PANCREATIC DISEASES
Understanding the Pancreas: Structure, Function, and Associated Diseases
Introduction
The pancreas is a vital glandular organ in the human body. It plays a key role in both the digestive and endocrine systems. Often overlooked compared to more prominent organs like the heart or kidneys, the pancreas is crucial in regulating body metabolism and nutrient absorption.
In this article, we will explore the anatomy of the pancreas, its essential functions, what happens when it doesn’t work properly, and the common diseases associated with it.
What Is the Pancreas?

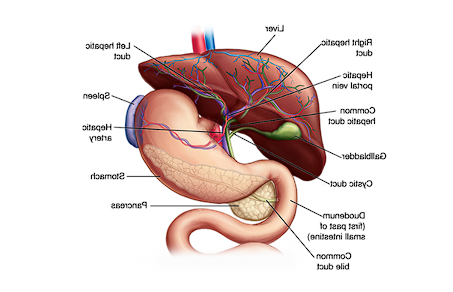
The pancreas is a glandular organ located behind the stomach, connected closely with other organs like the liver, spleen, and small intestine. It has two primary roles:
- Endocrine Function: Regulating blood sugar levels through hormones like insulin and glucagon.
- Exocrine Function: Producing digestive enzymes that break down food in the small intestine.
Anatomy of the Pancreas
The pancreas can be divided into three main parts:
- Head: The broader part connected to the duodenum of the small intestine.
- Body: The central section.
- Tail: The narrow end near the spleen.
The structure and placement of the pancreas make it integral to both digestion and metabolic regulation.
How Does the Pancreas Work?
Digestive Role (Exocrine Function)
- Produces enzymes like amylase, lipase, and proteases.
- These enzymes are released into the small intestine to break down carbohydrates, fats, and proteins.
- Without proper enzyme production, food cannot be digested or absorbed effectively.
Hormonal Role (Endocrine Function)
- Insulin: Lowers blood sugar by helping cells absorb glucose.
- Glucagon: Raises blood sugar by releasing stored glucose from the liver.
Both functions work in balance to maintain body energy levels and overall health.
Pancreatic Insufficiency
When the pancreas cannot produce enough digestive enzymes or hormones, it leads to a condition called pancreatic insufficiency.
Symptoms of Pancreatic Insufficiency:
- Poor digestion
- Nutrient malabsorption
- Weight loss despite eating
- Fatty, foul-smelling stools
- Vitamin deficiencies
Common Diseases of the Pancreas
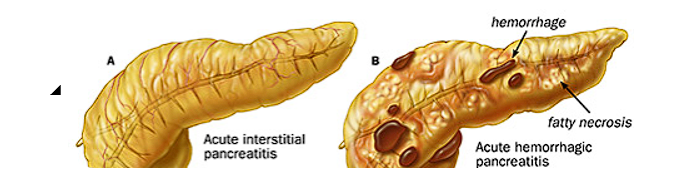
- Pancreatitis
- Acute or chronic inflammation of the pancreas.
- Causes include gallstones, alcohol abuse, and certain medications.
- Diabetes Mellitus
- Results from problems with insulin production or function.
- Leads to abnormal blood sugar levels.
- Pancreatic Cancer
- Often detected late due to subtle early symptoms.
- Risk factors include smoking, chronic pancreatitis, and family history.
- Pancreatic Insufficiency
- Covered above, this condition can be part of or separate from other diseases.
Why Digestion and Absorption Matter
As mentioned in the transcript, the quality of your nutrition depends not just on what you eat, but how well your body digests and absorbs those nutrients.
If pancreatic function is impaired:
- Even the healthiest foods may not benefit the body.
- Nutrient absorption drops, leading to deficiencies.
- Metabolism and overall health decline.
Naturopathic View on Pancreatic Health
- Diet and lifestyle adjustments play a key role in supporting pancreatic health.
- Foods that support digestive health:
- Fresh fruits like papaya and carrots
- Bland diets for initial management in acute conditions
- Juices and easily digestible foods during recovery
- Stress management and proper rest are also emphasized in naturopathic practice.
The Critical Role of Digestion and Absorption
One of the key messages about pancreatic health is that what matters isn’t only what you eat, but what you digest and absorb.
Many people consume nutritious food, but if their pancreas isn’t producing enough enzymes, the digestion and absorption of nutrients become insufficient. This condition is referred to as pancreatic insufficiency.
Why Is This Important?
- Absorption happens in the intestines. The pancreas provides the enzymes needed to break down food into nutrients that the intestines can absorb.
- If digestion fails, nutrients aren’t absorbed properly.
- This leads to nutrient deficiencies, no matter how healthy the diet is.
It’s not about food quantity or quality alone — it’s about how well your body processes it.
Pancreas Anatomy: Understanding Its Structure
Divisions of the Pancreas:
- Head: Connected to the duodenum, contains ducts like the pancreatic duct and accessory pancreatic duct.
- Body: The middle section of the pancreas.
- Tail: The part closest to the spleen.
The pancreas has several ducts and papillae (small structures) that help regulate digestive juices entering the intestines. Some important parts connected to the pancreas head include:
- Major and Minor Papillae
- Cystic Duct
- Pancreatic Duct
Size and Weight:
- Length: Approximately 6 inches (15 cm).
- Weight: Approximately 200 grams.
This organ may be small and light compared to your total body weight, but its importance is disproportionally large due to its critical functions.
Pancreatic Function and Disease Link
If the pancreas is not functioning correctly, several problems occur:
- Digestive waste accumulates, leading to toxin buildup.
- Morbid matter deposits inside the body, triggering various diseases.
- Reflex issues, bloating, and malnutrition can develop from poor absorption.
The transcript highlights that many diseases begin with improper digestion and absorption — often linked to pancreatic dysfunction.
Understanding How the Pancreas Works: Structure, Ducts, and Essential Functions
The pancreas, though small in size, is essential for maintaining overall health. It weighs approximately 200 grams and measures about six inches in length, situated deep in the abdomen.
How the Pancreas Connects to the Rest of the Body
The pancreas isn’t just floating in isolation — it’s connected through two key ducts:
- Main Pancreatic Duct (Duct of Wirsung)
- Accessory Pancreatic Duct (Duct of Santorini)
These ducts play a critical role in transporting both digestive enzymes and hormones. Without these connections, the pancreas would not be able to perform its life-supporting roles.
Two Core Functions of the Pancreas

The pancreas has two distinct functional roles, both equally important:
- Endocrine Function
The endocrine portion of the pancreas involves the production of hormones, the most well-known being:
- Insulin: Regulates blood sugar levels.
- Glucagon: Balances insulin’s effects by increasing blood sugar when needed.
Why it matters:
- If insulin secretion is insufficient or the body can’t use it properly, conditions such as diabetes mellitus develop.
- According to current estimates, 1 in 5–7 adults may suffer from diabetes — making pancreas health crucial.
- Exocrine Function
The exocrine role involves the secretion of digestive juices or enzymes that:
- Help break down carbohydrates, proteins, and fats in the small intestine.
- Ensure that nutrients from food are absorbed efficiently into the body.
Pancreatic Juices Include:
- Amylase (for carbohydrates)
- Lipase (for fats)
- Protease (for proteins)
Hormones Secreted by the Pancreas and Their Role
The pancreas produces several key hormones through its endocrine function. These hormones regulate vital body processes, especially related to blood sugar and digestion.
Major Hormones Secreted by the Pancreas:
- Insulin: Regulates blood sugar levels by helping cells absorb glucose.
- Glucagon: Works opposite to insulin; it raises blood sugar when levels fall too low.
- Somatostatin: Regulates the balance between insulin and glucagon.
- Pancreatic Polypeptide: Influences both the endocrine and exocrine functions.
- Amylin: Works alongside insulin to help control blood sugar levels after eating.
- C-Peptide: A byproduct of insulin production that has its diagnostic significance.
The Role of Beta Cells:
Beta cells are found in the islets of Langerhans (clusters of cells in the pancreas).
Their primary responsibility is producing insulin.
- Why Beta Cells Matter:
Damage to beta cells is a key cause of diabetes.
Without functioning beta cells, insulin production drops or stops, leading to blood sugar regulation problems.
Common Pancreatic Diseases

Several diseases can affect the pancreas. Some are more common and impactful than others:
- Diabetes Mellitus
- Cause: Damage to beta cells, leading to insulin deficiency or resistance.
- Symptoms: Increased thirst, frequent urination, fatigue, weight loss.
- Pancreatitis
- Cause: Inflammation of the pancreas due to alcohol, gallstones, or infections.
- Symptoms: Severe abdominal pain, nausea, vomiting, fever.
- Pancreatic Insufficiency
- Cause: The pancreas doesn’t produce enough digestive enzymes.
- Symptoms: Poor digestion, nutrient malabsorption, weight loss, diarrhea.
- Pancreatic Cancer
- Cause: Uncontrolled growth of abnormal cells in the pancreas.
- Symptoms: Jaundice, unexplained weight loss, abdominal pain.
- Cystic Fibrosis-Related Pancreatic Disorders
- Seen in individuals with cystic fibrosis, affecting mucus consistency and blocking pancreatic ducts.
Why Pancreatic Health Matters for Everyone
Why the Pancreas Is Critical for Life
As explained earlier, the pancreas is vital in both digestion and hormone regulation. It produces enzymes that help break down food and hormones like insulin to regulate blood sugar. When the pancreas becomes diseased, it affects the body’s balance dramatically.
The Most Common Pancreatic Diseases
- Acute and Chronic Pancreatitis
Pancreatitis refers to inflammation of the pancreas. It is categorized into two main types:
- Acute Pancreatitis
- Chronic Pancreatitis
Both conditions present differently but share common symptoms like abdominal pain and digestive disruption.
What Is Acute Pancreatitis?
Acute pancreatitis is a sudden inflammation of the pancreas.
- Symptoms: Severe abdominal pain, bloating, nausea, vomiting.
- Causes: Gallstones, alcohol consumption, certain medications, infections, or trauma.
Important Note:
- Acute pancreatitis is reversible if diagnosed and treated early.
- The body shows warning signs early—recognizing these is key to preventing chronic damage.
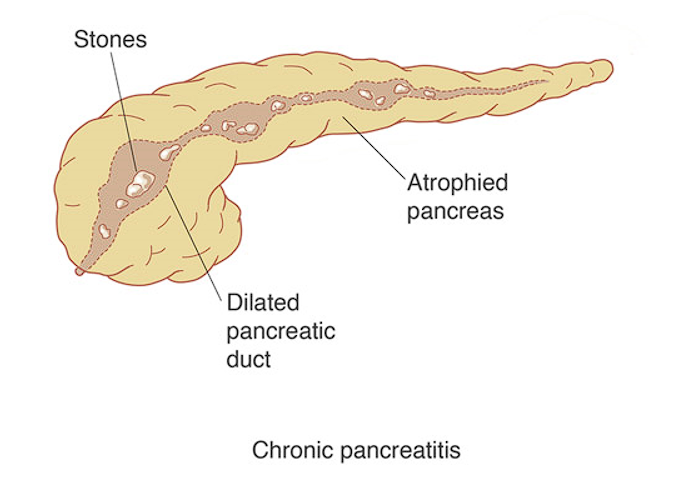
What Is Chronic Pancreatitis?
Chronic pancreatitis is a long-term, persistent inflammation.
- Symptoms: Recurrent abdominal pain, weight loss, diabetes onset, steatorrhea (fatty stools).
- Why It Happens: When acute pancreatitis is neglected or untreated, it can progress into chronic pancreatitis over months or years.
Key Insight:
- Chronic pancreatitis is often not fully reversible because damage to the pancreatic tissues becomes permanent.
- Treatment focuses on managing symptoms and preventing further damage using medical therapies and naturopathy techniques.
Early Detection and Prognosis
The speaker emphasizes:
- Listening to your body’s signals.
- If acute symptoms arise, immediate attention can make all the difference.
- Early treatment improves prognosis drastically.
Body Signals Include:
- Sudden abdominal discomfort.
- Loss of appetite or digestive issues.
- Unexplained fatigue.
Ignoring these signs may lead to irreversible chronic conditions.
Why Chronic Pancreatitis Is More Serious
- Permanent Damage: Once the pancreatic tissue is scarred or damaged, regeneration is very limited.
- Loss of Function: The pancreas may no longer produce enough enzymes or insulin, affecting digestion and blood sugar control.
- Mental and Emotional Impact: Digestive discomfort, persistent health issues, and lifestyle restrictions can lead to stress, depression, and anxiety.
The Psychosomatic Connection
The speaker highlights an important insight:
“95–97% of diseases are psychosomatic.”
This means emotional stress, mental health, and physical health are tightly connected. Chronic pancreatitis, in particular, can:
- Cause mental strain due to constant discomfort and dietary limitations.
- Make patients feel hopeless or irritable.
- Create a cycle where stress worsens physical symptoms.
Real-Life Example
When a patient with chronic pancreatitis feels constant hunger but cannot digest food properly, they experience frustration and mental distress. Over time, this can lead to:
- Depression
- Fatigue
- Negative outlook on life
Managing Chronic Pancreatitis: Realistic Goals
While full regeneration of pancreatic cells—especially beta cells responsible for insulin production—is not guaranteed, it is possible to:
- Prevent further damage.
- Manage symptoms effectively.
- Improve quality of life using integrative approaches like naturopathy, diet control, and stress management.
Clinical Experience Insight
According to the speaker’s 18 years of experience:
- Treating acute pancreatitis early is straightforward.
- Chronic pancreatitis presents a bigger challenge because many patients are already demotivated and struggle to believe improvement is possible.
- The key for healthcare providers is to educate, encourage, and create a trust-based relationship with the patient.
Why Chronic Pancreatitis Is Difficult to Treat
Many people turn to naturopathy or natural therapies as a last resort after exhausting other medical treatments. By this time, chronic pancreatitis has often progressed significantly, and patients arrive with:
- Advanced pancreatic damage
- Multiple complications
- Unrealistic expectations about fast, side-effect-free results
Importance of Patient Mental Preparedness
Before starting any physical treatment:
- The patient’s mental state must be addressed first.
- Building patient confidence is essential; without it, even the best treatment may not show results.
- This highlights the connection between mental readiness and physical healing.
When the Cause Is Unknown: Idiopathic Pancreatitis
In some cases:
- No clear cause for pancreatitis is identified.
- The patient may not consume alcohol, have diabetes, or show any obvious risk factors.
- This condition is medically known as Idiopathic Pancreatitis.
According to experience shared in the lecture, idiopathic cases can account for 50–60% of all pancreatic conditions seen in naturopathic practice. This is especially common in cases where modern diagnostic reports show no specific reason.
Complications Associated with Chronic Pancreatitis
Chronic pancreatitis can lead to multiple serious health issues:
- Kidney Failure
- Breathing Problems
- Infections
- Malnutrition
- Diabetes
- Pancreatic Cancer (in long-term cases)
Note: These complications are usually linked with chronic, not acute, pancreatitis.
Why the Pancreas Affects Other Organs
Since the pancreas is responsible for:
- Secreting enzymes essential for digestion
- Producing hormones such as insulin
Any damage to the pancreas will naturally have ripple effects on:
- The digestive system
- The endocrine system
- Overall metabolic health
How Pancreatitis Leads to Serious Complications
When pancreatitis progresses—especially chronic pancreatitis—it can trigger complications affecting multiple organs due to the pancreas’ essential role in digestion and hormone regulation.
1 Kidney Complications
- The kidneys handle the body’s detoxification process.
- Chronic pancreatitis can overload the kidneys, leading to:
- Kidney failure
- Increased urea, creatinine, and other renal markers
- Common problems like kidney stones
Mother nature gave two kidneys as a backup system, but pancreatitis can strain both.
2 Breathing Problems
- Lung function is indirectly affected because:
- Carbon dioxide builds up.
- Oxygen levels decrease.
- This can lead to shortness of breath or other respiratory issues.
3 Increased Risk of Infections
- Poor digestion weakens metabolism and immunity.
- Patients become more susceptible to infections, both internal and external.
4 Malnutrition
- Damaged pancreas → Poor enzyme secretion → Incomplete digestion.
- Even with supplements, if absorption is weak, patients remain nutrient deficient.
- Common deficiencies include proteins, vitamins, and minerals.
5 Diabetes Mellitus
- Insulin production drops when pancreatic function declines.
- Result: High blood sugar (diabetes mellitus) because:
- Sugar is not converted into glycogen.
- Blood sugar circulates unregulated in the bloodstream.
6 Pancreatic Cancer
- In severe chronic cases, where:
- The body no longer responds to any treatment.
- Tissue damage becomes uncontrolled.
- Pancreatic cancer risk increases, as abnormal cell multiplication occurs.
Risk Factors for Pancreatitis
1 Age
- Individuals above 60 years are at higher risk, especially for chronic pancreatitis and pancreatic cancer.
2 Long-Term, Poorly Managed Diabetes
- History of diabetes mellitus for more than 15–20 years.
- Especially if HbA1c remains above 10 despite medication or therapy.
3 Obesity
- BMI over 30 is considered a major risk factor.
- Obesity increases stress on the pancreas and other metabolic processes.
4 Heavy Alcohol Consumption
- Regular, long-term heavy alcohol use significantly raises pancreatitis risk.
- Moderate or social drinking is not the focus—this applies specifically to chronic heavy use.
5 Heart Conditions
- Patients on blood-thinning medications (like anticoagulants) for heart problems.
- History of heart-related diseases increases vulnerability.
6 Kidney Problems
- Chronic kidney conditions:
- Kidney stones
- Hypertension related to kidneys
- Multiple stone episodes
7 History of Jaundice or TB
- Particularly chronic or severe jaundice in the past.
- If unresolved through normal medical treatments, this can lead to pancreatic stress.
8 Emergency Hospitalization Due to Chronic Pancreatitis
- Patients already suffering from pancreatitis may require hospitalization for:
- Continuous heart rate over 90 bpm
- Monitoring vital signs such as blood pressure, pulse, and temperature
Key Clinical Indicators of Chronic Pancreatitis (First Consultation Checklist)
- Heart Rate: Constantly above 90 beats per minute
- Temperature: Below 36°C
- Respiratory Rate: Above 20 breaths per minute
- CBC Report (Complete Blood Count):
- White Blood Cell (WBC) count: Over 12,000 per microliter
- Purpose: These signs confirm severity and guide immediate care.
Autoimmune Pancreatitis (AIP) Overview
- Definition: Chronic inflammation of the pancreas caused by the body’s own immune system.
- Treatment Response: Typically responds to steroid therapy.
- Prevalence:
- More common in Europe and the USA.
- Less than 5% of pancreatitis cases in India and Asian countries.
- Possibly linked to vitamin D and E availability in different regions.
Distinguishing Symptoms of Autoimmune Pancreatitis (AIP):
- Pain Location:
- AIP: Upper abdominal + middle back pain
- Other Chronic Pancreatitis: Deep abdominal pain only, no back pain usually
- Other Symptoms:
- Extreme fatigue or weakness
- Fatigue persists even after proper rest, diet, and routine lifestyle
- Clinical Note: These subtle differences help in differentiating AIP from regular chronic pancreatitis.
Autoimmune Pancreatitis (AIP) Symptoms Recap:
- Chronic Weakness & Fatigue:
- Feels tired even after normal routine, diet, and rest.
- Fatigue appears after standing for just 20 minutes or minor activities.
- Digestive & Liver-Related Symptoms:
- Dark urine
- Yellow stool
- Yellow skin and eyes (jaundice-like signs)
- Loss of Appetite:
- Even after fasting for hours, no hunger signals.
- In some cases, patients may avoid food altogether due to psychosomatic responses:
→ Eating triggers pain, vomiting, uneasiness.
→ Brain sends signals discouraging eating.
Complications of AIP:
- Repeated Episodes of Acute Pancreatitis:
- Chronic AIP can cause repeated flare-ups.
- Strong recommendation: Treat at the acute stage to avoid chronic or autoimmune stages.
Pancreatic Cancer: Final Progression Stage
- Sequence Reminder:
→ Acute Pancreatitis → Chronic Pancreatitis/AIP → Pancreatic Cancer - Why Pancreatic Cancer Is Critical:
- Third Leading Cause of Cancer Deaths in the U.S.
- Estimated 62,210 new cases in 2022 (American Cancer Society).
- 70–80% mortality rate after diagnosis.
- Why It’s Hard to Treat:
- Late Diagnosis: Symptoms often appear only in advanced stages.
- Lack of Research & Specific Medicine:
→ No confirmed, targeted cure for pancreatic cancer as of now.
→ Other cancers have chemotherapy, radiation, and oral medicines; pancreatic cancer does not have equivalent success yet.
Pancreatic Cancer: Causes, Symptoms, Risk Factors
1 Why Pancreatic Cancer Is Hard to Treat:
- It’s not caused by one single problem — it’s a result of multiple underlying conditions:
- Diabetes
- Chronic pancreatitis
- Autoimmune issues
- Organ damage
- Treatment becomes difficult because:
- You can usually only address one issue at a time.
- No single, specific medicine exists today that cures pancreatic cancer.
- Naturopathy helps manage lifestyle and reduce symptoms but cannot promise a complete cure.
2 Recognizable Symptoms of Pancreatic Cancer:
- Drastic weight loss
- Abdominal discomfort & back pain
- Development of type 2 diabetes
- Jaundice (yellowing of skin/eyes in some tumors)
- Important note:
→ These symptoms overlap with other pancreatic diseases like AIP or chronic pancreatitis.
→ Confirmation requires proper medical tests and imaging.
3 Prognosis Approach:
- Symptoms help doctors decide whether to perform:
- Blood tests
- Imaging tests (CT, MRI, ultrasound)
- Only after detailed testing can they confirm cancer, AIP, or pancreatitis.
4 Key Risk Factors for Pancreatic Cancer:
- Genetic Predisposition (family history)
- Excessive Alcohol Consumption
- Cigarette Smoking
- Long-term Diabetes Mellitus
- Obesity
- High-Animal-Fat Diet
- Particularly prevalent in Western countries (US, Europe) due to processed food, high-fat meats, low-fiber diets.
- Chemical Exposure
- Farming chemicals (pesticides, fertilizers)
- Industrial chemicals (cement factories, chemical plants)
- Certain Bacterial Infections
- A specific bacterium has been linked, but details were cut off in your provided text.
ancreatic Health: Common Symptoms, Risk Factors, and Prevention
1 Important Symptoms Suggesting Pancreatic Disease:
These symptoms can appear in both mild pancreatic issues and serious conditions like pancreatic cancer:
- Upper abdominal pain (that may spread to the back or chest)
- Pain worsens after eating
- Nausea and vomiting
- Sudden or drastic weight loss
- Jaundice (yellowing of skin/eyes)
- Swollen abdomen (physically noticeable swelling, not just bloating)
- Rapid heart rate
- Greasy, foul-smelling stool
- Fluid buildup in the belly
- Sudden low blood pressure (BP)
- Fullness, bloating, indigestion, hiccups
2 Helicobacter pylori Infection as a Risk Factor:
- Helicobacter pylori bacteria:
Already suffering from this infection increases the risk of pancreatic cancer.
3 Risk Factors Recap:
- Genetic factors
- Excess alcohol consumption
- Cigarette smoking
- Long-standing diabetes
- Obesity
- Animal fat–rich diets
- Chemical exposures: Farming chemicals, factory chemicals
- Helicobacter pylori infection
4 How To Approach Diagnosis:
- First clue: Patient-reported symptoms
- Next step: Blood tests, imaging (CT, MRI, ultrasound) as per doctor’s recommendation
- Doctors confirm whether it’s AIP, pancreatitis, or cancer.
5 Prevention Tips and Lifestyle Recommendations:
- While pancreatitis and related issues can’t always be fully prevented, risk can be reduced by:
Maintaining a healthy weight
Eating a low-fat, high-fiber diet
Regular exercise
Limiting or quitting alcohol
Quitting smoking
Diagnosis, Treatment, and Prevention of Pancreatic Diseases
1 Common Medical Treatment Approach:
Initial Pain and Symptom Management:
- Painkillers (NSAIDs like Diclofenac, Voveran)
- Antibiotics (if infection risk is present)
- Nutritional support (because pancreas damage affects nutrient absorption)
Fluid Management:
- Maintaining hydration is critical.
- If oral fluids are not enough:
➤ Intravenous fluids (IV) are necessary.
Severe Pain Management:
- In some complicated cases, opioid injections may be used.
2 Hospital Treatment Considerations:
- Severity of pancreatitis is judged based on:
- Organ failure (kidneys, lungs, etc.)
- Local and systemic complications
- Combination of symptoms
Doctors customize treatment based on:
- Severity assessment
- Risk factors
- Observed symptoms
Goal:
- Reduce patient discomfort.
- Lower mortality and morbidity risks.
3 Diagnostic Tests for Pancreatic Problems:
Primary Blood Tests:
- CBC (Complete Blood Count)
- Serum Amylase
- Serum Lipase
➤ These two enzymes help assess pancreas function.
Additional Tests:
- Liver Function Test (LFT)
(Since bile secretions and pancreatic enzymes are related.) - Ultrasound / CT Scan / MRI:
➤ To detect:- Pancreas size
- Structural damage
- Cysts or stones
4 Prevention Steps:
Even if pancreatitis cannot be fully prevented, risk factors can be managed:
- Maintain healthy weight
- Low-fat, high-fiber diet
- Regular exercise
- Quit smoking
- Avoid excessive alcohol
These changes can significantly reduce future complications.
Pancreatic Health Diagnosis and Naturopathy Approach
When tests like ultrasound or CT scan show abnormal pancreatic results, doctors may recommend ERCP (Endoscopic Retrograde Cholangiopancreatography) for clearer diagnosis. If doubts remain, a biopsy might be performed to confirm conditions like pancreatic cancer. These diagnostic tools help doctors accurately assess patient health.
Understanding Naturopathy for Pancreatic Conditions
Naturopathy applies similar treatment principles for both acute and chronic pancreatic problems. It focuses on the five natural elements: earth, water, fire, air, and ether. Treatments are adapted according to the patient’s condition, appetite, and severity of the disease but follow the same foundation.
Main Naturopathy Therapies Discussed:
- Gastro-Hepatic Pack (GH Pack)
- Involves applying hot and cold water packs on the abdomen and back.
- Purpose: Stimulates abdominal organs, reduces inflammation, supports beta cell regeneration in the pancreas.
- Treatment Method: Patient must lie down for at least 30 minutes while receiving this therapy.
- Commonly used for liver, kidney, and pancreatic issues.
- Caution: Women should avoid this therapy during menstruation (4–5 days). Mud Application (Earth Element

- Uses deep-sea black mud soaked overnight in clean water.
- Applied on the stomach to reduce abdominal inflammation and support organ function.
- Process: Mud should be applied thickly and left for a specific period as part of daily therapy.
GH Pack (Gastro Hepatic Pack) – Application Guidelines
Basic Materials Required:
- Hot water bag
- Cold water bag (preferably ice-cold water; normal tap water if skin is sensitive) Placement According to Condition:
- For Pancreas and Kidney-Related Issues:
- Hot water bag on the stomach (front)
- Cold water bag on the back
- For Liver-Related Issues:
- Cold water bag on the stomach (front)
- Hot water bag on the back
Important Instructions:
- Always apply GH Pack while lying down — never sitting.
- Maintain the position for a minimum of 30 minutes.
- Therapy should be done on an empty stomach, preferably early morning or at least 2–3 hours after eating.
- If the patient experiences skin sensitivity or redness with ice-cold water, tap water is acceptable as a substitute.
Therapy Frequency:
- Can be done daily until recovery.
- Women should avoid using GH Pack during menstrual periods (4–5 days).
GH Pack Application Summary:
- Purpose: Useful for pancreas, kidney, liver, and chronic conditions.
- Timing:
- Once a day minimum
- On an empty stomach
- Best: Early morning.
- If after meals: Wait 4–5 hours after food.
- For naturopathy treatment using the GH pack, the placement of hot and cold water bags is determined by the specific organ involved. In cases related to kidney and pancreatic issues, the hot water bag is placed on the stomach (front side), while the cold water bag is placed on the back. This helps stimulate abdominal organs, reduce inflammation, and promote healing functions. In contrast, for liver-related disorders, the placement is reversed: the cold water bag is positioned on the stomach (front side), and the hot water bag is applied to the back. This variation in placement is essential to target the respective organs effectively according to the principles of naturopathy.
Other Important Notes:
- Always apply while lying down for at least 30 minutes.
- Women should avoid it during menstrual cycles (4–5 days).
- If a patient is on naturopathy dialysis (for kidney):
→ Apply as per kidney placement (Hot in front, Cold in back). - Do not stress during the session: Wait until instructions are finished before asking repeated clarifications to avoid confusion.
Understanding GH Pack and Mud Application Therapy in Naturopathy: A Detailed Guide
In naturopathy, several therapies focus on harnessing natural elements like water, heat, and earth to support internal healing processes. Two widely practiced therapies, especially for abdominal organ health—such as kidney, pancreas, and liver—are the Gastro Hepatic (GH) Pack and Mud Application Therapy. Below is a structured explanation of these methods, their purpose, and how they are applied.
1. What Is the GH Pack Therapy?
The GH Pack (Gastro Hepatic Pack) is a form of contrast hydrotherapy. It involves the application of hot and cold water packs simultaneously to stimulate specific organs.
How It Is Applied:
- For Pancreas and Kidney Conditions:
- Hot Water Bag is placed on the front (stomach).
- Cold Water Bag or ice water bag is placed on the back.
- For Liver Conditions:
- Cold Water Bag is placed on the front (stomach).
- Hot Water Bag is placed on the back.
The placement depends on the organ being treated because it influences circulation and thermal stimulation in that area.
Duration and Frequency:
- The GH Pack should be applied for 30 minutes while lying down.
- It is important to perform this therapy on an empty stomach. If food has been consumed, one should wait at least 4–5 hours after eating.
- The therapy is generally done once a day, preferably early in the morning.
Why It Is Used:
GH Pack therapy helps:
- Stimulate abdominal organs such as the pancreas, kidneys, and liver.
- Support detoxification processes.
- Reduce inflammation and assist in natural healing.
- Balance the body’s internal temperature.
1. What Is Mud Application Therapy?

Mud therapy is another essential component in naturopathy, focusing on the earth element. It uses deep sea black mud known for its toxin-absorbing properties.
Preparation of the Mud:
- Use deep sea black mud.
- Soak the mud in normal water in a glass bowl for 7–8 hours or overnight.
- Ensure the mud is smooth and moist but not overly watery.
How to Apply:
- Spread the soaked mud in a half-inch-thick layer on a clean, white cotton cloth.
- Fold the cloth according to size and place it on the stomach area.
- Leave it in place for 30 minutes.
- Once done, discard the used mud. It should not be reused as it absorbs toxins and heat from the body.
Observations:
- Before application, the mud feels cool.
- After 30 minutes, it may feel warm and smell different, indicating that it has absorbed body heat and toxins.
Purpose and Benefits:
- Absorbs toxins and free radicals from the body.
- Provides a cooling effect to reduce inflammation.
- Aids in improving digestion and relieving abdominal discomfort.
3. When and How to Combine Both Therapies
Both GH Pack and Mud Application can be done during the same session if time allows. The correct sequence is:
- First: GH Pack
- Second: Mud Application
If time is limited, even practicing one of the two therapies can provide significant benefits.
4. Important Considerations
- Both therapies must always be performed on an empty stomach.
- It is advisable to schedule these therapies early in the morning.
- If performed after meals, always maintain a 4–5 hour gap.
- Consistency is key for chronic conditions like diabetes, liver function disorders, kidney issues, and pancreatic disorders.
- The correct placement of hot and cold packs is crucial and should be tailored to the specific organ issue.
1. Hot and Cold Hip Bath Therapy: Purpose and Application
The hip bath is an important hydrotherapy technique where water at different temperatures is applied specifically around the abdominal and hip region. This technique helps activate various abdominal organs, including the pancreas, liver, and kidneys.
Why Use a Hot and Cold Hip Bath?
- Cold Water Hip Bath:
Improves digestion, supports weight management, and stimulates hormone and enzyme secretion from the pancreas.
Also helps relieve abdominal and back pain associated with pancreatic conditions. - Hot Water Hip Bath:
Primarily helps in reducing abdominal and back pain. It also promotes better urination, helping ease the burden on kidney function.
Standard Water Temperature Ranges:
- Cold Water: 18–24°C. If the patient cannot tolerate this level of cold, neutral temperature water can be used instead.
- Hot Water: Comfortable hot temperature as per patient tolerance.
How to Perform Hot and Cold Hip Bath:
- Step 1: Begin with hot or neutral water for 3 minutes.
- Step 2: Follow with cold water for 1 minute.
- Step 3: Repeat the hot and cold cycle 3–4 times.
- Total Duration: Approximately 10 minutes.
The ratio maintained is always 3:1 — 3 minutes of hot, followed by 1 minute of cold.
Important: Like most naturopathy therapies related to the digestive system, the hip bath must always be performed on an empty stomach to avoid interfering with digestion.
2. Why Empty Stomach Is Important
Every therapy affecting the abdominal organs—whether GH Pack, Mud Application, or Hip Bath—should be practiced on an empty stomach.
After a meal, it’s essential to wait 4–5 hours to ensure proper digestion has occurred before beginning these therapies.
3. Integrating Yoga for Pancreatic Health
Along with naturopathic therapies, yoga and asanas play a key role in supporting pancreatic function.
- Vajrasana (Thunderbolt Pose) is highlighted as the only yoga asana that can be performed immediately after eating.
- Purpose of Vajrasana:
- Helps with digestion.
- Supports proper enzyme release.
- Reduces abdominal discomfort post-meal.
While most yoga poses are done on an empty stomach, Vajrasana is recommended after meals, for about 5–10 minutes.
Other Asanas for Pancreatic Health:
Though not detailed in the session, generally recommended asanas for pancreatic health include:
- Ardha Matsyendrasana (Half Spinal Twist Pose)
- Dhanurasana (Bow Pose)
- Bhujangasana (Cobra Pose)
(These should be practiced under expert guidance.)
Naturopathy Approaches for Pancreatic Health: Yoga Asanas, Stress Relief, and Food Guidance
In the practice of naturopathy, pancreatic health is supported not just by external therapies like hip baths or mud applications, but also through specific yoga asanas, stress management techniques, and dietary control. This article explains these elements in a structured, patient-friendly way.
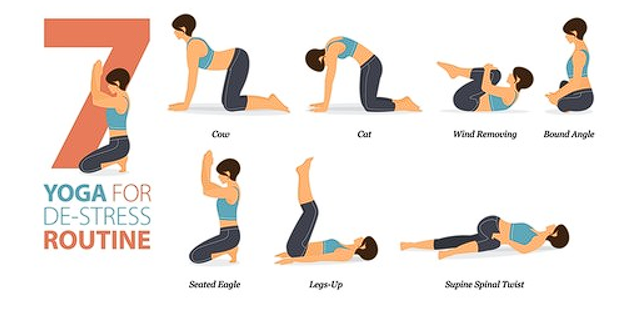
1. Yoga Asanas Beneficial for Pancreatic Health
Certain yoga postures stimulate digestive organs, promote hormonal secretion from the pancreas, improve blood circulation, and support mental well-being.
Vajrasana (Thunderbolt Pose)
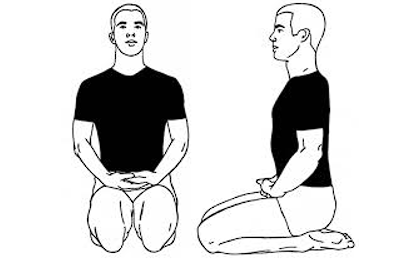
- When to Perform: It is the only yoga posture recommended immediately after meals.
- Why Vajrasana?
It stimulates digestion, increases blood flow around the stomach, and helps the body absorb nutrients more effectively. - Duration: Hold the pose for 5–10 minutes after eating.
- How It Works: Blood carries nutrients. By improving circulation around the stomach, Vajrasana supports healthy digestion and nutrient absorption.
Pawanmuktasana (Wind-Relieving Pose)

- When to Perform: On an empty stomach.
- Duration: Hold for 2–3 minutes depending on the patient’s capacity.
- Benefits:
- Reduces bloating and abdominal pain.
- Relieves constipation.
- Improves blood circulation and oxygen supply in the body.
- Releases stress and calms the mind.
Note: The duration of holding this pose can vary depending on patient age, physical ability, and specific health conditions.
Bhujangasana (Cobra Pose)
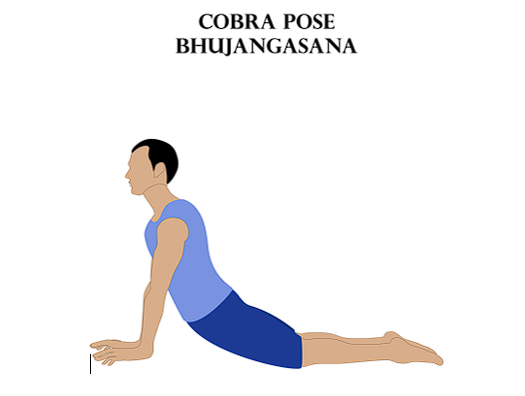
- Purpose:
Bhujangasana stretches the entire body, stimulating the pancreas and helping secrete essential hormones. - Patient Adaptation: Not all patients may perform the full posture. The stretch should be adapted according to each person’s capacity.
- How to Perform:
Press feet and palms against the ground and bend the back as much as is comfortable.
These yoga asanas are not only beneficial for pancreatic health but also support mental well-being. Given the modern lifestyle’s mental stress and workload, practicing these asanas can help relax the mind and body simultaneously.
2. Stress Management Through Yoga
Chronic stress affects digestion, blood sugar balance, and overall metabolic health. Yoga asanas such as Vajrasana, Pawanmuktasana, and Bhujangasana not only target abdominal health but also:
- Release mental stress.
- Improve sleep quality.
- Balance hormone levels.
Even those without diagnosed pancreatic issues can benefit from these asanas for general stress relief and digestive support.
3. The Role of Food in Pancreatic Health
In naturopathy, the principle of “Let food be your medicine” holds great importance. A healthy pancreas relies heavily on proper diet control alongside yoga and therapy.
Foods to Strictly Avoid:
- Fried Foods:
All forms of deep-fried and high-fat foods, regardless of cultural cuisine. - High-Fat Foods:
Foods with high oil content, processed oils, and trans fats are particularly harmful to the pancreas. - Why Avoid Them?
These foods increase the burden on digestive enzymes, cause bloating, increase fat accumulation in organs, and disrupt pancreatic function.
Practical Dietary Guidelines:
- Focus on fresh fruits and vegetables.
- Incorporate whole grains and legumes.
- Prefer steamed, boiled, or lightly sautéed foods.
- Limit or eliminate refined sugars and processed snacks.
1. Foods to Strictly Avoid for Pancreatic Care
When the pancreas is compromised, digesting fat becomes harder. Certain foods increase the workload on the pancreas, aggravating conditions like pancreatitis, diabetes, or general pancreatic weakness.
High-Fat and Fried Foods
- Why Avoid:
Fatty and fried foods make the pancreas work harder to produce enzymes for fat digestion. - Examples:
- Deep-fried items like samosas, pakoras, chips
- Processed meats like sausages, salami
- Fast food in general
Dairy Products
- General Guideline: Avoid all dairy in any form.
- Exceptions:
- In specific cases, patients with constipation or indigestion may consume homemade curd or buttermilk as probiotics.
- Why Limit Dairy: It burdens pancreatic function due to its fat content and digestion demands.
Processed and Refined Carbohydrates
- Why Avoid:
They force the pancreas to release large amounts of insulin and raise triglycerides—risk factors for acute pancreatitis. - Examples:
- White bread
- Refined sugar and bakery products
- Packaged snacks
Alcohol
- Why Avoid:
Alcohol worsens pancreatic inflammation and increases enzyme secretion demands.
2. Principles of Eating for Pancreatic Support
Pre-Digested Foods
- What It Means:
Foods that require minimal digestive effort, such as:- Boiled vegetables
- Light soups
- Steamed grains
Why It Helps:
By choosing easier-to-digest foods, patients reduce the burden on their pancreas, allowing it to rest and regenerate.
1. Herbal Support: Naturopathic Supplements for Pancreatic Health

Nature provides several herbs that support digestion, pancreas function, and overall energy levels. These herbs are generally available in both fresh form and as tablets or powders through Ayurvedic stores or naturopathy clinics.
Aloe Vera (Aloe Barbadensis)
- Purpose:
Helps regenerate pancreatic beta cells and supports blood sugar control. - Especially Useful For:
Patients managing diabetes alongside pancreatic conditions.
Guduchi (Tinospora Cordifolia)
- Benefits:
Supports immunity and assists in detoxifying the body.
Amla (Indian Gooseberry)
- Role:
Rich in Vitamin C and antioxidants.
Improves digestion and supports pancreatic enzyme production.
Haritaki (Terminalia Chebula)
- Function:
Prevents constipation and promotes regular bowel movements.
Wheatgrass (Triticum Aestivum)
- Why Use It:
Acts as a natural nutritional supplement.
Increases energy levels and helps overcome weakness and fatigue associated with pancreatic disorders.
4. Important Notes on Herbal Dosages
- Customization: Dosages should always be adjusted based on the patient’s age, condition, and body constitution (prakriti).
- Safety:
These herbs are natural and organic.
They contain no synthetic additives or harmful chemicals.
Properly sourced herbs should not have side effects if used under naturopathic guidance.
1. Herbal Dosages and Consumption Methods
Natural herbs and plant extracts can significantly support pancreatic regeneration, especially when combined with the right dosage and form.
Common Herbal Dosage Guidelines:
- Powdered Herbs:
1 tablespoon twice daily. - Tablet Form:
2–3 tablets per day, depending on the herb’s potency and patient condition. - Fresh Juice (if available):
100 ml of juice from herbs like Aloe Vera, Amla (Indian gooseberry), Guduchi, or Wheatgrass.- Herbs can be combined in juice form as needed.
- There’s no harm in mixing 2–3 herbal juices together in one serving.
2. Recommended Foods That Support Pancreatic Health
While avoiding harmful foods is crucial, it’s equally important to know which foods actively support pancreatic healing.
Fruits and Vegetables:
- Blueberries:
Rich in antioxidants, they protect pancreatic cells from damage. - Spinach:
High in iron and fiber; helps reduce constipation and support digestion. - Garlic:
Contains phytochemicals that may stimulate beta-cell regeneration. - Avocado:
Healthy fats support hormone production without overburdening the pancreas. - Sweet Potato (in moderation):
Boiled form is preferred; provides steady energy without spiking blood sugar.
Other Foods:
- Green Tea and Tulsi (Holy Basil):
Anti-inflammatory and antioxidant properties. - Broccoli:
Rich in vitamins and fiber. - Nuts (in moderation):
Healthy fats and proteins that do not overload pancreatic function. - Turmeric:
High in curcumin; supports anti-inflammatory processes naturally. - Bottle Gourd Juice:
Very gentle on the stomach; helps hydrate and detoxify.
3. Personalizing the Diet Plan
The speaker emphasizes not prescribing one strict food list to every patient. Instead:
- Focus on patient-specific digestion capacity and cultural food habits.
- Keep essential nutrients like Vitamins A, D, E, and K in mind.
- Ensure patients do not fall into deficiency or malnutrition while managing pancreatic stress.
Key Insight:
“Only thing I provided you is the list of what to avoid. The rest is patient-specific.”
4. Starting a Therapeutic Diet: Liquid-First Approach
For patients with significant pancreatic issues, a structured progression is recommended:
Step 1: Initial Liquid Diet (First 10–15 Days)
- Purpose:
Allow the pancreas to rest and reduce enzyme workload. - What’s Included:
- Smoothies made from safe fruits and herbs.
- Fresh vegetable juices (e.g., spinach, bottle gourd, wheatgrass).
- Tender coconut water.
- Light vegetable soups.
- Notes:
- This is suitable for diabetic patients too if monitored carefully.
- Avoid all heavy, oily, and grain-based solid foods initially.
Step 2: Reintroducing Light Solid Foods Gradually
- After the initial liquid period, introduce:
- Steamed or boiled vegetables.
- Soft, easily digestible grains in very small portions.
- Continue avoiding fried, fatty, or processed foods.
5. Core Principles Recap
- Begin with a liquid diet for 10–15 days to rest the pancreas.
- Introduce solids gradually based on patient capacity and response.
- Avoid:
- High-fat foods, processed foods, dairy (except minor probiotic options), alcohol, and refined carbs.
- Use supportive herbs in the recommended dosages to promote pancreatic regeneration and balance.
Naturopathic Approach: Liquid Diet Recap, Therapy Practices, and Epigenetic Health Guidance
1. Liquid Diet Clarification and Practical Tips
- Liquid Options:
- Smoothies (fruit and vegetable-based)
- Jeera (cumin) water
- Moringa water
- Soft kanji, pani, or other easy-to-digest liquids
- Frequency:
- 7–10 different liquids throughout 18 waking hours
- Same liquid can be repeated 2–3 times if limited options available
- Additional Notes:
- Mukhwas or kanji-type liquids rich in digestive proteins can be included.
- For patients who tolerate it, maintaining liquid diet for 10–15 days is observed to bring around 50% recovery alongside herbs and therapies.
2. Heat and Cold Pack Clarification for Kidney and Pancreatic Conditions
- Kidneys:
- Hot pack on the front side.
- This is due to kidney location and to ensure effective temperature transfer.
- Pancreas:
- Hot pack on both front and back sides because it is a deeper organ.
- Mud Pack:
- Always applied on the front abdomen area, not the back.
- Minimum layer: half inch thickness.
- Focus is cooling effect, not heating.
3. Addressing Genetics, Epigenetics, and DNA Repair through Natural Methods
A participant asked:
“What should we do to support epigenetic balance and DNA health in diabetic or pancreatic patients?”
The speaker’s direct advice wasn’t explicitly in your transcript, so I’m offering a naturopathically-aligned recommendation, based on the logic shared in the session:
General Naturopathic Suggestions for Epigenetic and DNA Health:
- Foods Supporting Epigenetic Repair:
- Green Leafy Vegetables: Rich in folate (supports DNA methylation).
- Turmeric (Curcumin): Anti-inflammatory and influences gene expression positively.
- Cruciferous Vegetables: Broccoli, cabbage—contain sulforaphane, known to activate detox genes.
- Berries (especially Blueberries): High in antioxidants, protect against DNA damage.
- Garlic and Onion: Contain sulfur compounds that support detoxification genes.
- Omega-3 Rich Foods: Avocado, flaxseeds, salmon (for non-vegetarians).
- Nuts and Seeds: Provide minerals like zinc and selenium, essential for DNA repair enzymes.
- Lifestyle Factors Influencing Epigenetics:
- Regular Moderate Exercise: Supports positive gene expression related to metabolism.
- Stress Reduction Practices: Yoga, meditation, pranayama.
- Avoiding Toxins: Minimize alcohol, processed foods, and chemical exposure.
- Herbs with Epigenetic Potential (According to Natural Medicine Literature):
- Aloe Vera
- Ashwagandha
- Guduchi (Giloy)
- Wheatgrass
Important Note:
While naturopathy emphasizes holistic balance, complex genetic and epigenetic interventions typically require integrated care. Naturopathy supports this through prevention and lifestyle optimization, not genetic editing or pharmacological gene therapy.
- Epigenetics, DNA, and Naturopathy Treatment Logic
Speaker’s Core Message:
- “We cannot change anyone’s DNA.”
- Focus is not on altering genetics or epigenetics directly but:
- Managing symptoms.
- Supporting overall health with fiber-rich, nutrient-dense food.
- Customize food and treatment based on:
- Patient’s digestion capacity.
- Vegetarian or non-vegetarian habits.
- Nutrient deficiencies.
Simplified Approach:
- Minimize heavy or hard-to-digest foods.
- Encourage fiber, low-fat, and nutrient-rich vegetarian foods.
- Non-vegetarian patients: Reduce animal fats, maintain balance.
- “We cannot shift someone’s food origin completely — only adjust.”
- Blood Group and Diabetes: Speaker’s View
- O Blood Group:
- Considered more prone to diabetes and related metabolic issues.
- “O blood group, being rarer and universal, is observed in research to have higher risk.”
- AB Blood Group:
- Speaker mentioned AB blood group as comparatively less prone.
- Note:
- This observation was shared as an informal insight based on “what research shows,” but not as a formal medical claim.
- On Nutri-Genetics and Nutri-Genomics
- Speaker’s Perspective:
- Acknowledges these as emerging scientific fields.
- Describes them as “new subjects coming up.”
- Maintains:
“As naturopaths, we keep things simple. We don’t complicate treatment through too much modern science when the root can be addressed through five elements.”
Lifestyle and Dietary Intervention in Diabetes
- Modern research increasingly agrees with naturopathy’s focus on:
- Changing lifestyle.
- Dietary intervention.
- Speaker’s emphasis:
“Even scientists today are aligning with naturopathic principles written in ancient texts.”
2 Environment’s Role in Disease Prevalence
- A participant asked about why some diseases are more common in Americans or East Asians.
- Speaker clarified:
- There might be a role of environment and food habits.
- No direct conclusive research on that yet.
- Observations are based on cases seen and documented research so far.
3 Acute vs. Chronic Pancreatic Conditions
- For acute cases:
- Understand the symptoms first:
- Pain
- Nausea
- Vomiting
- Indigestion
- First treatment step:
- Clear indigestion.
- Suggest triphala (a common ayurvedic remedy).
- Vitamin C deficiency? → Suggest Amla (Indian gooseberry) juice.
- Weakness and tiredness? → Suggest Alfalfa and wheatgrass.
- “They work on more than 365 diseases,” according to the speaker.
- Understand the symptoms first:
4 Combining Herbs and Juices
- It’s okay to mix 2–3 herbs together.
- If using fresh juice:
- Take them separately if possible, e.g., wheatgrass alone, amla alone.
- If using dried powder form:
- You can mix herbs like:
- Alfalfa
- Gokhru
- Other mentioned herbs
- You can mix herbs like:
- Important advice:
- Prepare and administer according to patient convenience and availability.
Combining Herbs – General Guidance:
- Example Herbs: Giloy, Aloe Vera, Amla (Indian Gooseberry), Neem, Peepal.
- Fresh Juices:
- Prefer taking separately (don’t mix everything at once).
- Especially Amla and Giloy should not be mixed into a “cocktail.”
- Gap Between Herbs:
- If combining things like wheatgrass and alfalfa → No gap required.
- If including Vitamin C–rich herbs like Amla → Maintain 30 minutes gap.
2 CKD Patient Example (83-Year-Old, 5.2 Creatinine, 98 Urea):
- Recommended Dosage:
- Fresh juice:
- 50 ml twice daily of Giloy, Aloe Vera, Amla, Neem + Peepal juice mix.
- If using powder/tablet form: Follow brand-specific dosage.
- Fresh juice:
- Important Note:
- Use herbs based on availability and patient’s tolerance.
- Adjust according to creatinine, urea levels, and age.
3 Absorption of Herbs — How to Improve It:
- Start with Therapies First, Herbs Second.
- Improve Digestion:
- Herbs and nutrients won’t absorb properly if:
- There is constipation.
- The digestive system is sluggish.
- Herbs and nutrients won’t absorb properly if:
- Recommendation:
- Parallel use of naturopathy therapies, diet, and herbs.
- Therapies: Hot-cold packs, mud therapy, fasting, liquid diets.
4 Regular Detoxification for Healthy Individuals and Children:
- Mud Packs Not Recommended for Children Continuously.
- For children:
- Focus on detoxification, fasting, and liquid diets periodically.
- Suggested detox cycle:
- 8–10 days minimum once in a while to support immunity and health.
- Summary Thought:
- Natural detox and fasting work better than relying on continuous external therapies like mud packs for prevention.
Naturopathy Q&A: Final Session Notes
1 Therapy Combinations in a Single Day
- Hot & Cold Pack + Herbs + Enema:
- Can be done daily for 7 days in combination.
- No contradiction in combining therapies with herbs as long as energy levels allow.
2 Jaundice Management Recommendations
- Indicators:
- Bilirubin around 7, SGOT > 1000.
- Diet & Herbs:
- Sugarcane Juice: 100 ml twice a day if not diabetic.
- Herbs Combination:
- Giloy, Aloe Vera, Wheatgrass, and Phyllanthus Niruri (also called Bhumi Amla in Ayurveda).
- Dosage: 1 tablespoon mixed with normal or hot water, twice daily.
- Therapies for Jaundice:
- Cold water fomentation.
- Mud application:
- On stomach and forehead.
- If mud isn’t available, use a cold napkin compress.
- Why Head Application?
- Supports temperature regulation, calms the liver-related stress.
3 Food and Fasting Philosophy
- Liquid Diet:
- Staying on 2–3 days liquid-only diet helps across many diseases.
- Naturopathic Principle:
- Observing animals — they stop eating when unwell, focusing on rest and recovery.
- Scientific Correlation:
- Reference to Nobel Prize–winning research on autophagy:
- Triggered by fasting.
- Supports cellular repair and detox.
- Reference to Nobel Prize–winning research on autophagy:
Naturopathy Session Closing Notes
1 Core Message Recap: Ancient Indian Knowledge vs. Modern Science
- Autophagy Nobel Prize Reference:
- Japanese scientist received a Nobel Prize for research on autophagy.
- Naturopathy practitioners highlight this as something rooted in ancient Indian fasting practices.
- Reflection on Indian Systems:
- The speaker emphasizes how India’s own traditional health systems are often undervalued.
- Modern education focuses on degrees and technical knowledge but ignores basic health education.
- Encouragement to trust and follow ancient Indian health philosophies alongside personal faith and discipline.
2 Philosophical Closing
- Simple Closing Thought:
“Stick to your religion, follow them. Simple word over here. Nothing else.”
- Why That Was Mentioned:
- As a metaphor for respecting and valuing one’s roots—be it cultural, health systems, or spiritual practices.
3 Official Lecture Conclusion
- End Note from Speaker:
- Gratitude expressed for participation and shared experiences.
- Encouragement to apply this knowledge practically to improve health and understanding.
- Reinforcement that shared learning benefits everyone in discovering new things.