment options for lumbar disc herniation aim to relieve pain, reduce inflammation, and improve mobility. Mild cases can often be managed with rest, physical therapy, and pain medications. In more severe cases where conservative treatments fail to provide relief, corticosteroid injections or surgical procedures such as discectomy may be recommended to remove or repair the herniated disc.
Prevention and Lifestyle Modifications: To prevent lumbar disc herniation, it is essential to maintain a healthy lifestyle, including regular exercise to strengthen the back muscles and maintain a healthy weight. Additionally, practicing proper lifting techniques and avoiding prolonged sitting or standing can help reduce the risk of disc herniation.
In conclusion, lumbar disc herniation is a common spinal condition that can cause significant pain and discomfort. Understanding the mechanism, symptoms, and treatment options can help individuals manage the condition effectively and improve their quality of life. If you suspect you have lumbar disc herniation, it is important to consult with a healthcare professional for proper diagnosis and personalized treatment plan.
Understanding Sciatica: Symptoms, Causes, and Treatment:
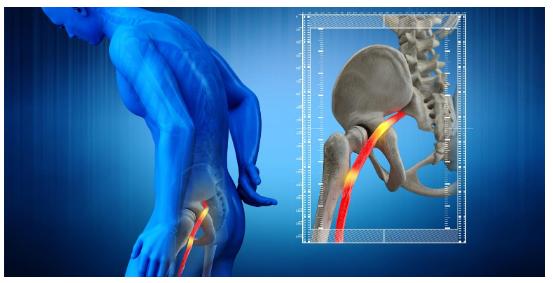
Sciatica is a condition characterized by pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. The pain can vary widely, from a mild ache to a sharp, burning sensation or excruciating discomfort. Sometimes it can feel like a jolt or electric shock. It can be worsened by coughing, sneezing, or sitting for long periods.
Symptoms of Sciatica: The hallmark of sciatica is pain that radiates from your lower back to your buttock and down the back of your leg. You might also feel numbness, tingling, or weakness in your leg or foot. Sciatica usually affects only one side of your body.
Causes of Sciatica: Sciatica occurs when the sciatic nerve is compressed or irritated. This can happen for a variety of reasons. Some common causes include:
- Herniated or bulging discs: The most common cause of sciatica is a herniated disc in the spine pressing against the nerve roots that lead to the sciatic nerve.
- Spinal stenosis: This condition causes the spinal canal to become narrower over time, putting pressure on the nerves, including the sciatic nerve.
- Degenerative disc disease: As we age, our spinal discs can degenerate and lose their cushioning ability, leading to irritation of the nerves.
- Spondylolisthesis: This is a condition in which one vertebra slips forward over another, putting pressure on the nerves in the lower back.
- Piriformis syndrome: The piriformis muscle in the buttocks can sometimes irritate the sciatic nerve if it spasms or tightens.
Diagnosis and Treatment of Sciatica: Diagnosing sciatica usually involves a physical examination and a review of your symptoms. Imaging tests like X-rays, MRI, or CT scans may be ordered to confirm the diagnosis and identify the underlying cause.
Treatment for sciatica often involves a combination of self-care measures and medical treatments. Self-care measures may include rest, hot or cold packs, and gentle stretches. Over-the-counter pain medications can help reduce pain and inflammation. In more severe cases, your doctor may recommend prescription medications or physical therapy. In very rare cases where conservative treatments fail, surgery may be considered to relieve pressure on the sciatic nerve.
Prevention of Sciatica: While it’s not always possible to prevent sciatica, there are some steps you can take to reduce your risk. These include maintaining good posture, using proper lifting techniques, staying active and exercising regularly to keep your back muscles strong and flexible, and avoiding prolonged sitting or standing in one position.
In conclusion, sciatica is a common condition that can cause significant pain and discomfort. Understanding the symptoms, causes, and treatment options can help you manage the condition effectively and improve your quality of life. If you’re experiencing symptoms of sciatica, it’s important to see your healthcare provider for a proper diagnosis and treatment plan.
Understanding Sciatica: Key Facts and Prevention Tips
Sciatica is a condition characterized by pain that radiates along the path of the sciatic nerve, which is the longest and widest nerve in the body. It originates in the lower back and extends through the buttocks to the lower leg. Here are some important facts about sciatica and tips for prevention:
- Anatomy of the Sciatic Nerve: The sciatic nerve is the longest and widest nerve in the human body. It originates from nerve roots in the lumbar spine and sacral region of the spine and extends down the back of each leg. It provides sensation to the skin of the foot and controls the muscles of the back of the knee and lower leg.
- Common Symptoms and Presentation: The most common initial complaint of sciatica is lower back pain. As the condition progresses, individuals may experience pain, numbness, tingling, or weakness in one leg. It typically affects only one side of the body, with more intense lower back pain on the same side as the leg symptoms.
- Causes of Sciatica: Sciatica can be caused by various factors, including pregnancy, disc herniation, excess weight, and even habits like keeping a large wallet in the back pocket. Weakening of the body due to poor nutrition and lack of exercise is also a significant contributing factor.
- Prevention of Sciatica: The best way to prevent sciatica is to maintain an active lifestyle and eat a healthy diet. Regular exercise helps strengthen the muscles that support the spine, reducing the risk of nerve compression. Eating a diet rich in fruits, vegetables, whole grains, legumes, and healthy fats provides essential nutrients that support overall health and spinal health.
In conclusion, sciatica is a common condition that can cause significant pain and discomfort. Understanding the anatomy of the sciatic nerve, common symptoms, and causes can help individuals take preventive measures. By staying active, eating healthy, and maintaining a strong body, you can reduce your risk of developing sciatica and enjoy a better quality of life. If you experience symptoms of sciatica, it is important to consult with a healthcare professional for proper diagnosis and treatment.
Understanding Sciatica Symptoms: Pain, Numbness, and Mobility Issues:
Sciatica is a condition characterized by pain that radiates along the path of the sciatic nerve, which runs from the lower back through the hips and buttocks and down each leg. The symptoms of sciatica can vary in intensity and presentation, but common signs include:
- Lower Back Pain and Leg Pain: The most common symptom of sciatica is pain. This pain can vary from a dull ache to a sharp, shooting sensation. It typically starts in the lower back and radiates down the back of one leg. The pain can be intense and debilitating, making it difficult to sit, stand, or walk for long periods.
- Burning, Tingling, and Numbness: In addition to pain, individuals with sciatica may experience sensations of burning, tingling, or numbness in the affected leg. These sensations can be constant or intermittent and may worsen with certain movements or positions.
- Walking Difficulty: The pain and numbness associated with sciatica can make walking difficult. Some individuals may experience weakness or a “heavy” feeling in the affected leg, making it challenging to lift or move the leg properly.
- Difficulty Standing Up: Sciatica can also cause difficulty in standing up from a seated position. The pain and stiffness in the lower back and leg can make it hard to straighten the back and bear weight on the affected leg, leading to difficulty in standing up.
Sciatica can cause a range of symptoms, including pain, numbness, and mobility issues. Understanding these symptoms is crucial for early diagnosis and treatment. If you experience any of these symptoms, it is important to consult with a healthcare professional for proper evaluation and management. Treatment for sciatica often includes a combination of self-care measures, physical therapy, and medications to alleviate pain and improve mobility. In some cases, surgery may be recommended to relieve pressure on the sciatic nerve.
Understanding the Risk Factors for Sciatica:
Sciatica, a condition characterized by pain radiating along the path of the sciatic nerve, can significantly impact one’s quality of life. While the exact cause of sciatica can vary, several risk factors have been identified that may increase the likelihood of developing this condition. Understanding these risk factors is crucial for prevention and early intervention.
- Strenuous Activities or Heavy Lifting: Engaging in activities that require heavy lifting or strenuous exertion can put pressure on the spine and increase the risk of developing sciatica. It is important to use proper lifting techniques and take regular breaks to avoid excessive strain on the back.
- Cigarette Smoking: Smoking is known to have detrimental effects on overall health, including the spine. It can lead to decreased blood flow and oxygen supply to the spinal discs, which may increase the risk of disc degeneration and herniation, contributing to sciatica.
- Obesity: Excess weight can put additional pressure on the spine and contribute to the compression of the sciatic nerve. Maintaining a healthy weight through proper diet and regular exercise is essential for reducing the risk of developing sciatica.
- Old Age: As we age, the spine undergoes natural degenerative changes, such as the narrowing of the spinal canal and the formation of bone spurs. These age-related changes can increase the risk of developing sciatica in older adults.
- Prolonged Sitting: Sitting for long periods, especially with poor posture, can put pressure on the lower back and lead to muscle stiffness and imbalances. This can contribute to the development or exacerbation of sciatica symptoms.
- Diabetes: Diabetes is associated with nerve damage, known as diabetic neuropathy, which can affect the sciatic nerve. Proper management of diabetes is important for reducing the risk of nerve damage and related complications.
- Inactive Lifestyle: Lack of regular physical activity can lead to weak muscles and poor flexibility, increasing the risk of back injuries and sciatica. Incorporating regular exercise into your routine can help strengthen the muscles that support the spine and reduce the risk of sciatica.
While these risk factors can increase the likelihood of developing sciatica, it is important to note that not everyone with these risk factors will develop the condition. Taking proactive steps to maintain a healthy lifestyle, including regular exercise, proper lifting techniques, and avoiding smoking, can help reduce the risk of developing sciatica and promote overall spinal health.
Understanding the Diagnosis and Examinations for Sciatica:
Diagnosing sciatica involves a thorough examination of the patient’s symptoms and physical condition. Several key examinations are commonly performed to assess the severity and underlying cause of sciatic pain.
- Physical Examination: A comprehensive physical examination is essential for evaluating sciatica. This includes observing the patient’s posture and gait, palpating the spine and surrounding muscles for tenderness or abnormalities, and assessing the range of motion of the spine. A root tension test may also be conducted to evaluate the tension in the affected nerve roots.
- Straight Leg Raising Test (Lasègue Sign): This test is a hallmark examination for sciatica. It involves raising the patient’s leg while keeping it straight. The test is considered positive if the patient experiences pain that radiates down the leg when the affected leg is raised. This indicates irritation or compression of the L5 or S1 nerve roots, which are commonly affected in sciatica.
- Neurological Evaluation: Assessing the neurological status of the lower limbs is crucial for diagnosing sciatica. This includes testing muscle strength, reflexes, and sensation in the legs to determine if there is any nerve damage or compression affecting the function of the sciatic nerve.
- Imaging Studies: In some cases, imaging studies such as X-rays, MRI scans, or CT scans may be recommended to visualize the spine and identify any structural abnormalities, such as herniated discs, bone spurs, or narrowing of the spinal canal, that may be causing sciatic nerve compression.
- Electrodiagnostic Tests: Nerve conduction studies or electromyography (EMG) may be performed to assess the electrical activity of the nerves and muscles, which can help identify the location and severity of nerve compression or damage in sciatica.
- Other Examinations: Depending on the suspected cause of sciatica, additional examinations such as blood tests or specialized tests for conditions like diabetes or infections may be necessary to rule out underlying medical conditions contributing to sciatic nerve pain.
Diagnosing sciatica requires a comprehensive approach that considers the patient’s symptoms, physical examination findings, and any relevant imaging or diagnostic tests. By accurately diagnosing the underlying cause of sciatic pain, healthcare providers can develop an appropriate treatment plan to relieve symptoms and improve the patient’s quality of life.
Clinical Tests for Sciatica: Understanding Nerve Root Dysfunction:
Diagnosing sciatica involves not only identifying the presence of symptoms but also pinpointing the specific nerve root that may be affected. Several clinical tests are commonly used to assess nerve root dysfunction in patients with sciatica.
- Dorsiflexion Strength Test: This test evaluates the strength of the ankle and big toe dorsiflexion, which is primarily controlled by the L5 nerve root. Weakness in dorsiflexion can indicate dysfunction or compression of the L5 nerve root, which is commonly affected in cases of sciatica.
- Ankle Reflex Test: Testing the ankle reflex can help assess the function of the S1 nerve root. Diminished or absent ankle reflexes may suggest dysfunction of the S1 nerve root, which is another common site of compression in sciatica.
- Light Touch Sensation Test: Sensory testing is important for evaluating nerve function in sciatica. Testing the sensation in specific areas of the toe can help localize the nerve root affected. Light touch sensation in the medial aspect of the toe corresponds to the L4 nerve root, the dorsal aspect to the L5 nerve root, and the lateral aspect to the S1 nerve root. Abnormalities in sensation in these areas can indicate dysfunction of the corresponding nerve roots.
These tests are valuable tools for healthcare providers in diagnosing sciatica and determining the underlying cause of nerve root dysfunction. By identifying the specific nerve root affected, healthcare providers can tailor treatment plans to address the root cause of the problem and provide targeted relief for patients with sciatica.
Diagnostic Investigations for Sciatica: Understanding Your Options:
When it comes to diagnosing sciatica and identifying the underlying cause of your symptoms, healthcare providers have several investigative tools at their disposal. These tests help provide a clearer picture of the condition of your spine and nerves, aiding in an accurate diagnosis and effective treatment plan.

- MRI (Magnetic Resonance Imaging): This imaging technique is often considered the most helpful investigation for diagnosing sciatica. An MRI scan can provide detailed images of the spinal cord, nerve roots, and surrounding structures, allowing healthcare providers to identify any abnormalities such as herniated discs, spinal stenosis, or nerve compression that may be causing your sciatic pain.
- CT Scan (Computed Tomography Scan): While not as commonly used as MRI, a CT scan can also be useful in diagnosing sciatica, especially when MRI is not feasible or inconclusive. CT scans provide detailed images of the bones and can help identify bony abnormalities, such as bone spurs or fractures, that may be contributing to your symptoms.
- X-ray: Although X-rays do not show soft tissues like discs or nerves, they can be used to assess the alignment of the spine and look for any signs of degeneration, such as the loss of normal lordosis (the natural curve of the spine). X-rays are often used as a preliminary investigation to rule out other potential causes of back pain before more advanced imaging is considered.
These investigative tools play a crucial role in diagnosing sciatica and guiding treatment decisions. Your healthcare provider will determine which tests are most appropriate based on your symptoms, medical history, and physical examination findings. By obtaining an accurate diagnosis, you can receive the most effective treatment to alleviate your sciatic pain and improve your quality of life.
Managing Sciatica: Options for Relief and Recovery:
Sciatica, characterized by pain radiating along the sciatic nerve, can be debilitating. However, effective management strategies can help alleviate symptoms and improve quality of life. Here are some common approaches to managing sciatica:
1. Conservative Management: In many cases, sciatica can be managed without surgery. Conservative treatments aim to relieve pain and promote healing through non-invasive methods. These may include:
- Pain Medications: Over-the-counter pain relievers such as ibuprofen or acetaminophen may help reduce pain and inflammation.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and inflammation.
- Physical Therapy: A structured physical therapy program can help strengthen muscles, improve flexibility, and reduce pressure on the sciatic nerve.
- Activity Modification: Avoiding activities that worsen symptoms and adopting a more back-friendly posture can help alleviate pain.
2. Management through Physiotherapy and Exercise: Physiotherapy plays a crucial role in managing sciatica. A physiotherapist can design a customized exercise program to strengthen the muscles supporting the spine, improve flexibility, and reduce pressure on the sciatic nerve. Regular exercise can also help manage weight, which is beneficial for reducing the strain on the spine.
3. Management through Naturopathy: Naturopathy offers a holistic approach to managing sciatica, focusing on natural remedies and lifestyle modifications. Some naturopathic treatments that may be beneficial include:
- Herbal Remedies: Certain herbs such as turmeric, ginger, and devil’s claw have anti-inflammatory properties that may help reduce sciatic pain.
- Acupuncture: This traditional Chinese therapy involves inserting thin needles into specific points on the body to alleviate pain and promote healing.
- Nutritional Counseling: A balanced diet rich in anti-inflammatory foods can help reduce inflammation and support overall spinal health.
4. Surgical Management: Surgery is usually considered when conservative treatments fail to provide relief or if there is progressive neurological deficit. Surgical options for sciatica may include:
- Microdiscectomy: A minimally invasive procedure to remove the portion of a herniated disc that is pressing on the nerve.
- Laminectomy: A surgical procedure to remove the lamina (back part of the vertebra) to relieve pressure on the nerve roots.
- Spinal Fusion: In cases of severe spinal instability, spinal fusion may be performed to stabilize the spine and reduce pain.
Managing sciatica often requires a combination of approaches tailored to the individual’s specific condition and needs. Consulting with healthcare professionals, including physiotherapists, naturopaths, and orthopedic surgeons, can help determine the most appropriate management plan for optimal relief and recovery.
Conservative Management of Sciatica: A Comprehensive Approach to Relief:
When it comes to managing sciatica, conservative treatments are often the first line of defense. These non-invasive strategies aim to relieve pain, promote recovery, and prevent further complications. Here’s a closer look at how healthcare providers approach conservative management and the medications that may be prescribed:
Aims of Conservative Management:
- Relieve Pain: The primary goal of conservative management is to alleviate the pain associated with sciatica, which can be sharp, shooting, or burning in nature.
- Promote Recovery: Conservative treatments also aim to facilitate healing of the affected nerve roots and surrounding tissues.
- Prevent Further Complications: By addressing the underlying cause of sciatica and promoting proper spinal health, conservative management aims to prevent the condition from worsening or leading to long-term complications.
Medication Options: Healthcare providers may prescribe medications to help manage pain and inflammation associated with sciatica. These medications are typically prescribed in a stepwise approach, starting with milder options and progressing to stronger medications if needed. The four steps often include:
- Paracetamol (Acetaminophen): This over-the-counter medication is commonly used to relieve mild to moderate pain. It is often the first-line medication for sciatica.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs such as ibuprofen or naproxen can help reduce inflammation and relieve pain. They are often used if paracetamol alone is not sufficient.
- Tramadol, Paracetamol, or NSAID in Combination with Codeine: In cases where pain is more severe, healthcare providers may prescribe medications that combine tramadol, paracetamol, or an NSAID with codeine, which is a stronger pain reliever.
- Morphine: Morphine is a potent opioid medication that may be prescribed for severe pain that does not respond to other treatments. It is typically used for short periods and under close supervision due to the risk of dependence and side effects.
Important Considerations:
- Individualized Treatment: The choice of medication and treatment plan should be tailored to each patient’s specific needs and medical history.
- Short-Term Use: Medications should be used for the shortest duration possible to manage symptoms effectively.
- Monitor for Side Effects: Patients should be monitored for side effects and complications associated with medication use, especially with opioids like morphine.
Conservative management of sciatica can be highly effective in relieving pain and promoting recovery. However, it is essential to work closely with healthcare providers to develop a comprehensive treatment plan that addresses your specific needs and ensures the best possible outcome.
Physiotherapy and Exercise: Key Components of Sciatica Management:

For individuals suffering from sciatica, physiotherapy and targeted exercises play a pivotal role in alleviating pain, improving mobility, and enhancing overall quality of life. These interventions are designed to address the root causes of sciatic pain and restore function to the affected areas. Here’s a closer look at how physiotherapy and exercise can help manage sciatica:
Goals of Physiotherapy and Exercise:
- Restore Pain-Free Functional Movement Patterns: Physiotherapy focuses on restoring normal movement patterns, reducing pain during daily activities such as walking, bending, and lifting.
- Relieve Pain: By targeting specific muscles and tissues, physiotherapy aims to alleviate pain in the lower back, buttock, thigh, and leg.
- Reduce Muscle Spasm: Through targeted exercises and manual therapy, physiotherapy helps reduce muscle spasms that may be contributing to sciatic pain.
- Restore Function of the Lumbar Spine and Sacroiliac Joint: Physiotherapy helps improve the function of the lumbar spine and sacroiliac joint, which are often affected in cases of sciatica.
- Improve Mobility of the Lower Body: Specific exercises and stretches are prescribed to improve the flexibility and mobility of the lower body, reducing stiffness and discomfort.
- Foster a Better Healing Environment: Physiotherapy techniques such as ultrasound and electrical stimulation can help create a conducive environment for healing in the lower back.
- Promote Neurologic Adaptations: Physiotherapy promotes neurologic adaptations that reduce the perception of pain, helping individuals manage their symptoms more effectively.
- Prevent Future Pain Flare-Ups: Through education and personalized exercise programs, physiotherapy helps individuals prevent future episodes of sciatic pain.
- Reduce Fear Associated with Movement: By gradually reintroducing movement and activity, physiotherapy helps reduce fear and anxiety associated with pain, empowering individuals to regain control of their lives.
Tailored Treatment Plans: Physiotherapy and exercise programs are tailored to each individual’s specific needs and may include a combination of stretching, strengthening, aerobic conditioning, and manual therapy techniques. These programs are designed to be progressive, starting with gentle exercises and gradually increasing intensity as tolerance improves.
Physiotherapy and exercise are essential components of sciatica management, offering a safe and effective way to reduce pain, improve function, and prevent future episodes. By working closely with a physiotherapist, individuals can regain mobility, reduce pain, and enjoy a better quality of life.
Effective Protocols for Managing Sciatica: A Comprehensive Approach:
When it comes to managing sciatica, a multifaceted approach that combines various treatment modalities can be highly effective. Here are some key protocols that healthcare providers often use to address sciatic pain and promote recovery:
- Muscle Strengthening Exercises: Strengthening the muscles supporting the spine can help improve posture, reduce pressure on the sciatic nerve, and enhance overall spinal health. Exercises targeting the core, back, and lower body muscles are typically included in a comprehensive exercise program.
- McKenzie Method: This specialized form of physical therapy focuses on self-directed exercises and postural changes to alleviate pain and restore function. The McKenzie Method aims to centralize or reduce radiating pain by guiding the patient through specific movements and positions.
- Transcutaneous Electrical Nerve Stimulation (TENS): TENS therapy involves the use of a small device that delivers low-voltage electrical impulses to the affected area. This can help reduce pain by disrupting or blocking pain signals sent to the brain.
- Traction: Traction therapy involves gently stretching the spine to relieve pressure on the discs and nerves. This can help reduce pain and improve mobility, particularly in cases of disc herniation or spinal stenosis.
- Cryotherapy: Cold therapy, or cryotherapy, involves applying ice or cold packs to the affected area to reduce inflammation and numb the pain. This can help alleviate sciatic pain and promote healing.
- Shortwave Diathermy: This form of heat therapy uses electromagnetic energy to generate deep heat within tissues. Shortwave diathermy can help improve blood flow, reduce muscle spasms, and alleviate pain in sciatica.
- Ultrasound: Therapeutic ultrasound uses high-frequency sound waves to generate heat deep within tissues. This can help improve circulation, reduce inflammation, and promote healing in the affected area.
Combining Modalities for Optimal Results: In many cases, a combination of these protocols is used to address sciatica comprehensively. For example, a treatment plan may include muscle strengthening exercises along with TENS therapy and cryotherapy to reduce pain and improve function. The specific protocols used will depend on the individual’s symptoms, severity of the condition, and response to treatment.
Consultation with Healthcare Providers: It’s important for individuals with sciatica to work closely with their healthcare providers to develop a tailored treatment plan that addresses their specific needs. By combining various protocols and modalities, healthcare providers can help individuals manage their symptoms effectively and improve their quality of life.
Naturopathy and Yoga: Holistic Approaches to Sciatica Management:
Naturopathy and yoga offer holistic and natural approaches to managing sciatica, focusing on restoring balance to the body and promoting overall well-being. These practices emphasize the body’s innate ability to heal itself and can be effective in alleviating pain and improving mobility. Here are some key components of naturopathic and yogic approaches to managing sciatica:

- Hydrotherapy: Hydrotherapy involves the therapeutic use of water in various forms, such as hot and cold compresses, baths, and wraps. Hydrotherapy can help reduce inflammation, relax muscles, and improve circulation, which can all contribute to relieving sciatic pain.
- Acupuncture: Acupuncture is a traditional Chinese therapy that involves the insertion of thin needles into specific points on the body to stimulate energy flow and promote healing. Acupuncture can help alleviate pain and reduce inflammation associated with sciatica.
- Nutrition and Diet: A healthy diet rich in anti-inflammatory foods can help reduce inflammation and support the body’s natural healing processes. Naturopaths often recommend a diet high in fruits, vegetables, whole grains, and lean proteins, while avoiding processed foods and sugars.
- Mud Therapy: Mud therapy, also known as peloid therapy, involves the application of mud or clay packs to the affected area. Mud therapy can help reduce pain, inflammation, and muscle spasms, while also improving circulation and promoting detoxification.
- Yoga Therapy: Yoga offers gentle stretching and strengthening exercises that can help improve flexibility, reduce muscle tension, and alleviate sciatic pain. Yoga poses such as the pigeon pose, cobra pose, and seated spinal twist are often recommended for sciatica.
Integrating Naturopathy and Yoga into Your Routine: To benefit from naturopathy and yoga for sciatica, it’s important to work with qualified practitioners who can tailor a treatment plan to your specific needs. They can help you incorporate these practices into your daily routine and make lifestyle changes that support your overall health and well-being.
Combining Therapies for Optimal Results: While naturopathy and yoga can be effective on their own, they can also complement conventional treatments such as medication or physical therapy. By combining these approaches, you can create a comprehensive treatment plan that addresses the underlying causes of sciatica and promotes healing from multiple angles.
In conclusion, naturopathy and yoga offer safe and natural ways to manage sciatica, focusing on holistic healing and promoting overall health. By incorporating these practices into your routine, you can reduce pain, improve mobility, and enhance your quality of life.
Hydrotherapy: Using Water for Sciatica Relief:
Hydrotherapy, or water therapy, is a natural and effective way to manage sciatica pain and promote healing. This therapeutic approach utilizes the properties of water, such as temperature and pressure, to provide relief and improve overall well-being. Here’s a closer look at how hydrotherapy can benefit individuals with sciatica:
Spinal Spray or Lumbar Spray: One of the key benefits of hydrotherapy is its ability to influence the central nervous system and vasomotor nerves, which can have a positive effect on the body as a whole. Spinal or lumbar sprays involve the application of water jets or sprays directly to the affected area, such as the lower back or lumbar region. This gentle massage action can help relax muscles, reduce pain, and improve circulation, which are all beneficial for relieving sciatica symptoms.
Heat and Cold Packs: Heat and cold packs are commonly used in hydrotherapy to help manage sciatica pain. Here’s how each type of pack can provide relief:
- Heat Packs: Heat packs can help relieve pain by reducing muscle stiffness and increasing blood flow. The heat from these packs helps dilate blood vessels, improving circulation and reducing muscle tension. Heat therapy can also promote relaxation, making it easier to perform exercises or attend physical therapy sessions.
- Cold Packs: Cold packs, on the other hand, can help reduce pain and swelling by causing a numbing effect. These packs constrict the blood vessels beneath the skin, reducing blood flow to the affected area and decreasing inflammation. Cold therapy can also slow down the chemical reactions that cause pain, providing relief from sciatica symptoms.
Incorporating Hydrotherapy into Your Treatment Plan: Hydrotherapy can be a valuable addition to your sciatica treatment plan, especially when used in conjunction with other therapies such as physical therapy, medication, and lifestyle modifications. Before starting any hydrotherapy regimen, it’s important to consult with a healthcare professional to ensure that it is safe and appropriate for your individual needs.
Conclusion: Hydrotherapy offers a natural and effective way to manage sciatica pain and promote healing. Whether through spinal sprays or the use of heat and cold packs, hydrotherapy can provide relief and improve your overall quality of life. Consider incorporating hydrotherapy into your treatment plan to experience the benefits for yourself.
Acupuncture for Sciatica Relief: A Natural Approach to Pain Management:
Acupuncture, an ancient Chinese therapy, has been used for centuries to relieve pain and promote healing. This holistic approach to healthcare is based on the principle of stimulating specific points on the body, known as acupoints, to restore balance and improve the flow of energy, or Qi, throughout the body. When it comes to sciatica, acupuncture has shown promising results in providing relief from pain and discomfort associated with this condition.
How Acupuncture Works: Acupuncture is believed to stimulate blood circulation at corresponding acupoints, which helps relieve pain. This mechanism is also thought to be the basis for acupuncture’s effectiveness in treating pain caused by lumbar disc herniation (LDH), a common cause of sciatica. By targeting specific acupoints along the meridians, or energy pathways, acupuncture can help reduce inflammation, relax muscles, and improve nerve function, all of which can contribute to alleviating sciatic pain.
Selected Acupoints for Sciatica: When it comes to treating sciatica with acupuncture, several acupoints are commonly targeted to provide relief. These acupoints are carefully selected based on their location and their ability to influence the flow of Qi in the body. Some of the acupoints commonly used for sciatica include:
- Shenshu (BL23)
- Qihaishu (BL24)
- Dachangshu (BL25)
- Guanyuanshu (BL26)
- Huantiao (GB30)
- Huanzhong (Extra35)
- Chengfu (BL36)
- Yinmen (BL37)
- Weizhong (BL40)
- Chengshan (BL57)
- Kunlun (BL60)
These acupoints are typically used on both sides of the body to maximize the therapeutic effect of acupuncture.
Incorporating Acupuncture into Your Sciatica Treatment Plan: If you’re considering acupuncture for sciatica relief, it’s important to consult with a qualified acupuncturist who can assess your condition and develop a treatment plan tailored to your specific needs. Acupuncture is generally safe when performed by a trained practitioner and can be used in conjunction with other therapies, such as physical therapy and medication, to enhance its effectiveness.
Conclusion: Acupuncture offers a natural and effective way to manage sciatica pain and improve overall well-being. By targeting specific acupoints, acupuncture can help relieve pain, reduce inflammation, and promote healing, providing a holistic approach to sciatica treatment. Consider exploring acupuncture as part of your sciatica management plan to experience its potential benefits firsthand.
A Day in the Life of a Sciatica Management Plan:
Managing sciatica involves a comprehensive approach that includes not only physical therapies but also a well-balanced diet and lifestyle changes. Here’s a detailed breakdown of a daily schedule that incorporates diet, yoga therapy, hydrotherapy, and acupuncture to help manage sciatic pain and promote healing:
6:30 am – Breakfast: Start your day with a nutritious breakfast that includes plantain pith juice, ash gourd juice, or lemon juice (250 mL). These juices are known for their detoxifying and anti-inflammatory properties, which can help reduce inflammation and promote healing.
9:00 am – Mid-Morning Snack: Enjoy a variety of fruits such as papaya, guava, banana, and orange (100 g). Pair this with green gram or groundnut sprouts (50 g) for added protein and fiber. Include vegetables like bottle gourd, cucumber, carrot, and beetroot (100 g) for added nutrients and antioxidants.
12:00 pm – Lunch: For lunch, have a refreshing carrot, grapes, or watermelon juice (250 mL). These juices are not only hydrating but also rich in vitamins and minerals that support overall health and healing.
1:30 pm – Afternoon Snack: Continue with your fruit intake with another serving of papaya, guava, banana, and orange (100 g). Pair this with green gram or groundnut sprouts (50 g) for a balanced and nutritious snack.
4:30 pm – Evening Snack: Stay hydrated with lemon juice or curry leaves juice (250 mL). These juices can help detoxify the body and reduce inflammation. Follow this up with another serving of fruits and vegetables (100 g each) to keep you energized until dinner.
7:00 pm – Dinner: For dinner, stick to a light and healthy meal consisting of fruits (papaya, guava, banana, and orange – 100 g each) and vegetables (bottle gourd, cucumber, carrot, and beetroot – 100 g each). This combination provides essential nutrients and fiber without being too heavy on the stomach.
Treatment Plan:
- Yoga Therapy: Incorporate specific yoga poses such as Tadasana, Ardha Katichakrasana, Ardha Chakrasana, and Supta Udharakarshasana to improve flexibility, reduce muscle tension, and relieve sciatic pain.
- Yogic Breathing: Practice Nadi Shodhana Pranayama to promote relaxation and reduce stress, which can exacerbate sciatic pain.
- Relaxations: Include deep relaxation techniques and Yoga Nidra to help calm the mind and body, facilitating healing and pain relief.
- Hydrotherapy: Incorporate mud packs on the abdomen and eyes, as well as steam baths, to improve circulation, reduce inflammation, and promote relaxation.
- Acupuncture: Receive bilateral needling at specific acupoints such as UB-40, GV-6, UB-30, Sp-6, Liv-13, SI-11, K-3, GB-30, and GB-31. This can help stimulate blood circulation, reduce pain, and promote healing.
- Meridian Massage: Focus on the Kidney channel and Back Shu points to further stimulate circulation and relieve tension in the muscles and nerves.
Conclusion: A holistic approach that combines a nutritious diet, regular exercise, and targeted therapies such as yoga, hydrotherapy, and acupuncture can help manage sciatica effectively. It’s important to consult with healthcare professionals before starting any new treatment regimen to ensure it is safe and appropriate for your individual needs.
Understanding Muscular Dystrophy: Causes, Symptoms, and Clinical Features
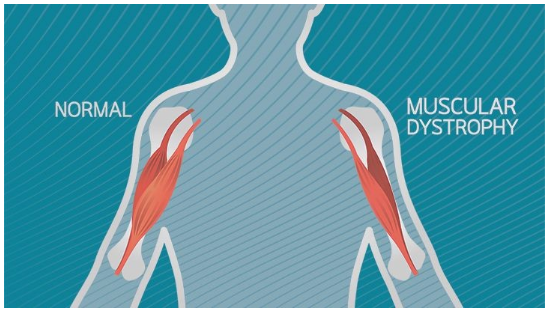
Muscular dystrophy is a group of genetic disorders characterized by progressive muscle weakness and degeneration. It is caused by defects in muscle proteins, leading to the death of muscle cells and tissues. One of the most well-known forms of muscular dystrophy is Duchenne muscular dystrophy, named after the French neurologist Guillaume Duchenne, who first identified the condition.
Genetic Basis: Muscular dystrophy is primarily an autosomal dominant disorder, meaning that the defective gene responsible for the condition is located on one of the autosomal chromosomes (non-sex chromosomes) and only one copy of the gene is sufficient to cause the disease. However, some forms of muscular dystrophy can be autosomal recessive, requiring two copies of the defective gene (one from each parent) to manifest the disease.
Clinical Features: The clinical features of muscular dystrophy vary depending on the specific type and severity of the condition. Common symptoms include:
- Progressive Muscular Wasting: Muscles gradually weaken and decrease in size over time.
- Poor Balance: Difficulty maintaining balance and coordination.
- Atrophy: Muscles may appear smaller and weaker than normal.
- Scoliosis: Curvature of the spine and back, which can lead to postural abnormalities.
- Inability to Walk: As the disease progresses, individuals may lose the ability to walk and require mobility aids.
- Frequent Falls: Weakness and instability can lead to frequent falls.
- Waddling Gait: A characteristic walking pattern where the hips sway from side to side.
- Calf Deformation: Muscles in the calf area may become enlarged or deformed.
- Limited Range of Movement: Reduced flexibility and range of motion in affected muscles.
- Respiratory Difficulty: Weakness in the muscles involved in breathing can lead to respiratory problems.
- Muscle Spasms: Involuntary muscle contractions and spasms may occur.
- Cowers Sign: Difficulty rising from a seated position without using the arms for support.
Management and Treatment: Currently, there is no cure for muscular dystrophy. Treatment focuses on managing symptoms, slowing disease progression, and improving quality of life. This may include physical therapy, assistive devices (such as braces or wheelchairs), respiratory support, and medications to manage symptoms and complications.
Conclusion: Muscular dystrophy is a complex group of genetic disorders that affect muscle function and strength. While there is no cure, early diagnosis and management can help improve outcomes and quality of life for individuals living with muscular dystrophy. On-going research is aimed at developing new therapies and treatments to better manage this condition.
Understanding Gower’s Sign and Causes of Muscular Dystrophy:
Gower’s Sign: Gower’s sign is a clinical indicator of weakness in the proximal muscles, particularly those of the lower limbs. It is observed when a person has to use their hands and arms to “walk” up their own body from a squatting position due to muscle weakness. This sign is commonly seen in individuals with muscular dystrophy, especially in the early stages of the disease.
Causes of Muscular Dystrophy: Muscular dystrophy is primarily a genetic disorder, meaning it is inherited from one’s parents. However, mutations in the dystrophin gene and nutritional deficits can also play a role in the development of the disease. The main cause of muscular dystrophy is the lack of muscle proteins, particularly dystrophin and the dystrophin-associated protein complex. These proteins are essential for maintaining the structure and function of muscle cells. Without them, muscle cells become weak and damaged over time, leading to the symptoms of muscular dystrophy.
Types of Muscular Dystrophy: There are several types of muscular dystrophy, each with its own genetic cause and characteristic symptoms. Duchenne muscular dystrophy (DMD) is one of the most common and severe forms of the disease, caused by mutations in the dystrophin gene. Other types include Becker muscular dystrophy, caused by mutations in the same gene but with milder symptoms, and myotonic dystrophy, caused by mutations in different genes and characterized by muscle stiffness and weakness.
Symptoms and Management: Symptoms of muscular dystrophy vary depending on the type and severity of the disease but often include progressive muscle weakness, poor balance, muscle atrophy, and difficulty walking. Treatment focuses on managing symptoms, slowing disease progression, and improving quality of life. This may include physical therapy, assistive devices, respiratory support, and medications.
Conclusion: Muscular dystrophy is a group of genetic disorders characterized by progressive muscle weakness and degeneration. Gower’s sign is a clinical indicator of muscle weakness commonly seen in individuals with muscular dystrophy. Understanding the causes and symptoms of muscular dystrophy is essential for early diagnosis and management of the disease. Ongoing research is aimed at developing new treatments and therapies to improve outcomes for individuals living with muscular dystrophy.
Diagnosis of Muscular Dystrophy: Understanding the Process:
Diagnosing muscular dystrophy involves a combination of medical tests and assessments to evaluate muscle function and genetic factors. Here’s a breakdown of the key diagnostic methods used:
- Muscle Biopsy: A muscle biopsy involves removing a small sample of muscle tissue for analysis. This procedure helps identify abnormalities in muscle structure and proteins, which are characteristic of muscular dystrophy.
- Creatine Kinase (CK) Levels: Creatine kinase is an enzyme found in muscles. Increased levels of CK in the blood can indicate muscle damage, which is often seen in muscular dystrophy. A blood test is used to measure CK levels.
- Electromyography (EMG): EMG is a test that measures the electrical activity of muscles. It can help identify abnormal muscle function and detect patterns of muscle weakness associated with muscular dystrophy.
- Electrocardiography (ECG): Since some forms of muscular dystrophy can affect the heart muscles, an ECG may be performed to assess heart function and detect any abnormalities.
- DNA Analysis: DNA analysis is a crucial diagnostic tool for muscular dystrophy, as it can identify specific genetic mutations associated with the condition. This test helps confirm the diagnosis and determine the type of muscular dystrophy present.
Importance of Early Diagnosis: Early diagnosis of muscular dystrophy is crucial for initiating appropriate treatment and management strategies. It allows healthcare providers to monitor disease progression, implement interventions to improve quality of life, and provide genetic counseling to families.
Conclusion: Diagnosing muscular dystrophy involves a comprehensive approach that includes medical history review, physical examination, and specialized tests such as muscle biopsy, CK levels, EMG, ECG, and DNA analysis. These tests help healthcare providers confirm the diagnosis, determine the type and severity of muscular dystrophy, and develop a tailored treatment plan to manage the condition effectively. Early diagnosis and intervention can significantly improve outcomes and quality of life for individuals living with muscular dystrophy.
Physical Therapy Management of Muscular Dystrophy: Strategies for Different Stages
Physical therapy plays a crucial role in managing muscular dystrophy, focusing on maximizing strength, mobility, and functional capabilities. The approach varies based on the stage of the disease, with different strategies employed for early and transitional stages.
Early Stage Management: In the early stages of muscular dystrophy, the focus is on educating the family and preventing deformities. Physical therapists work to maximize strength and functional capabilities, aiming to maintain ambulation for as long as possible. This stage involves:
- Education of Family: Providing information and guidance to family members on how to support and care for the individual with muscular dystrophy.
- Prevention of Deformity: Implementing strategies to prevent joint contractures and postural abnormalities.
- Maximizing Strength: Developing a personalized exercise program to maintain muscle strength and function.
- Functional Capabilities: Working on activities of daily living (ADLs) and mobility to enhance independence.
Transitional Stage Management: As the disease progresses, the focus shifts to managing symptoms and maintaining quality of life. Physical therapy interventions at this stage include:
- Muscle Stretching: Targeted stretching exercises for muscles prone to tightness and contractures.
- Lower Extremities Stretching: Focus on muscles like the illiotibial bands, tensor fascia lata, hip flexors, hamstrings, gastrocnemius, and posterior tibialis.
- Upper Extremities Stretching: Including the elbow flexors, forearm pronators, wrist, and finger flexors.
- PNF Techniques: Proprioceptive Neuromuscular Facilitation techniques like hold-relax to improve muscle flexibility and range of motion.
- Joint Mobilization: Gentle manipulation of joints such as the patella, elbow, and anterior and posterior movements of the tibia on the femur to improve joint mobility.
- Myofascial Release: Soft tissue therapy to relieve muscle tightness and improve muscle function.
- Moist Heat Therapy: Application of moist heat to increase tissue elasticity and reduce discomfort, with caution to avoid tissue damage.
- Positioning Training: Teaching proper positioning techniques for lying and sitting to prevent pressure ulcers and maintain comfort.
Conclusion: Physical therapy is a critical component of the management of muscular dystrophy, aiming to maintain mobility, prevent deformities, and enhance quality of life. The specific interventions and strategies employed depend on the stage of the disease and the individual’s needs. Early and consistent physical therapy can help individuals with muscular dystrophy maintain function and independence for as long as possible.
In conclusion, sciatica is a condition that affects the sciatic nerve, causing pain, numbness, and tingling sensations along its path. It is often caused by compression or irritation of the nerve roots in the lower back. Understanding the anatomy of the sciatic nerve, common symptoms, and causes of sciatica is crucial for early diagnosis and effective management.
Prevention of sciatica involves maintaining an active lifestyle, eating a healthy diet, and practicing good posture. These measures can help strengthen the muscles that support the spine and reduce the risk of nerve compression. If you experience symptoms of sciatica, such as lower back pain, leg pain, or difficulty walking, it is important to consult with a healthcare professional for proper evaluation and treatment.
By taking proactive steps to prevent sciatica and seeking timely medical attention if symptoms arise, you can effectively manage this condition and improve your quality of life.