PCOD AND PCOS BY DR AKANSHA SINGH
Understanding the Reproductive System and Managing Disorders through Naturopathy and Yoga
The reproductive system plays a crucial role in the continuation of the human species. In simple terms, it is the system responsible for reproduction, ensuring the survival and continuation of life. In this article, we will explore the physiology of the reproductive system, its functions, and how disorders such as Polycystic Ovary Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) can be managed through naturopathy and yoga.
The Reproductive System: An Overview
The reproductive system is integral to human reproduction. It includes various organs and glands that work together to facilitate the production of offspring. The main function of the reproductive system is to produce gametes, the reproductive cells that unite to create a new organism.
At the heart of the reproductive system are the gonads, which are the primary endocrine glands responsible for producing these gametes. In males, the gonads are the testes, which produce sperm, while in females, the gonads are the ovaries, which produce eggs (ova).
These gonads also play a crucial role in the secretion of hormones, which are responsible for the development of reproductive organs and the proper functioning of the entire reproductive process.
The Role of Hormones in Reproduction
Hormones produced by the gonads are essential in regulating various aspects of reproduction. In males, the primary hormone is testosterone, which is responsible for the development of male sexual characteristics such as facial hair, deepening of the voice, and muscle development. In females, the main reproductive hormones are estrogen and progesterone. These hormones regulate the menstrual cycle, facilitate the maturation of eggs, and prepare the body for pregnancy.
These hormones also help with the development of secondary sexual characteristics in both genders, such as body hair, breast development, and changes in voice pitch during puberty. The precise balance of these hormones is essential for maintaining reproductive health and ensuring proper functioning of the reproductive organs.
Common Reproductive Disorders: PCOD and PCOS
Two common reproductive disorders that affect many individuals are Polycystic Ovary Disease (PCOD) and Polycystic Ovary Syndrome (PCOS). Both of these conditions primarily affect women and can impact fertility and overall reproductive health.
Polycystic Ovary Disease (PCOD)
PCOD is a hormonal disorder in which a woman’s ovaries become enlarged and develop multiple small cysts. This condition is associated with irregular periods, excessive androgen (male hormone) levels, and infertility. Women with PCOD may experience symptoms such as weight gain, acne, excessive hair growth, and difficulty in conceiving.
Polycystic Ovary Syndrome (PCOS)
PCOS is a more common condition that shares many similarities with PCOD. In PCOS, women may have irregular or absent menstrual cycles, cysts in the ovaries, and elevated levels of male hormones. Like PCOD, PCOS can cause symptoms such as acne, excessive hair growth, and difficulty conceiving. However, the condition is more widely recognized and diagnosed, and its management is typically more standardized.
Both of these conditions can disrupt the normal functioning of the reproductive system, leading to challenges in conception and various health issues.
Managing Reproductive Disorders through Naturopathy and Yoga
While conventional treatments for reproductive disorders often involve medications or hormonal therapies, naturopathy and yoga offer alternative, holistic approaches to managing these conditions and promoting overall reproductive health.
Naturopathy: A Natural Approach to Hormonal Balance
Naturopathy focuses on the use of natural treatments to support the body’s healing processes. In the case of reproductive disorders such as PCOD and PCOS, naturopathic treatments may include:
- Dietary Changes: A balanced, nutrient-dense diet can help regulate hormone levels, reduce inflammation, and improve overall reproductive health. Foods rich in antioxidants, healthy fats, and vitamins (such as vitamin D and omega-3 fatty acids) may support hormonal balance.
- Herbal Remedies: Certain herbs, such as Vertex (Chaste Tree Berry), Spearmint, and Saw Palmetto, are believed to help balance hormones, regulate menstrual cycles, and reduce symptoms of PCOS. Herbal supplements should always be taken under the guidance of a qualified healthcare professional.
- Supplements: Supplements such as magnesium, zinc, and omega-3 fatty acids can help improve insulin sensitivity, support hormone production, and reduce inflammation in the body.
Yoga: Restoring Balance through Movement and Mindfulness
Yoga has been practiced for centuries as a way to promote overall well-being. For women with reproductive disorders, certain yoga practices can help reduce stress, balance hormones, and improve circulation to the reproductive organs. Some key benefits of yoga in managing reproductive health include:
- Stress Reduction: Chronic stress can exacerbate hormonal imbalances and contribute to conditions like PCOS. Yoga’s focus on mindfulness and relaxation techniques can help reduce cortisol levels (the stress hormone), promoting a healthier hormonal environment.
- Improved Circulation: Specific yoga poses, such as Viparita Karani (Legs-Up-the-Wall Pose) and Sputa Buddha Kona Sana (Reclining Bound Angle Pose), can improve blood flow to the ovaries and uterus, supporting the overall health of the reproductive organs.
- Hormonal Balance: Certain yoga poses, including Uttanasana (Standing Forward Bend) and Setu Bandhasana (Bridge Pose), are believed to stimulate the thyroid and adrenal glands, which play a significant role in hormone production. These poses may help balance reproductive hormones and regulate the menstrual cycle.
- Emotional Well-being: Yoga encourages emotional balance through mindfulness and meditation, which can help individuals cope with the emotional challenges that come with reproductive health issues.
The Role of Gonads and Hormones in Reproductive Health 
The reproductive system is a complex network of organs and hormones working together to enable reproduction. At the center of this system are the gonads, the endocrine glands responsible for producing gametes (reproductive cells) and hormones. In males, these gonads are the testes, while in females, they are the ovaries. Understanding how these gonads work and how their function is regulated by hormones is crucial for understanding reproductive health, particularly when discussing conditions such as hormonal imbalances or disorders.
The Role of Gonads and Hormones
The gonads (testes in males and ovaries in females) produce gametes—sperm in males and eggs (ova) in females. However, the function of these gonads is heavily regulated by hormones. One of the key hormones responsible for regulating the release of other hormones is gonadotropin-releasing hormone (GnRH), which is produced by the hypothalamus in the brain. GnRH signals the pituitary gland to release gonadotropins, including luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones then stimulate the gonads (testes or ovaries) to produce sex hormones and gametes.
In both males and females, the secretion of gonadal hormones is tightly controlled to maintain a delicate balance necessary for reproductive health. These gonadal hormones are responsible for the development and functioning of the reproductive organs and the regulation of sexual characteristics and cycles.
The Male Reproductive System: Testes and Testosterone
In males, the primary gonads are the testes—a pair of organs responsible for producing sperm and the hormone testosterone. Testosterone is the primary male sex hormone and plays a crucial role in the development of male reproductive tissues, including the prostate and testes. It is also responsible for the development of secondary sexual characteristics such as facial hair, deeper voice, and increased muscle mass.
Testosterone is essential not only for sperm production but also for maintaining libido, bone density, and muscle strength. A proper balance of testosterone is critical to male health, and any disruptions in its production can lead to various reproductive and health-related issues, including erectile dysfunction, low libido, and infertility.
The Female Reproductive System: Ovaries and Hormonal Regulation
In females, the gonads are the ovaries, which are responsible for producing eggs and the hormones estrogen and progesterone. These hormones play a central role in the menstrual cycle, pregnancy, and the development of secondary sexual characteristics such as breast development and wider hips.
- Estrogen: This hormone is involved in regulating the menstrual cycle, promoting the development of female secondary sexual characteristics, and supporting the health of bones and the cardiovascular system.
- Progesterone: This hormone is primarily involved in preparing the uterus for pregnancy. It ensures that the uterine lining is ready for the implantation of a fertilized egg. If pregnancy does not occur, progesterone levels fall, leading to menstruation.
The proper function of the ovaries and the balance of estrogen and progesterone are vital for regular menstrual cycles and fertility. Any disruptions to this hormonal balance can result in conditions such as Polycystic Ovary Syndrome (PCOS), irregular periods, and infertility.
: The Interplay between Gonads and the Pituitary Gland
The function of both the testes in males and the ovaries in females is regulated by a complex interaction between hormones produced by the brain and pituitary gland. The gonadotropin-releasing hormone (GnRH) released by the hypothalamus triggers the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland. These hormones, in turn, stimulate the gonads to produce their respective sex hormones (testosterone in males and estrogen and progesterone in females).
This regulatory feedback loop is crucial for maintaining the proper hormonal balance in the body. Any disruptions in the production or regulation of these hormones can lead to a variety of reproductive health issues, including hormonal imbalances, infertility, and irregular menstrual cycles.
Key Hormones in Male and Female Reproductive Health
- Testosterone (Male): The primary male sex hormone, responsible for sperm production, the development of male secondary sexual characteristics, and maintaining overall male reproductive health.
- Estrogen (Female): The primary female sex hormone, responsible for regulating the menstrual cycle, the development of female secondary sexual characteristics, and supporting bone health.
- Progesterone (Female): A key hormone in preparing the uterus for pregnancy and maintaining the early stages of pregnancy.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): These hormones, produced by the pituitary gland, regulate the production of testosterone in males and estrogen and progesterone in females.
Understanding the Primary and Accessory Sex Organs in Male and Female Reproductive Systems
The reproductive system is a complex and finely-tuned network of organs and hormones that work together to ensure the continuation of the species. Within this system, there are primary and accessory sex organs, each playing a specific role in reproduction. Understanding the structure and function of these organs, as well as the hormones they produce, is essential for comprehending human reproductive health.
Primary and Accessory Sex Organs in Males
In males, the primary sex organs are the testes, which are responsible for producing sperm (the male gamete) and the hormone testosterone. Testosterone plays a key role in the development of male sexual characteristics such as facial hair, deepened voice, and muscle growth, as well as the production of sperm.
However, the male reproductive system also includes accessory sex organs, which are not involved in sperm production but support the function of the reproductive system. These accessory organs include:
- Prostate Gland: The prostate gland produces fluid that nourishes and protects sperm during ejaculation.
- Urethra: The urethra is a tube that carries urine from the bladder and semen from the reproductive system to the outside of the body.
- Penis: The penis serves as the organ for sexual intercourse and also acts as a conduit for the passage of semen and urine.
Together, the testes, prostate gland, urethra, and penis make up the male reproductive system. The proper functioning of these organs is essential for reproduction and overall male health.
Primary and Accessory Sex Organs in Females
In females, the primary sex organs are the ovaries, which are responsible for producing eggs (ova) and the hormones estrogen and progesterone. Estrogen and progesterone play crucial roles in regulating the menstrual cycle, supporting pregnancy, and facilitating the development of secondary sexual characteristics such as breast development and wider hips.
In addition to the ovaries, the female reproductive system includes several accessory sex organs that play an important role in the reproductive process. These include:
- Genital Ducts:
- Fallopian Tubes: These tubes transport eggs from the ovaries to the uterus and are the site where fertilization often occurs.
- Uterus: The uterus is where a fertilized egg implants and grows during pregnancy. It is also responsible for shedding the uterine lining during menstruation.
- Cervix: The cervix is the lower part of the uterus that connects to the vagina. It plays a role in the passage of sperm into the uterus and also helps prevent infections.
- Vagina: The vagina serves as the passageway for menstrual blood, the site of sexual intercourse, and the birth canal during delivery.
- External Genitalia:
- Labia Majora and Labia Minora: These are the folds of skin that protect the internal female reproductive organs.
- Clitoris: A highly sensitive organ involved in female sexual pleasure.
These organs are integral to the female reproductive system, with each playing a role in menstruation, conception, pregnancy, and childbirth.
The Importance of Hormonal Regulation
As mentioned earlier, the functioning of both male and female reproductive systems is regulated by hormones. In males, the testes produce testosterone, while in females, the ovaries secrete estrogen and progesterone. These hormones work in tandem to regulate the development and functioning of the reproductive organs.
For example, in females, estrogen stimulates the growth and development of the reproductive organs and the secondary sexual characteristics, while progesterone prepares the uterus for pregnancy by thickening the uterine lining. The proper balance of these hormones is essential for maintaining a regular menstrual cycle, fertility, and overall reproductive health.
In both sexes, the secretion of these hormones is regulated by the pituitary gland, which releases gonadotropins such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones stimulate the gonads (testes or ovaries) to produce the respective sex hormones. The feedback loop between the gonads and the pituitary gland ensures a balanced hormonal environment, critical for healthy reproductive function. Understanding the structure and function of these organs, as well as the hormonal regulation involved, is vital for addressing reproductive health issues and promoting overall well-being.
Anatomy of the Female Reproductive System: Primary and Accessory Sex Organs
The female reproductive system consists of both primary and accessory sex organs, each playing a crucial role in reproduction and overall female health.
Primary Sex Organs
The primary sex organs in females are the ovaries, which are responsible for producing eggs (ova) and hormones essential for sexual function and reproduction. The ovaries are the primary source of estrogen and progesterone, hormones that regulate the menstrual cycle, fertility, and secondary sexual characteristics.
Accessory Sex Organs
In addition to the ovaries, the female reproductive system includes accessory sex organs that aid in the process of reproduction. These organs include:
- Genital Ducts: These structures help transport the egg from the ovaries to the uterus. The fallopian tubes, which extend from the uterus toward the ovaries, are the primary ducts where fertilization occurs.
- Uterus: Also known as the womb, the uterus is a central organ in the female reproductive system. It is a hollow, muscular structure located in the pelvic cavity, situated between the rectum and urinary bladder. The uterus plays a key role in supporting a developing fetus during pregnancy.
- Cervix: The cervix is the lower part of the uterus that connects it to the vagina. It has a central cavity that opens into the vagina, facilitating the passage of menstrual blood, sperm, and, eventually, the baby during childbirth.
- Vagina: The vagina is a muscular canal that serves as the entry point for sperm and the passageway for menstrual blood and childbirth. It connects the uterus to the external genitalia.
Functional Anatomy of the Uterus 
The uterus is one of the most vital organs in the female body. It is responsible for housing and nourishing a fertilized egg during pregnancy. Structurally, the uterus is composed of several layers:
- Endometrium: The innermost layer of the uterus, the endometrium, is where a fertilized egg implants and develops during pregnancy. If pregnancy does not occur, this layer sheds during menstruation.
- Myometrium: The middle layer of the uterus, the myometrium, consists of smooth muscle tissue that contracts during labor to expel the baby.
The uterus is designed to expand and contract as needed, ensuring that it can house a developing fetus and facilitate the process of childbirth.
The Cervix and Vagina: Connecting Structures
The cervix serves as the passage between the uterus and the vagina. It produces mucus that changes in consistency during the menstrual cycle to either block or facilitate the passage of sperm. The cervix also plays a significant role during childbirth, as it dilates to allow the baby to pass from the uterus into the birth canal.
The vagina is the muscular canal that leads from the cervix to the external genitalia. It serves as the receptacle for sperm during intercourse and as the birth canal during delivery. The vaginal environment also plays a role in protecting against infections through its acidic pH.
External Genitalia and Additional Structures
The external female genitalia include the labia majora, labia minora, clitoris, and the vulva, which serve to protect the internal reproductive organs. However, these external features, while important for sexual function, are not classified as reproductive organs.
It is important to distinguish between the anatomical structures involved in reproduction and those that serve other functions. While features such as the labia, clitoris, and vulva are critical for sexual arousal and protection of the reproductive organs, they do not play direct roles in reproduction.
Anatomy of the Vagina and Ovaries: Functions, Disorders, and Treatment Approaches
The Vagina: Structure and Function
The vagina is a short, tubular organ that plays a significant role in the female reproductive system. It is lined with a mucous membrane made up of stratified epithelial cells, which provide protection and moisture. The vagina serves several key functions, including acting as the passageway for menstrual flow, receiving sperm during sexual intercourse, and serving as the birth canal during labor and delivery.
The Ovaries: Primary Sex Organs in Females
The ovaries are considered the primary sex organs in females. Females typically have two ovaries, which are located on either side of the uterus. The ovaries perform two main functions:
- Gonadal Function (Genetic Function): The ovaries are responsible for producing and releasing ova (eggs), which are the female reproductive cells or gametes. Each egg contains half of the genetic material necessary for the formation of a new individual upon fertilization by sperm.
- Endocrine Function: The ovaries also secrete hormones, primarily estrogen and progesterone, which regulate the menstrual cycle, control reproductive processes, and influence secondary sexual characteristics such as breast development and the distribution of body fat.
These two vital functions make the ovaries critical to female reproduction, classifying them as the primary sex organs.
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS)
An important condition affecting the ovaries is Polycystic Ovarian Disease (PCOD), which often leads to confusion with Polycystic Ovary Syndrome (PCOS). While these terms are sometimes used interchangeably, there are distinct differences between them.
Polycystic Ovarian Disease (PCOD)
PCOD is a condition in which the ovaries do not release a mature egg during each menstrual cycle. Instead, the egg becomes trapped in the follicle, preventing it from fully maturing. As a result, the follicle fills with fluid and forms a cyst. Over time, multiple cysts can develop within the ovaries. This condition may be visible on an ultrasound and can cause irregularities in the menstrual cycle, difficulty with ovulation, and potential fertility challenges.
Polycystic Ovary Syndrome (PCOS)
PCOS is a more complex hormonal disorder that can include the presence of multiple cysts in the ovaries, but it also affects the body in other ways. It may cause hormonal imbalances leading to symptoms such as irregular periods, excessive hair growth, acne, and obesity. Unlike PCOD, PCOS may also be associated with insulin resistance and other metabolic issues.
Naturopathy Treatment Approaches for PCOD
In the field of naturopathy, there are various holistic approaches for managing PCOD. These treatments focus on balancing hormones, improving the function of the ovaries, and promoting overall health. Some commonly recommended strategies include:
- Dietary Changes: A balanced diet that includes anti-inflammatory foods, low-glycemic-index foods, and essential nutrients can help regulate insulin levels and promote ovarian health.
- Herbal Remedies: Certain herbs like Vitex (Chaste Tree) and Spearmint may help balance hormonal levels, especially in women with PCOD who experience excess male hormones (androgens).
- Lifestyle Modifications: Regular exercise, stress management, and weight control are essential in managing PCOD. Reducing stress through practices such as yoga or meditation may also have positive effects on hormone balance.
By focusing on lifestyle and dietary changes, naturopathy aims to treat PCOD in a non-invasive, natural way, improving symptoms and fertility outcomes.
Polycystic Ovarian Disease (PCOD) vs. Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Differences
Understanding PCOD and PCOS
Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) are both conditions that affect the ovaries and cause hormonal imbalances in women. Though often used interchangeably, they are distinct in their nature and severity. PCOD tends to be less severe than PCOS, though both conditions share similar underlying causes and symptoms.
Polycystic Ovarian Disease (PCOD) 
PCOD is primarily characterized by the formation of cysts in the ovaries due to immature or partially mature eggs not being properly released during the menstrual cycle. Instead of the egg fully maturing, the follicle fills with fluid and forms a cyst. This disruption in the egg maturation process leads to hormonal imbalances and various symptoms, most notably affecting the menstrual cycle.
Key Symptoms of PCOD:
- Irregular Menstrual Cycles: The most common symptom, as the hormonal imbalance disrupts the regular cycle of ovulation and menstruation.
- Weight Gain: Many women with PCOD experience difficulty managing weight due to hormonal fluctuations, particularly involving insulin resistance.
- Acne and Oily Skin: Hormonal imbalances often lead to an overproduction of oil in the skin, which can cause acne.
- Hair Thinning or Hair Loss: Some women with PCOD notice thinning hair, which may be related to hormonal changes.
- Fatigue and Lethargy: Women with PCOD often experience unexplained tiredness and low energy levels, making it difficult to perform daily tasks.
The hormonal imbalances in PCOD can also contribute to insulin resistance, leading to increased blood sugar levels and a greater likelihood of developing conditions like diabetes.
Main Causes of PCOD: Although the exact cause of PCOD remains unclear, several factors are believed to contribute to its development, including:
- Hormonal Imbalances: An imbalance in the production of reproductive hormones, particularly androgens (male hormones), can interfere with normal ovulation.
- Insulin Resistance: Many women with PCOD have a reduced ability to use insulin effectively, leading to higher levels of insulin in the body. This, in turn, can increase the production of androgens, exacerbating symptoms.
- Genetic Predisposition: A family history of PCOD or similar conditions may increase the likelihood of developing PCOD.
- Lifestyle Factors and Stress: Poor diet, lack of exercise, and high-stress levels can aggravate hormonal imbalances and insulin resistance.
PCOS, or Polycystic Ovary Syndrome, is a more complex condition that includes not only hormonal imbalances but also metabolic issues. It is a syndrome, meaning it consists of a group of symptoms affecting multiple systems in the body.
PCOS often involves the presence of multiple cysts on the ovaries, irregular or absent ovulation, and metabolic disturbances. Women with PCOS may experience more severe symptoms compared to those with PCOD due to the metabolic aspect of the disorder.
Key Characteristics of PCOS:
- Hormonal Imbalances: Women with PCOS typically have elevated levels of androgens, or male hormones, which can lead to symptoms like excess hair growth (hirsutism), acne, and thinning scalp hair.
- Irregular or Absent Menstrual Cycles: Similar to PCOD, women with PCOS often experience missed periods or irregular cycles, making conception more difficult.
- Ovarian Cysts: Multiple cysts may develop in the ovaries due to the incomplete maturation of eggs.
- Metabolic Issues: Women with PCOS are more likely to experience insulin resistance, which can lead to higher blood sugar levels, obesity, and an increased risk of type 2 diabetes. This is one of the key differences between PCOS and PCOD.
- Increased Risk of Heart Disease: Due to the metabolic disruptions and hormonal imbalances, women with PCOS are at a higher risk for cardiovascular diseases.
The Difference between PCOD and PCOS
While both PCOD and PCOS involve hormonal imbalances and ovarian cysts, there are key differences:
- Severity: PCOS is generally more severe than PCOD, as it affects not only the ovaries but also involves metabolic and systemic complications like insulin resistance and an increased risk of cardiovascular diseases.
- Symptoms: PCOS often presents with more pronounced symptoms, including metabolic issues like obesity and insulin resistance, while PCOD primarily affects the reproductive system with fewer metabolic concerns.
- Treatment: Treatment for PCOS often involves managing both hormonal imbalances and metabolic issues, while PCOD treatment may focus more on regulating the menstrual cycle and managing cyst formation.
Polycystic Ovary Disease (PCOD) vs. Polycystic Ovary Syndrome (PCOS): Symptoms and Key Differences
Introduction to PCOS
Polycystic Ovary Syndrome (PCOS) is a hormonal and metabolic disorder that not only affects the ovaries but also impacts other systems in the body. Unlike Polycystic Ovarian Disease (PCOD), which primarily affects the ovaries, PCOS involves a broader range of symptoms and complications that influence the overall metabolism and health of the individual.
PCOS is characterized by an imbalance of male hormones (androgens) in women, which can result in significant changes to the female body. This hormonal disruption is linked to a variety of symptoms, some of which overlap with PCOD, though they tend to be more severe and lead to more serious health consequences in PCOS.
Key Differences between PCOD and PCOS
- Ovarian vs. Systemic Effects:
- PCOD: Primarily affects the ovaries. The cysts formed in PCOD are often due to immature eggs that don’t mature properly and result in fluid-filled cysts within the ovaries. This condition mainly disrupts the reproductive system.
- PCOS: Affects not only the ovaries but also other systems in the body, particularly metabolic and endocrine functions. It can lead to insulin resistance and cardiovascular issues, making it a more complex condition.
- Hormonal Imbalance:
- PCOD: While PCOD involves hormonal imbalances, the effects are usually less severe, and the condition does not typically involve significant metabolic issues.
- PCOS: The imbalance of androgens (male hormones) is much more pronounced, leading to symptoms like excess body and facial hair, acne, and more severe menstrual irregularities. This hormonal disruption can have long-term health consequences.
Key Symptoms of PCOS
The symptoms of PCOS are often more severe and can significantly impact a woman’s quality of life. Some of the common symptoms include:
- Severe Menstrual Irregularities: Women with PCOS often experience very irregular or even absent periods. These irregularities are more severe compared to those seen in PCOD, leading to difficulties in conceiving.
- Excess Facial and Body Hair: Known as hirsutism, this symptom is common in women with PCOS due to the elevated levels of male hormones. The excess hair may appear on the face, chest, or abdomen.
- Persistent Acne: Acne associated with PCOS tends to be persistent and difficult to clear up, unlike occasional breakouts that may occur with PCOD. The acne is often linked to the hormonal imbalance caused by excess androgens.
- Weight Gain and Difficulty Losing Weight: Women with PCOS may experience weight gain, especially around the abdomen, and find it difficult to lose weight due to insulin resistance.
Overlapping Symptoms of PCOD and PCOS
Though PCOD and PCOS are distinct conditions, many of their symptoms overlap, making it challenging to differentiate between the two at first. Common overlapping symptoms include:
- Irregular Periods: Both PCOD and PCOS can cause irregular menstrual cycles, though the severity may vary. In PCOS, the menstrual irregularities tend to be more severe.
- Acne: Both conditions can cause acne, although in PCOS, the acne is typically more persistent and harder to treat.
Long-Term Health Complications of PCOS
While PCOD tends to be less severe and primarily affects the reproductive system, PCOS is associated with long-term health complications. These complications may include:
- Insulin Resistance: Women with PCOS are at a higher risk for insulin resistance, which can lead to elevated blood sugar levels and an increased risk of developing type 2 diabetes.
- Cardiovascular Issues: The hormonal imbalances in PCOS, combined with metabolic disruptions, can increase the risk of heart disease and other cardiovascular problems.
- Infertility: Due to the irregular ovulation associated with PCOS, many women with the condition face challenges with fertility.
Diagnosis of PCOD and PCOS: A Comprehensive Approach
Diagnosing Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) requires a thorough and systematic approach to ensure accurate identification of the condition. Given the overlap in symptoms, it’s crucial for healthcare professionals to have a deep understanding of the differences between these two conditions. This knowledge enables the physician to differentiate between PCOD and PCOS more effectively, especially during the initial consultation.
Step 1: Case History and Symptoms Evaluation
The first step in diagnosing PCOD or PCOS is taking a detailed case history. A comprehensive history allows the physician to understand the patient’s symptoms and chief complaints.
During the consultation, healthcare providers should ask the patient about:
- Menstrual irregularities: Are the menstrual cycles irregular or absent?
- Physical changes: Are there signs of excess facial or body hair (hirsutism)?
- Skin issues: Has the patient experienced persistent acne or oily skin?
- Weight changes: Has there been unexplained weight gain or difficulty losing weight?
- Fatigue and energy levels: Is the patient experiencing fatigue, lethargy, or a lack of energy?
In addition to these questions, it’s important to inquire about any changes in the body, such as discoloration of the skin (often associated with insulin resistance), hair growth patterns, and other signs that may indicate hormonal imbalances. A detailed and accurate history can help differentiate between PCOD and PCOS and provide insight into the severity of the condition.
Step 2: Laboratory Tests for Confirmation
Once a comprehensive case history is taken, laboratory tests are necessary to confirm the diagnosis of PCOD or PCOS. These tests help assess hormone levels and rule out other conditions that may mimic the symptoms.
- Thyroid Function Tests: It’s essential to rule out thyroid disorders, as they can cause symptoms similar to PCOD and PCOS, such as menstrual irregularities and weight gain.
- Blood Sugar and Insulin Levels: Since insulin resistance is commonly associated with PCOS, checking blood sugar levels and insulin levels is crucial. Elevated insulin levels are a key indicator of insulin resistance, a hallmark of PCOS.
- Androgen Levels: Excessive levels of androgens (male hormones such as testosterone) are often found in women with PCOS. Blood tests can measure these levels, helping to confirm the presence of hormonal imbalance.
- Cholesterol Levels: Elevated cholesterol levels may indicate metabolic disturbances, which are common in women with PCOS.
Step 3: Ultrasound for Ovarian Morphology
An ultrasound is a key diagnostic tool for evaluating ovarian morphology. It provides a clear picture of the ovaries, allowing doctors to detect any changes in their appearance, such as the presence of cysts.
In women with PCOD or PCOS, ultrasound can help:
- Identify cysts in the ovaries: Multiple small cysts are often visible in the ovaries of women with PCOD or PCOS. These cysts are typically the result of immature or partially matured eggs that have not been released during ovulation.
- Assess the endometrial lining: The ultrasound can also help evaluate the endometrial lining of the uterus, checking for any abnormalities that could indicate underlying issues related to hormonal imbalance.
Step 4: Comprehensive Diagnosis and Treatment Planning
After gathering all relevant information through case history, laboratory tests, and ultrasound imaging, healthcare professionals can make an accurate diagnosis of either PCOD or PCOS. The results will guide the treatment approach, which may involve lifestyle changes, medication to regulate hormones, and addressing metabolic issues such as insulin resistance.
Differences between PCOD and PCOS: A Detailed Overview
Understanding the differences between Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) is crucial for accurate diagnosis and treatment. Below is a point-wise comparison to highlight the essential differences between these two conditions:
- Definition and Nature of the Conditions
- PCOD (Polycystic Ovarian Disease):
PCOD is a condition where the ovaries release immature or partially mature eggs. These immature eggs do not rupture as they should and are instead filled with fluid or water, leading to the formation of small cysts. This primarily affects the ovaries and does not extend to other systems in the body. - PCOS (Polycystic Ovary Syndrome):
PCOS is a complex endocrine and metabolic disorder. The name itself indicates that it involves more than just the ovaries. It affects both the hormonal (endocrine) system and the metabolism of the individual. PCOS is characterized by the growth of multiple cysts in both ovaries, which leads to disrupted ovulation and hormonal imbalances that affect other systems in the body.
- Prevalence of PCOD and PCOS
- PCOD:
PCOD is more common than PCOS, both in India and worldwide. It affects approximately 10% of women globally and is commonly observed during the adolescent and early reproductive years. - PCOS:
PCOS is less common than PCOD, affecting about 0.2% to 2.5% of women worldwide. This condition also typically arises during the early reproductive years, though it may sometimes be diagnosed later.
- Age of Onset
- PCOD:
PCOD generally occurs during the adolescent years or early reproductive years, often presenting at the time of puberty. It can be observed in young women as their bodies begin to undergo hormonal changes. - PCOS:
Like PCOD, PCOS also tends to present during the early reproductive years, but the onset of symptoms may sometimes be later in life, depending on the severity of the condition and the individual’s hormonal profile.
- Impact on Ovulation
- PCOD:
In PCOD, ovulation is typically less severely disrupted compared to PCOS. The primary issue is the formation of immature eggs that don’t rupture, leading to small cysts in the ovaries. Ovulation may still occur but may be irregular. - PCOS:
In PCOS, ovulation is more severely disrupted due to hormonal imbalances. This leads to irregular or absent periods, making it difficult for women with PCOS to conceive. The disruption of ovulation is one of the main factors contributing to infertility in women with PCOS.
- Hormonal Imbalance
- PCOD:
The hormonal imbalance in PCOD is usually milder. The primary issue is the presence of immature eggs that do not properly mature and ovulate, but the hormonal disruption tends to be limited to the ovaries. - PCOS:
In PCOS, there is a significant imbalance of male hormones (androgens), such as testosterone. Elevated androgen levels lead to symptoms like excess facial and body hair (hirsutism), acne, and thinning of the hair on the scalp. This hormonal imbalance affects multiple systems in the body, not just the ovaries.
- Cyst Formation
- PCOD:
The cysts formed in PCOD are small, and they result from the immature eggs that fail to ovulate. These cysts remain in the ovaries and do not typically spread or cause systemic issues. - PCOS:
In PCOS, multiple cysts develop in both ovaries, which can disrupt normal hormonal functions. These cysts are a hallmark of the condition, and the number of cysts may vary in size and appearance.
: A Detailed Overview of Hormonal Imbalance, Symptoms, and Fertility Impact 
Understanding the differences between Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) is vital for diagnosis and treatment. Below is a detailed comparison of these two conditions, focusing on hormonal imbalances, menstrual cycles, and fertility impacts. 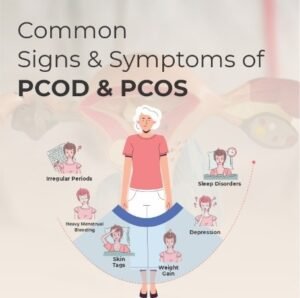
Age of Onset and Symptoms
- PCOD (Polycystic Ovarian Disease):
PCOD can begin during adolescence, but symptoms are often mild and may not be as pronounced until later in life. Some women may not experience significant metabolic or endocrine symptoms initially. However, in their twenties or thirties, the symptoms may become more noticeable as the condition persists. Since PCOD is a chronic issue, the symptoms can continue and evolve over time. - PCOS (Polycystic Ovary Syndrome):
PCOS can also begin in adolescence, but its symptoms are usually more pronounced and noticeable in the twenties to thirties. Due to the complex nature of the condition, it often involves more severe metabolic and endocrine disturbances. The symptoms may include significant changes in the menstrual cycle, fertility issues, and physical symptoms such as excessive hair growth and acne.
- Hormonal Imbalance
- PCOD:
In PCOD, the hormonal imbalance is usually mild. It primarily affects the balance of estrogen and progesterone, the two primary hormones involved in the female reproductive system. This hormonal disturbance may result in irregular ovulation and the formation of small cysts in the ovaries, but it is generally less severe than in PCOS. - PCOS:
PCOS is marked by a significant hormonal imbalance, particularly an elevation in androgen levels (male hormones, such as testosterone). This rise in male hormones can cause symptoms like hirsutism (excessive hair growth on the face and body), acne, and scalp hair thinning. This hormonal disturbance affects not only the ovaries but also other systems in the body, including metabolism and insulin regulation.
- Cyst Formation
- PCOD:
In PCOD, cysts tend to be small and are a result of immature eggs that do not rupture during ovulation. These small cysts remain in the ovaries but typically do not cause severe health issues. They are often discovered during routine imaging tests. - PCOS:
In PCOS, the cysts are usually larger and can be more persistent. They form when the ovaries do not release eggs properly, leading to the accumulation of fluid-filled sacs. If left untreated, these cysts may persist and cause ongoing reproductive and metabolic issues. Medical intervention is typically necessary to manage the condition.
- Menstrual Cycle
- PCOD:
In women with PCOD, menstrual cycles may be irregular or slightly delayed, but they are generally not severely impacted. Women with PCOD may experience slightly longer or irregular periods, but in most cases, they can still have regular menstrual cycles, although ovulation may be impaired. - PCOS:
In contrast, women with PCOS tend to have more severe menstrual irregularities. Periods can be highly irregular or even completely absent. This occurs because of the hormonal imbalance that disrupts the normal ovulatory cycle. In some cases, women with PCOS may not have any periods for several months, which can lead to fertility challenges.
- Fertility Impact
- PCOD:
While PCOD can affect fertility, the impact is generally milder compared to PCOS. Since the hormonal imbalance in PCOD is typically less severe, women with this condition may still be able to conceive, although they might experience difficulty due to irregular ovulation. However, with proper treatment, such as hormone therapy or lifestyle changes, many women with PCOD can successfully conceive. - PCOS:
In PCOS, the hormonal imbalances and disrupted ovulation can have a more significant impact on fertility. The condition is one of the leading causes of infertility in women. Irregular or absent ovulation makes it more difficult for women with PCOS to conceive naturally. However, with appropriate medical intervention, such as ovulation-inducing medications or assisted reproductive technologies like IVF, many women with PCOS are able to become pregnant.Fertility and Metabolic Impacts of PCOD vs. PCOS: A Comprehensive Comparison
A Comprehensive Comparison
When comparing Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS), it’s crucial to understand the significant differences in their impact on fertility, weight, and overall metabolic health. While both conditions share some common features, their effects on a woman’s reproductive and metabolic health can differ greatly.

Fertility Impact
- PCOD (Polycystic Ovarian Disease):
One of the distinguishing features of PCOD is that it rarely causes infertility. Women with PCOD may experience irregular ovulation, but most can still conceive with minor medical assistance or by implementing lifestyle changes such as improved diet and exercise. The fertility issues related to PCOD are generally not as severe, and many women with this condition can get pregnant naturally or with minimal intervention. - PCOS (Polycystic Ovary Syndrome):
On the other hand, PCOS is frequently linked with infertility due to more pronounced hormonal imbalances that disrupt the ovulatory cycle. Although it is not a certainty that women with PCOS will face infertility, the condition significantly affects their ability to conceive naturally. Furthermore, women with PCOS are at a higher risk of miscarriages and other pregnancy complications. The hormonal imbalance associated with PCOS makes pregnancy challenging, and medical intervention such as fertility treatments may be required.
Weight Impact
- PCOD (Polycystic Ovarian Disease):
Women with PCOD often experience weight gain, but this can generally be managed through lifestyle changes. Maintaining a healthy diet, regular physical activity, and weight management strategies can help keep the condition under control. Weight gain in PCOD is typically not as severe or persistent as in PCOS, and with proper management, weight can be maintained at a healthy level. - PCOS (Polycystic Ovary Syndrome):
In contrast, weight gain in PCOS is more difficult to manage. Many women with PCOS find it challenging to lose weight, even with strict diet and exercise regimens. This difficulty is often due to insulin resistance, a common feature of PCOS. Insulin resistance leads to increased fat storage and continuous weight gain, making it harder for women to maintain a healthy weight. In many cases, weight gain can become significant and difficult to reverse without medical intervention.
Metabolic Impact
- PCOD (Polycystic Ovarian Disease):
The metabolic impact of PCOD is minimal, with the primary effects limited to the ovaries. PCOD does not typically cause disturbances in other parts of the body, such as blood sugar regulation or cardiovascular health. Women with PCOD may experience some metabolic shifts, but these are generally not as severe as those seen in PCOS. - PCOS (Polycystic Ovary Syndrome):
PCOS, on the other hand, is strongly associated with metabolic syndrome. This includes serious health concerns such as insulin resistance, type 2 diabetes, and high cholesterol. The insulin resistance in PCOS can increase the risk of developing these conditions, which not only affect the ovaries but also impact overall metabolic health. Women with PCOS may experience difficulties with blood sugar regulation, and are at an increased risk for developing long-term complications like heart disease and diabetes.
Health Complications and Treatment Approaches for PCOD and PCOS
Both Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) can lead to a variety of health complications, but the severity and long-term health risks differ between the two conditions. Understanding these differences is crucial for effective diagnosis and treatment. Here’s an in-depth look at the potential health complications and treatment strategies for each condition.
Health Complications
- PCOD (Polycystic Ovarian Disease):
PCOD generally does not lead to severe, long-term health complications if managed properly. The condition mainly affects the ovaries, leading to mild hormonal imbalances. While these imbalances can cause some mild mood swings or emotional stress, they typically do not cause significant issues like depression or anxiety. Additionally, the health impact on other systems of the body is minimal, and PCOD patients can manage the condition with proper lifestyle adjustments, reducing the risk of complications over time. - PCOS (Polycystic Ovary Syndrome):
In contrast, PCOS involves not just the ovaries, but also impacts other metabolic systems in the body. The hormonal imbalances in PCOS can cause more severe mood swings, depression, and anxiety due to the disruption of the hormonal regulation. These mental health issues often arise from the more significant endocrine disruption that occurs with PCOS, and they can be harder to manage without medical intervention. Additionally, PCOS is associated with long-term complications such as insulin resistance, type 2 diabetes, and high cholesterol, which can further impact overall health.
Treatment Approaches
- PCOD (Polycystic Ovarian Disease):
The treatment for PCOD primarily revolves around lifestyle changes. This includes dietary modifications, regular physical activity, and weight management. The condition is typically manageable with these adjustments alone, and medication is not always necessary. Doctors will often recommend a healthy lifestyle first, emphasizing exercise and a balanced diet to control symptoms. In some cases, if the condition worsens or if symptoms become more pronounced, mild medications or hormonal treatments may be suggested, but this is rare. - PCOS (Polycystic Ovary Syndrome):
The treatment approach for PCOS is more complex and requires a combination of lifestyle changes along with medical intervention. Alongside adjustments to diet and exercise, hormonal therapy (such as birth control pills or other hormone-regulating medications) is often prescribed to manage symptoms like irregular periods, acne, and excessive hair growth. Additionally, for women with insulin resistance, insulin-sensitizing medications (like Metformin) may be used to help regulate blood sugar levels and reduce the risk of developing type 2 diabetes. The treatment plan for PCOS is highly individualized, and doctors may prescribe different medications depending on the severity of symptoms and the patient’s health needs.
Reversibility, Risk, and Severity: Differences between PCOD and PCOS
Understanding the differences between Polycystic Ovarian Disease (PCOD) and Polycystic Ovary Syndrome (PCOS) is crucial for diagnosing, managing, and treating these conditions effectively. While both involve hormonal imbalances and impact the ovaries, the severity, reversibility, long-term risks, and treatment paths differ significantly between the two. Here, we’ll explore these differences in greater detail, especially focusing on reversibility, associated risks, and severity.
Reversibility of Symptoms
- PCOD (Polycystic Ovarian Disease):
One of the most significant aspects of PCOD is that its symptoms are often reversible with lifestyle modifications. Because the condition is generally mild, with minimal impact on other parts of the body, women with PCOD can often manage or reverse symptoms like irregular periods, weight gain, and acne through dietary changes, exercise, and weight management. No medical interventions, such as hormone therapy or insulin management, are usually necessary. Thus, with proper lifestyle adjustments, the symptoms can often improve or disappear. - PCOS (Polycystic Ovary Syndrome):
In PCOS, while symptoms can be managed with lifestyle changes, full reversibility is often not achievable. This condition tends to be more severe, with systemic effects on the body. Managing PCOS typically requires long-term medical care and medical interventions, including hormonal therapy and possibly insulin management. In some cases, the symptoms may not be fully reversible, but they can be controlled with continuous medical treatment and lifestyle changes. Therefore, it may take a significant amount of time to see improvements, and in some cases, complete reversal of symptoms may not be possible.
Risk of Chronic Illness
- PCOD:
When PCOD is properly managed, the risk of chronic diseases is minimal. Since the condition primarily affects the ovaries without spreading to other organs or systems, there is no significant increase in the risk of heart disease, type 2 diabetes, or certain cancers. However, PCOD still requires management to prevent any possible complications in the future, but with early intervention, the overall chronic disease risk is minimal. - PCOS:
On the other hand, PCOS carries a higher risk of chronic illnesses, including heart disease, type 2 diabetes, and certain cancers. Due to its systemic effects and the impact of insulin resistance, PCOS can lead to metabolic disturbances that affect other organs and increase the likelihood of these chronic conditions. Women with PCOS are also at a higher risk for high cholesterol, which contributes to cardiovascular issues. Therefore, it’s essential for women with PCOS to undergo regular monitoring and medical treatment to manage these risks.
Severity of the Conditions
- PCOD:
PCOD is generally less severe than PCOS and is considered easier to manage. Since it primarily affects the ovaries and causes mild hormonal imbalances, it typically does not cause major disruptions to the body’s overall function. It can be effectively managed with lifestyle changes, making it a less complex condition. - PCOS:
PCOS, on the other hand, is more severe and has systemic effects. It involves not only hormonal imbalances but also metabolic disruptions that affect various parts of the body. Women with PCOS often require medical interventions, such as hormone therapy and insulin-sensitizing medications. The condition may also cause significant disruptions to the menstrual cycle, fertility, and overall hormonal balance, requiring a more complex treatment approach.
Management of PCOD and PCOS through Naturopathy
Both PCOD and PCOS can be managed through naturopathy alongside conventional medical treatments. Naturopathic approaches emphasize natural remedies, dietary changes, and lifestyle adjustments to support the body’s natural healing processes. Here’s how naturopathy can help manage these conditions:
PCOD Management in Naturopathy
- Dietary Modifications:
A healthy, balanced diet rich in whole foods, low glycemic index foods, and high in fiber can help regulate insulin levels and support ovarian health. - Herbal Supplements:
Herbs such as Spearmint tea or Saw Palmetto may help manage symptoms like excess hair growth and acne. - Stress Management:
Techniques like yoga, meditation, and deep breathing exercises can help reduce stress, which is crucial for hormonal balance and overall well-being. - Physical Activity:
Regular exercise can help with weight management and improve insulin sensitivity.
PCOS Management in Naturopathy
- Comprehensive Lifestyle Modifications:
For PCOS, lifestyle changes are crucial, but additional support through naturopathy can be beneficial. This includes dietary modifications to address insulin resistance, regular physical activity, and stress-reducing techniques. - Herbal Medicine:
Certain herbs like Vitex (Chaste Tree) and Spearmint may help balance hormones and reduce excess hair growth. Cinnamon and Berberine can be used to improve insulin sensitivity. - Detoxification:
Detox programs can help the body eliminate toxins that might exacerbate hormonal imbalances and reduce inflammation. - Support for Metabolic Health:
Naturopathic treatments can support metabolic health by including antioxidant-rich foods, supplements like Omega-3 fatty acids, and the use of herbs known to aid in insulin regulation.
Main Approaches in Naturopathy for Managing PCOS
Naturopathy offers a holistic and natural approach to managing conditions like PCOS (Polycystic Ovary Syndrome). The main principles of naturopathic treatment focus on restoring the body’s natural balance and enhancing overall well-being. These approaches include:
- Holistic Approach:
The holistic approach in naturopathy aims to treat the whole person, considering not only the physical symptoms but also the emotional, mental, and spiritual aspects of health. This approach emphasizes mind-body wellness, which includes stress management, relaxation techniques, and improving emotional well-being to restore balance in the body. - Restoring Hormonal Balance Naturally:
One of the key aspects of managing PCOS through naturopathy is restoring hormonal balance naturally. This includes using herbal remedies, nutritional supplements, and lifestyle changes to balance the body’s hormones and improve conditions like insulin resistance, androgen excess, and menstrual irregularities, which are common in PCOS. - Detoxification:
Detoxification plays a critical role in PCOS management. Naturopathy emphasizes natural detoxification through herbs, diet, and specific lifestyle modifications to help the body eliminate toxins. This process helps reduce inflammation, improve liver function, and regulate hormonal levels, which can ease symptoms of PCOS. - Lifestyle Correction:
Correcting lifestyle habits is a significant aspect of naturopathic treatment for PCOS. This includes dietary modifications, regular physical activity, adequate sleep, and stress management techniques. Healthy lifestyle changes help to manage weight, improve insulin sensitivity, and reduce the severity of PCOS symptoms.
Dietary Management in PCOS
Dietary management plays a crucial role in managing PCOS and addressing its symptoms. Studies have shown that the majority of women with PCOS consume an imbalanced diet lacking essential nutrients, which exacerbates the condition.
Common Nutrient Deficiencies in PCOS
Many women with PCOS suffer from nutrient deficiencies, which can worsen hormonal imbalances and metabolic dysfunction. Common deficiencies found in PCOS patients include:
- Fiber: Fiber helps regulate blood sugar levels and improve insulin sensitivity. It is essential for digestive health and reducing inflammation, both of which are crucial for PCOS management.
- Omega-3 Fatty Acids: Omega-3s help reduce inflammation and support heart and metabolic health. These are particularly important for women with PCOS, as they may be at a higher risk of cardiovascular issues due to insulin resistance.
- Calcium: Calcium is essential for bone health, which can be compromised in women with PCOS due to hormonal imbalances.
- Magnesium: Magnesium is involved in over 300 biochemical reactions in the body, including those that regulate blood sugar and support heart health.
- Zinc: Zinc plays a role in immune function and skin health, and it can help reduce acne, a common symptom in women with PCOS.
- Vitamins: Women with PCOS are commonly deficient in several vitamins, including:
- Folic acid: Important for cellular function and the prevention of birth defects.
- Vitamin C: An antioxidant that helps manage inflammation and supports overall immune health.
- Vitamin B12: Essential for energy production and metabolic function.
- Vitamin D: Crucial for hormonal balance and insulin sensitivity, and many women with PCOS have low vitamin D levels.
Excess Nutrients in PCOS
In addition to deficiencies, some nutrients may be consumed in excess by women with PCOS, which can contribute to further metabolic disturbances. These include:
- Sucrose (Sugar): Excess sugar intake can exacerbate insulin resistance and weight gain, two major concerns for women with PCOS. High sugar consumption can lead to elevated blood sugar and insulin levels, worsening the hormonal imbalance associated with the condition.
- Sodium: High sodium intake, often found in processed foods, can lead to high blood pressure and other cardiovascular issues. It is important for women with PCOS to limit their sodium intake to manage overall health.
- Total Fats and Saturated Fatty Acids: Excessive intake of unhealthy fats, particularly saturated fats, can increase inflammation, contribute to weight gain, and worsen insulin resistance. A low-fat, balanced diet is important for managing PCOS effectively.
- Cholesterol: High cholesterol levels can be a concern in PCOS, particularly for those with insulin resistance. Managing cholesterol levels through a healthy diet and lifestyle is important for reducing the risk of cardiovascular diseases.
Nutritional Management in PCOS: Key Nutrients and Supplements

In managing PCOS (Polycystic Ovary Syndrome), nutrition plays a crucial role. Research has identified specific nutrient deficiencies and excesses in women with PCOS that contribute to the condition’s symptoms and complications. By addressing these imbalances through targeted supplements, significant improvements can be made in managing PCOS symptoms and overall health.
Common Nutrient Deficiencies and Excesses in PCOS Patients
Women with PCOS often experience deficiencies in essential nutrients, such as magnesium, zinc, calcium, vitamin D, and omega-3 fatty acids. At the same time, they may have excess levels of sucrose (sugar), sodium, saturated fats, and cholesterol. Proper dietary management aims to correct these imbalances by introducing the right nutrients while reducing those in excess.
Key Supplements for PCOS Patients
Recent studies have shown that specific nutrient supplementation can greatly benefit women with PCOS, particularly when it comes to magnesium, zinc, calcium, and vitamin D.
- Magnesium, Zinc, Calcium, and Vitamin D Supplements
Research has shown that supplementation of these nutrients can significantly improve health outcomes in PCOS patients. When women with PCOS are given a combination of magnesium, zinc, calcium, and vitamin D for a period of time (such as 30 days), there is a noticeable reduction in symptoms like UTI (urinary tract infections) and excess testosterone levels, which are typically elevated in PCOS patients. These nutrients help in:- Reducing testosterone levels: PCOS is often marked by high levels of testosterone, a male hormone that leads to symptoms such as excess facial hair and acne. Supplementation with magnesium, zinc, calcium, and vitamin D has been shown to reduce these elevated levels.
- Improving metabolic function: These nutrients support the body’s metabolism, which is crucial in managing the insulin resistance and metabolic disorders commonly associated with PCOS.
- Myo-Inositol
Another beneficial supplement for PCOS patients is myo-inositol. This supplement has been found to be as effective as metformin, a commonly prescribed drug for insulin resistance in PCOS patients. Myo-inositol improves the clinical and metabolic profile in women with PCOS, helping to regulate insulin sensitivity and improve ovarian function. In addition to its benefits for insulin resistance, myo-inositol can help reduce the risk of metabolic disorders such as type 2 diabetes.
Clinical Evidence Supporting Supplementation
Several studies have shown the positive impact of these nutrient supplements on PCOS patients. For example, the supplementation of magnesium, zinc, calcium, and vitamin D not only reduces symptoms but also improves the metabolic profile by reducing testosterone levels and improving overall ovarian function. Furthermore, myo-inositol supplementation has been shown to be as effective as metformin in managing insulin resistance, which is a cornerstone of PCOS management.
Dietary Sources of Myo-Inositol and Key Nutrients for PCOS Management
In managing PCOS (Polycystic Ovary Syndrome), dietary interventions play a crucial role, especially when it comes to providing essential nutrients that support hormonal balance and metabolic health. One such nutrient is myo-inositol, which has been shown to be beneficial in PCOS treatment, offering a natural alternative to medications like metformin for insulin resistance. Below, we discuss food sources that can provide myo-inositol and other important nutrients to help manage PCOS effectively.
Myo-Inositol-Rich Foods
While myo-inositol is often used in supplement form to help manage PCOS, there are natural food sources that contain myo-inositol and can be included in the diet:
- Citrus Fruits
Citrus fruits such as oranges, grapefruits, and lemons are excellent sources of myo-inositol. These fruits not only provide myo-inositol, but also are rich in vitamin C, which supports overall immune health. - Blueberries
Blueberries are another good source of myo-inositol. They also contain antioxidants that can help reduce inflammation and improve overall health. - Bananas
Bananas provide myo-inositol along with essential vitamins and minerals, making them a great addition to a PCOS-friendly diet. - Raisins
Like bananas, raisins also contain myo-inositol and offer a convenient snack option. - Lentils
Lentils are not only a good source of myo-inositol but also provide ample fiber, which is typically deficient in PCOS patients. Lentils are also rich in protein, making them a great plant-based protein source. - Whole Grains
Foods like rice bran and whole grains (such as oats, quinoa, and barley) are rich in myo-inositol and provide fiber, which is essential for managing PCOS and improving insulin sensitivity. - Nuts and Seeds
Peanuts, almonds, and other nuts are not only good sources of myo-inositol, but they also offer healthy fats and protein. These fats are important for supporting hormonal balance. - Honey
Honey is another food that contains trace amounts of myo-inositol and can be used as a natural sweetener in the PCOS diet.
Other Nutrients Essential for Managing PCOS
In addition to myo-inositol, certain other nutrients are particularly beneficial for women with PCOS. These nutrients can help address deficiencies commonly found in PCOS patients and improve overall health.
- Magnesium and Zinc
Magnesium and zinc are essential for managing PCOS symptoms. Foods such as avocados, almonds, walnuts, and pistachios are rich in both magnesium and zinc. These nutrients help support hormone regulation and reduce symptoms like acne and excess facial hair. - Calcium and Vitamin D
Studies have shown that calcium and vitamin D supplementation is effective in reducing testosterone levels and improving metabolic function in women with PCOS. Foods like leafy green vegetables, fortified dairy products, and sunlight exposure can help ensure adequate intake of these nutrients. - Fiber
Women with PCOS often suffer from fiber deficiencies. High-fiber foods, such as vegetables, fruits, and whole grains, help support digestive health and insulin sensitivity, which is essential for managing PCOS. - Healthy Fats
Healthy fats from avocados, nuts, and seeds provide essential fatty acids that support hormone balance and reduce inflammation in the body.
Herbal Remedies and Dietary Adjustments for Managing PCOS
When managing PCOS (Polycystic Ovary Syndrome), dietary modifications and herbal remedies play a significant role in balancing hormones and improving overall metabolic health. Incorporating certain foods and avoiding others, along with adding beneficial herbal remedies, can help manage the symptoms of PCOS effectively. Below, we will discuss the best dietary options, foods to avoid, and herbal remedies that can support women with PCOS.
Dietary Adjustments for PCOS
- Healthy Fats and Seeds
Including healthy fats in the diet is essential for managing PCOS, as they support hormone regulation and reduce inflammation. Foods such as avocados, nuts, and seeds are great sources of healthy fats. Specifically, chia seeds and pumpkin seeds are rich in magnesium, an important mineral that can help reduce insulin resistance and support metabolic health in PCOS patients. Olive oil, known for its anti-inflammatory properties, should also be incorporated into meals. - Anti-Inflammatory Foods
In addition to healthy fats, anti-inflammatory foods like turmeric, ginger, and green tea should be included in the diet. These ingredients help reduce inflammation in the body, which can contribute to the hormonal imbalances seen in PCOS. - Foods to Avoid
Certain foods should be minimized or excluded from the diet of those with PCOS:- Processed foods: These often contain unhealthy fats, added sugars, and preservatives that can worsen PCOS symptoms.
- Refined sugar: High sugar intake can exacerbate insulin resistance and contribute to weight gain in PCOS patients.
- Dairy: Dairy products can potentially aggravate PCOS symptoms due to their hormone content.
- Gluten: Foods containing gluten, such as wheat products, may also cause inflammation in some PCOS patients, and reducing gluten intake may improve symptoms.
Herbal Remedies for PCOS
In addition to dietary changes, certain herbal remedies have been found to be highly effective in managing PCOS symptoms, particularly in reducing androgen levels, improving insulin sensitivity, and supporting overall hormonal balance. Below are some of the key herbs that can help:
- Spearmint Tea
Spearmint tea is one of the most well-researched herbal remedies for PCOS. Studies have shown that spearmint has anti-androgenic effects, meaning it helps reduce the elevated levels of male hormones (androgens) that are commonly found in PCOS patients. Spearmint tea can be a natural alternative to medications that target androgen levels, reducing symptoms like excess facial hair (hirsutism).
In addition to its anti-androgenic effects, spearmint tea is also beneficial for stress reduction and promoting hormone balance. Regular consumption of spearmint tea can help regulate insulin levels, support metabolic health, and potentially aid in reducing ovarian cysts.
- Cinnamon
Cinnamon is another herb that plays a significant role in regulating insulin levels in PCOS patients. It can help improve insulin sensitivity, which is crucial for managing PCOS. Consuming cinnamon regularly, either in food or as a tea, can support metabolic health or assist in reducing symptoms of PCOS. - Chaste Tree Berry (Vitex)
Chaste tree berry, also known as Vitex, has been used for centuries to support hormonal balance. It is particularly useful for regulating menstrual cycles in women with PCOS. This herb can help normalize progesterone levels, which is crucial for addressing irregular periods and improving fertility in PCOS patients. - Green Tea
Green tea is rich in antioxidants and polyphenols, which support overall health. Studies have shown that green tea can help improve insulin sensitivity, reduce androgen levels, and promote weight loss, making it a valuable addition to the diet of PCOS patients. - Fenugreek
Fenugreek is an herb that has been found to have beneficial effects on insulin regulation in PCOS. It can help reduce blood sugar levels, which is important for women with insulin resistance, a common feature of PCOS. - Saw Palmetto
Saw palmetto is another herb known for its anti-androgenic properties. It works by inhibiting the production of dihydric testosterone (DHT), a potent androgen that contributes to PCOS symptoms like hair loss and acne.
Hydrotherapy Management for PCOS: The Tonic Sitz Bath
Hydrotherapy is an effective complementary treatment approach in managing PCOS (Polycystic Ovary Syndrome). One of the notable techniques in hydrotherapy is the Tonic Sitz Bath, which can help improve circulation, reduce inflammation, and support overall pelvic health. Below is a detailed explanation of this treatment, its benefits, and how it is performed.
What is a Tonic Sitz Bath?
A Sitz Bath involves immersing only the pelvic area in warm or hot water, which contrasts with a Hip Bath, where the entire lower body is immersed. The main aim of a Tonic Sitz Bath is to target the pelvic region specifically to improve blood circulation, reduce pelvic congestion, and promote relaxation in the area. This therapeutic practice is particularly beneficial for PCOS patients, as it helps to reduce abdominal discomfort, stress, and inflammation associated with the condition.
Procedure for the Tonic Sitz Bath
The Tonic Sitz Bath involves the following steps:
- Preparation
The patient should have access to a bucket or tub large enough to immerse the pelvic region comfortably. The water temperature should be maintained between 55 to 65 degrees Celsius (130 to 149 degrees Fahrenheit) to ensure it is hot enough to improve circulation but not so hot as to cause burns or discomfort. - Immersion
The patient is instructed to sit in the tub with their legs immersed in hot water, ensuring that only the pelvic region is submerged. The water should cover the lower abdomen and hip area, which is beneficial for targeting the reproductive organs, and may help relieve symptoms like pelvic pain and bloating that can be common in PCOS. - Wet Pack on the Head
In addition to the foot bath, a wet cold pack should be placed on the patient’s head. The cold pack helps to balance the hot therapy and encourages a cooling effect on the body’s upper regions. This contrast between hot and cold can enhance the therapeutic benefits and promote relaxation. - Massage
while in the sitz bath, the patient should be encouraged to gently rub their hips, abdomen, and thighs. This massage should be done for about 1 to 3 minutes and can be continued throughout the duration of the bath. The massage helps stimulate circulation and relaxes tense muscles, which can be particularly beneficial for PCOS patients experiencing bloating or muscle tension. - Duration
the bath should be continued for 15 to 20 minutes, allowing the patient to fully immerse in the therapeutic effects. It is recommended that this procedure be done regularly, depending on the patient’s comfort level and specific symptoms.
Benefits of the Tonic Sitz Bath for PCOS
The Tonic Sitz Bath offers several benefits for PCOS patients, including:
- Improved Blood Circulation: The warm water helps improve circulation in the pelvic region, which can promote healing and reduce congestion in the ovaries and surrounding tissues.
- Reduction of Inflammation: Regular use of hot and cold water therapy can reduce inflammation, which is often a contributing factor to the hormonal imbalances seen in PCOS.
- Pelvic Pain Relief: Many women with PCOS experience discomfort or pain in the pelvic area. The warm water helps to relax the muscles and soothe pain, making it an effective natural remedy.
- Stress Relief: The relaxation from the warm water and the gentle massage can also help reduce stress and promote overall relaxation. Stress is a known factor that can exacerbate PCOS symptoms, so any therapy that reduces stress can be very beneficial.
- Hormonal Balance: By improving circulation and reducing inflammation, the Sitz Bath can support hormonal balance, which is crucial for PCOS patients struggling with irregular periods, cyst development, and other symptoms related to hormonal imbalances.
- Enhanced Metabolic Function: Regular hydrotherapy can also support metabolic health by improving circulation, which may aid in better absorption of nutrients and overall better metabolic function.
Hydrotherapy Techniques for Managing PCOS: Short Cold Pack and Targeted Water Therapy
Hydrotherapy plays an important role in the management of Polycystic Ovary Syndrome (PCOS) by using thermic and mechanical effects to provide relief from various symptoms. Among the different techniques available, two stand out: the Tonic Sitz Bath and Targeted Water Therapy, which offer unique benefits to patients suffering from this condition.
Thermic and Mechanical Effects on Reflex Areas
The primary aim of these hydrotherapy techniques is to stimulate thermic (heat) and mechanical (pressure) effects on key reflex areas in the body. By targeting specific regions of the abdomen and pelvis, hydrotherapy improves nerve response, increases blood circulation, and supports hormonal balance. These therapeutic effects can be especially beneficial for PCOS patients, as they help address various issues like pelvic pain, irregular menstruation, and hormonal imbalances.
Short Cold Pack with Sheet over the Abdomen
One of the most beneficial alternative therapies for patients with PCOS, particularly those who are weak or unable to practice the Tonic Sitz Bath, is the use of a Short Cold Pack applied over the abdomen. This technique is known to provide a tonic effect and can be particularly helpful for patients experiencing anemia and irregular menstruation.
- Procedure
to perform this treatment, a cold pack is applied to the lower abdomen area, targeting the hypo gastric region (the area just below the navel and above the pelvic bone). The cold pack should be applied with a dry sheet covering the abdomen for a few minutes. This will stimulate the body, promote circulation, and support the hormonal balance essential for regulating the menstrual cycle. - Benefits
the application of a cold pack provides a tonic effect that can help with fatigue, particularly for those who feel weak due to PCOS-related symptoms. The cold helps reduce inflammation in the abdomen and pelvic region, promoting improved circulation and reducing discomfort. It is especially effective for patients with irregular menstruation or anemia.
Targeted Water Therapy for the Lower Abdomen and Pelvic Area
Another effective hydrotherapy treatment for PCOS patients involves targeted water pressure therapy applied to the lower abdomen, particularly the hypo gastric region.
- Procedure
In this method, a cold or cool water spray or fan nozzle is applied directly to the hypo gastric area, ensuring that the pressure and temperature are controlled to avoid discomfort. The goal is to focus the therapy on the pelvic viscera, including the uterus, ovaries, and bladder. By concentrating the pressure on this specific area, the therapy promotes blood flow, improves nerve function, and helps stimulate the body’s natural healing processes. - Types of Application
The water can be delivered using different methods:- Jet therapy, which involves a steady, pressurized stream of cold water.
- Percussion therapy, where the water is delivered in short, rapid bursts to stimulate circulation.
- Fan or spray nozzle, which evenly distributes cool water across the target area.
This technique can be done with varying pressures, ensuring that the water reaches the hypo gastric region without causing discomfort or pain. The duration and intensity should be adjusted based on the patient’s tolerance and specific symptoms.
- Benefits
- Hormonal Regulation: The application of water pressure in the hypo gastric region stimulates the ovaries and uterus, promoting hormonal balance and improving the regularity of the menstrual cycle.
- Pelvic Health: This therapy improves circulation in the pelvic area, which can help alleviate symptoms such as pelvic pain and bloating associated with PCOS.
- Reduced Inflammation: The cooling effect helps reduce inflammation, particularly in the ovaries, potentially aiding in the reduction of cysts and improving overall ovarian health.
Lumbar Region Pressure Therapy
A related therapy focuses on the lumbar (lower back) region. Cold therapy can be applied with sufficient pressure to this area to create a reflex effect on the lower abdomen and pelvic organs. This can be especially helpful for PCOS patients who experience lower back pain or pelvic discomfort due to hormonal imbalances.
- Procedure
In this therapy, a cold pressurized stream of water (using a jet or fan nozzle) is directed at the lumbar region, stimulating the reflexes in the lower abdomen and pelvic areas. This can help promote circulation, reduce inflammation, and relieve any muscular tension or pain in the pelvic area. It can also contribute to the relief of irregular menstruation by helping to regulate the hormonal fluctuations that cause menstrual disruptions. - Benefits
- Pain Relief: The cold pressure therapy applied to the lumbar region helps relax the muscles of the lower back, reducing discomfort and pain.
- Pelvic Health Support: By stimulating reflex points in the lumbar area, this therapy enhances circulation to the ovaries and uterus, improving hormonal function and potentially alleviating some symptoms of PCOS.
- Improved Menstrual Regularity: Regular treatment with cold pressure therapy on the lumbar region can support regular menstruation by improving blood flow and hormonal balance.
Hydrotherapy and MA Therapy for Managing PCOS: Therapeutic Approaches for Effective Symptom Relief
Hydrotherapy is a promising approach in the management of Polycystic Ovary Syndrome (PCOS), particularly for improving circulation, stimulating metabolism, and promoting overall wellness. These treatments leverage both hot and cold therapies to activate the body’s reflex zones and improve hormonal balance. Below is a breakdown of the various hydrotherapy techniques and their benefits, followed by an introduction to MA Therapy as an additional treatment for PCOS.
Hot and Cold Application to the Feet
One of the simplest yet most effective hydrotherapy treatments involves applying hot and cold water alternately to the feet. The feet are considered a major reflex area in the body, with points that correspond to various internal organs, including the uterus, ovaries, and abdominal viscera. This technique stimulates these organs by increasing vascular activity, which can aid in restoring menstruation and improving overall pelvic health.
- Procedure
- A cold application (such as cold water or ice) is applied to the feet for a short duration.
- This is followed by a hot application (using warm or hot water) to the feet, helping to dilate blood vessels and enhance circulation.
- The alternating hot and cold treatments are repeated for a few minutes.
- Benefits
- Increased Vascular Activity: The contrast between hot and cold therapies helps stimulate blood flow, supporting the health of reproductive organs and hormonal balance.
- Regulating Menstrual Cycle: The procedure is especially beneficial for those with irregular menstruation, as it can help stimulate the uterine muscles and improve menstrual flow.
- Supports Abdominal Health: By stimulating the feet’s reflex zones, this treatment has a positive impact on abdominal viscera, promoting overall digestive health.
Cold Immersion Bath for Metabolic Stimulation
The Cold Immersion Bath is another effective hydrotherapy technique, especially for those dealing with metabolic issues such as insulin resistance and overweight conditions, which are common among PCOS patients. This therapy focuses on stimulating the overall metabolism, improving circulation, and enhancing energy levels.
- Procedure
- In this treatment, the patient immerses their body (or specific areas such as the feet or lower body) into cold water for a specified period of time.
- The cold temperature helps activate the body’s metabolic processes and can be especially helpful for insulin resistance.
- Benefits
- Metabolic Boost: Cold immersion helps stimulate metabolic activity, supporting fat burning and improving insulin sensitivity.
- Overcoming Lack of Appetite: This therapy is also beneficial for patients who experience a lack of appetite, which can occur in some PCOS cases. Cold immersion may help regulate the appetite and improve overall nutrition.
- Weight Management: For those struggling with weight gain associated with PCOS, this treatment can help promote a more balanced metabolic rate, aiding in weight loss.
MA Therapy for PCOS
In addition to hydrotherapy, MA Therapy is another holistic treatment that has shown significant benefits for PCOS patients. MA Therapy (Mind-Body-Awareness Therapy) integrates mental, emotional, and physical healing practices to address the root causes of PCOS symptoms. This therapy focuses on the mind-body connection, helping patients reduce stress, hormonal imbalances, and other PCOS-related symptoms.
- How MA Therapy Works
- MA Therapy uses a variety of techniques including relaxation exercises, breathing techniques, mindfulness meditation, and visualization to promote emotional and physical balance.
- It targets the autonomic nervous system to regulate hormonal function and reduce the impact of stress on the body.
- Benefits
- Hormonal Regulation: By reducing stress and improving emotional well-being, MA Therapy can help regulate hormonal imbalances often seen in PCOS.
- Improved Menstrual Health: Through mind-body techniques, patients can experience better menstrual cycle regulation and reduce irregular periods.
- Mental Well-Being: MA Therapy can also reduce symptoms of anxiety and depression, which are often associated with PCOS, by promoting emotional healing and balance.
The Role of Mud Therapy in Managing PCOS: A Naturopathic Approach
Mud therapy, a popular modality in naturopathy, offers a natural way to help manage symptoms associated with Polycystic Ovary Syndrome (PCOS). This therapeutic treatment is based on the healing properties of mud, which is believed to restore balance to the body by engaging with the earth element. Through both direct and indirect applications, mud therapy can enhance relaxation, regulate hormonal levels, and promote overall well-being.
Types of Mud Therapy Applications
Mud therapy can be applied in two main ways: direct and indirect applications. Each approach offers distinct benefits, particularly in the context of hormonal imbalances and stress reduction associated with PCOS.
- Direct Application
In this method, mud is applied directly to the body, often to the abdomen or other affected areas. The therapy typically involves a 45-minute session in which the patient is exposed to sunlight to enhance the therapeutic effects of the mud. The direct application of mud helps to detoxify the body, promote skin rejuvenation, and activate the earth element within the body. By restoring balance to the earth element, mud therapy is believed to help regulate hormonal imbalances, which are a hallmark of PCOS. - Indirect Application
The indirect method involves applying a mud patch to specific areas of the body, such as the abdomen or forehead. This less direct approach still offers valuable benefits, promoting relaxation, stress relief, and cellular radiation. The mud patch works by gradually absorbing toxins from the skin and providing a calming effect to the body. Additionally, this method helps activate hormones in a more subtle and gentle manner.
Benefits of Mud Therapy for PCOS
The therapeutic use of mud has a range of benefits for individuals with PCOS:
- Restoration of Hormonal Balance: Mud therapy is believed to activate and balance hormonal levels, particularly in areas where the body is experiencing disruptions. By applying mud to the body, especially the abdomen, it can help regulate estrogen and insulin levels, which are often impaired in PCOS.
- Stress Reduction: Research has shown that mud therapy can be effective in reducing stress by lowering cortisol levels, the body’s primary stress hormone. This is particularly important for PCOS patients, as high stress levels can exacerbate symptoms, including irregular menstruation and hormonal imbalance. Reducing cortisol through mud therapy can help restore a sense of calm, thus improving overall emotional and physical well-being.
- Improvement of Physical and Emotional Relaxation: As mud therapy promotes relaxation, it can reduce symptoms such as fatigue, anxiety, and mood swings, all of which are common in PCOS. By soothing the body and mind, mud therapy helps patients cope with the emotional stress that often accompanies the condition.
- Enhancement of the Earth Element: Mud, being a product of the earth, is thought to resonate with the earth element within the human body. This connection is believed to improve the health of internal organs, particularly those affected by PCOS, such as the ovaries, uterus, and endocrine system. Restoring balance to these organs can help regulate menstrual cycles, improve fertility, and promote overall reproductive health.
Scientific Support for Mud Therapy
While the traditional belief in mud therapy’s effectiveness is rooted in naturopathy, recent research has also supported its use for relaxation and stress management. Studies have demonstrated that mud therapy can lead to a significant reduction in cortisol levels and an increase in subjective feelings of relaxation. This makes it a promising complementary treatment for managing the emotional and physical symptoms of PCOS.
The Role of Yoga, Exercise, and Lifestyle Management in Treating PCOS and PCOD
Managing Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD) requires a comprehensive approach that includes lifestyle modifications, dietary adjustments, and targeted therapies. Among the most effective treatments are yoga, exercise, and stress management, all of which can help balance hormonal levels, improve metabolic health, and alleviate common symptoms like irregular menstruation, weight gain, and stress.
Yoga and Exercise for PCOS and PCOD
Physical activity is essential for both PCOS and PCOD patients, as it promotes overall health, helps regulate insulin levels, and supports hormonal balance. Certain exercises, particularly those with moderate intensity, are highly beneficial in managing these conditions.
- Yoga: Yoga is an excellent way to manage PCOS and PCOD, as it combines physical movement with relaxation techniques that help reduce stress and improve circulation. Specific poses, such as supta Buddha konasana (reclining bound angle pose), sarvangasana (shoulder stand), and paschimottanasana (seated forward bend), have been shown to have positive effects on hormonal health and menstrual cycles.
- Moderate-Intensity Exercises: Moderate-intensity exercises such as walking, swimming, and strength training are effective in improving insulin sensitivity and blood circulation, both of which are important for managing PCOS. Regular physical activity also aids in weight management, which is crucial for those with PCOS, as excess body weight can exacerbate symptoms.
Stress Management Techniques
Stress is a major contributing factor to hormonal imbalances in both PCOS and PCOD. When under stress, the body releases cortisol, a hormone that can further disrupt the endocrine system, leading to an increase in androgens and other hormonal imbalances.
- Meditation:
Meditation, particularly techniques such as mindfulness meditation, can be highly effective in lowering stress levels. Regular meditation practice helps calm the mind, reduce anxiety, and regulate emotional responses, all of which contribute to better hormonal health. - Breathing Exercises:
Pranayama and other breathing exercises, such as diaphragmatic breathing and sectional breathing, are also helpful for managing stress. These techniques help activate the parasympathetic nervous system, which promotes relaxation and helps to lower cortisol levels, thereby improving hormonal balance. - Mantras and Chanting:
Engaging in practices like mantra chanting and meditative vibrations can also support hormonal health. The rhythmic vibrations from chanting have been shown to calm the nervous system, reduce stress, and potentially lower cortisol levels. These practices not only help balance the body but also promote mental peace.
The Importance of Adequate Sleep
One of the most significant challenges for PCOS and PCOD patients is the disruption of sleep patterns. Many individuals with PCOS experience disturbed sleep, which can worsen symptoms and make the condition harder to manage. This disruption is often linked to an imbalance in the circadian rhythm, which affects the body’s internal clock and hormone production.
- Circadian Rhythm and Hormonal Secretion:
The circadian rhythm is closely tied to the secretion of hormones such as melatonin, which regulates sleep, and cortisol, which controls stress. Any disturbance in this rhythm, whether from irregular sleep habits or high stress levels, can disrupt the sleep-wake cycle and further affect hormonal balance. For PCOS and PCOD patients, this can lead to issues such as insulin resistance, weight gain, and menstrual irregularities. - Sleep Hygiene:
Establishing good sleep hygiene practices is crucial for PCOS and PCOD patients. This includes maintaining a consistent sleep schedule, reducing screen time before bed, and creating a restful environment. Adequate sleep is essential for balancing hormones and improving overall health.
Lifestyle and Relaxation Techniques for Managing PCOS and PCOD
When it comes to managing Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD), incorporating lifestyle changes, relaxation techniques, and proper self-care is essential for improving overall well-being and alleviating symptoms. While medical interventions play a crucial role in managing these conditions, lifestyle modifications can often make a significant difference in symptom management and overall quality of life.
Relaxation Techniques and Stress Management
Stress is a significant contributing factor to hormonal imbalances in PCOS and PCOD. Chronic stress can lead to the release of the stress hormone cortisol, which can worsen symptoms like weight gain, irregular menstruation, and emotional disturbances.
- Reducing Exposure to Stress:
It is important to reduce exposure to stressors, whether they are work-related stress, personal challenges, or other external pressures. Managing stress is crucial for maintaining a balanced hormonal environment and improving the body’s ability to regulate insulin and cortisol levels. - Relaxation Techniques:
Incorporating relaxation techniques like deep breathing, meditation, and yoga can be incredibly helpful in reducing stress. These practices promote calmness, mental clarity, and physical relaxation, which are all beneficial in managing the symptoms of PCOS and PCOD.
Detoxification and Hydration
A well-hydrated body is essential for proper metabolic function and hormonal regulation. Ensuring adequate hydration can help flush out toxins and support the body’s natural detoxification processes.
- Hydration:
Proper hydration is key to maintaining healthy internal cells and ensuring proper circulation. Drinking adequate amounts of water throughout the day can help with digestion, detoxification, and overall well-being. Additionally, hydration supports cellular function, which is essential for balancing hormones and reducing inflammation in the body. - Herbal Detox Drinks:
Herbal detox drinks made from natural herbs can further enhance the body’s detoxification process. Certain herbs like ginger, turmeric, cinnamon, and mint can promote digestion, reduce inflammation, and support liver function, which is essential for hormone balance. Consuming these drinks regularly can provide additional support to those managing PCOS or PCOD.
Lifestyle Changes for PCOS and PCOD
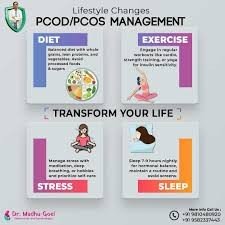
- Routine and Adequate Sleep:
PCOS and PCOD patients often experience disturbed sleep patterns due to hormonal imbalances. Establishing a regular sleep routine and ensuring adequate rest is critical for maintaining hormonal health. Circadian rhythm disruptions can affect hormonal secretion, particularly melatonin and cortisol, so it is essential to prioritize sleep for overall health. - Avoiding Environmental Toxins:
Environmental toxins, including plastics, chemicals, and heavy metals like lead, can contribute to hormonal disruptions. Limiting exposure to these toxins by using natural products, avoiding processed food packaging, and reducing the use of plastic containers can help reduce the toxic load on the body and support hormonal health. Dietary Management for PCOS and PCODThe role of diet is pivotal in managing PCOS and PCOD. While the dietary approach is largely similar for both conditions, there are some differences in the severity and focus of the dietary interventions.
Dietary Management for PCOS and PCODThe role of diet is pivotal in managing PCOS and PCOD. While the dietary approach is largely similar for both conditions, there are some differences in the severity and focus of the dietary interventions.
- For PCOS:
Dietary adjustments, such as increasing fiber intake, consuming healthy fats, and reducing refined sugar and processed foods, are essential. A low-glycemic diet that supports insulin sensitivity can help manage symptoms like weight gain, insulin resistance, and hormonal imbalances. - For PCOD:
In PCOD, lifestyle changes alone, including dietary management and the elimination of processed foods, may be sufficient to reverse symptoms in many cases. However, patients with PCOS may require more extensive dietary modifications and medical interventions, including medication and regular monitoring of blood sugar levels and hormonal health.
Key Lifestyle Changes for Both PCOS and PCOD
- Balanced Diet:
A balanced diet that includes whole foods, high fiber intake, lean proteins, and healthy fats is crucial. Nuts, seeds, avocados, fruits, and vegetables should be included, while sugary foods, processed snacks, and refined grains should be minimized to avoid triggering hormonal imbalances. - Exercise and Physical Activity:
Regular physical activity, such as walking, swimming, or strength training, is beneficial for both PCOS and PCOD patients. Exercise improves insulin sensitivity, supports weight management, and promotes overall hormonal health. - Stress Management and Relaxation:
Incorporating stress reduction techniques, such as meditation, pranayama (breathing exercises), and mindfulness, can help alleviate emotional and physical symptoms related to both PCOS and PCOD. - Herbal Remedies:
Herbal treatments, such as spearmint tea, ginger, and turmeric, have been shown to help with hormonal balance, insulin resistance, and inflammation. Incorporating these into a daily routine can provide additional support to the body.
Dietary Management and Hydrotherapy in PCOS and PCOD
When managing Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD), dietary modifications play a crucial role. However, the dietary approaches for both conditions are quite similar, with only slight adjustments necessary, particularly if metabolic components like insulin resistance are involved.
Dietary Management for PCOS and PCOD
The core principles of dietary management for PCOS and PCOD remain largely the same, focusing on a balanced, anti-inflammatory, and hormone-supportive diet. While some slight modifications might be needed for metabolic issues like insulin resistance or diabetes, in general, both conditions benefit from the following dietary guidelines:
- Focus on Whole Foods:
A diet rich in whole grains, vegetables, lean proteins, and healthy fats is vital. Foods high in fiber, such as fruits, vegetables, legumes, and whole grains, help improve insulin sensitivity and balance hormones. - Healthy Fats:
Including healthy fats in the diet—such as those from avocados, olive oil, nuts, and seeds—helps reduce inflammation and supports hormone regulation. - Reduced Refined Sugar:
Reducing the intake of refined sugars and processed foods can help regulate insulin levels and manage weight, which is often a concern for women with PCOS and PCOD. - High-Quality Proteins:
Protein sources like chicken, fish, eggs, and plant-based proteins such as lentils and beans should be prioritized for their role in balancing blood sugar and supporting metabolic function. - Gluten-Free Diet (If Inflammation is Present):
Gluten, found in wheat and other grains, can be an inflammatory nutrient for some individuals. If there is significant inflammation present, it’s recommended to avoid gluten for a period, typically around three months, to assess its impact on symptoms. However, this elimination should be done under the guidance of a healthcare provider to ensure balanced nutrition.
Hydrotherapy Treatments for PCOS and PCOD
Hydrotherapy can be a beneficial complementary treatment for PCOS and PCOD, helping to reduce symptoms, improve circulation, and manage stress. One of the most effective hydrotherapy treatments is the Tonic Sit Bath.
Tonic Sit Bath:
The Tonic Sit Bath is designed to target the pelvic area and lower abdomen, improving blood circulation, relieving tension, and promoting hormonal balance. Here’s how it works:
- Hot Foot Bath:
The patient should immerse their legs in a hot foot bath. This stimulates blood flow and promotes relaxation. - Cold Sit Bath:
Simultaneously, the patient should sit in a cold sit bath. This involves immersing only the pelvic area in cold water. The contrast of hot and cold helps to improve circulation, reduce inflammation, and enhance the overall therapeutic effect. - Wet Pack on the Head:
While in the sit bath, it’s recommended to place a wet pack on the head (which can be either warm or cold), adding an additional level of relaxation and stimulation to the body. - Massage:
During the sit bath, gently rub the hips, abdomen, and thighs for 1-3 minutes to further enhance the therapeutic effects. This massage improves lymphatic drainage and supports the pelvic organs. - Duration and Temperature:
The entire session typically lasts 15-20 minutes, with the foot bath being hot (around 55-65°C) and the sit bath being cold.
The Tonic Sit Bath is particularly useful for those experiencing irregular menstruation, pelvic discomfort, or hormonal imbalances related to PCOS and PCOD.
Tonic Sit Bath: A Hydrotherapy Treatment for PCOS and PCOD
The Tonic Sit Bath is a specialized hydrotherapy treatment that can be particularly effective in managing conditions like Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD). This treatment involves a combination of hot and cold water immersion along with gentle massage to stimulate the pelvic area and improve hormonal balance.
How to Perform the Tonic Sit Bath
The Tonic Sit Bath is designed to target the pelvic region, which is key for hormonal health. The procedure includes four main components:
- Hot Foot Bath:
The first step involves immersing the legs in a hot foot bath. This can be done in a bucket of hot water, which promotes blood circulation in the lower limbs and helps relax the body. - Wet Cloth Over the Head:
While soaking the feet in hot water, place a wet cloth over the head. The wet cloth can either be cool or warm, depending on the desired therapeutic effect. This helps in maintaining the body’s overall temperature balance during the treatment. - Cold Sit Bath:
While the feet are immersed in hot water, the pelvic region (from the navel down to the lower abdomen) is immersed in cold water. This is where the main therapeutic effect takes place. The sit bath focuses specifically on the pelvic area—unlike a regular hip bath, which covers the entire lower abdomen. The cold water immersion helps reduce inflammation and improve blood flow to the pelvic organs. - Massage:
During the sit bath, the patient should gently rub their abdomen, thighs, hips, and lower back. This can be done for about 1 to 3 minutes, or continuously throughout the bath. This massage stimulates blood circulation and enhances the effectiveness of the treatment.
Benefits of the Tonic Sit Bath for PCOS and PCOD
The Tonic Sit Bath has multiple benefits for women suffering from PCOS and PCOD. These conditions are often characterized by hormonal imbalances, and the tonic sit bath targets the reflex areas associated with hormone secretion.
- Hormonal Balance: The cold and hot water contrast in the sit bath helps stimulate hormonal secretions and can aid in regulating the endocrine system.
- Improved Circulation: The treatment helps improve blood flow to the pelvic area, which is essential for reproductive health.
- Stress Reduction: The therapy also works to relieve stress by promoting relaxation through the combination of heat, cold, and massage.
Duration and Frequency of the Tonic Sit Bath
- Duration: Each session should last around 10 minutes.
- Frequency: The tonic sit bath should be administered continuously for 7 to 10 days for maximum effectiveness. It is not recommended to do it just once a week or intermittently. For optimal results, this treatment should be done daily over the course of one to two weeks.
Understanding the Anti-Androgenic Effect and Dietary Management for PCOS
In the context of Polycystic Ovary Syndrome (PCOS), one of the key issues that many women face is the increase in androgen levels, which are typically male sex hormones. These elevated androgen levels can lead to symptoms such as excessive facial hair (hirsutism), acne, and scalp thinning.
Anti-Androgenic Effect
The term anti-androgenic effect refers to the ability of certain treatments or substances to reduce the levels of androgens (male hormones) in the body. In women with PCOS, elevated androgen levels are one of the primary hormonal imbalances, and reducing them can help manage the symptoms of the condition.
The anti-androgenic effect works by decreasing the production of androgens, effectively lowering the amount of male hormones in the female body. This can help alleviate symptoms like acne, hair thinning, and excessive hair growth, all of which are commonly seen in women with PCOS. Some treatments, such as medications or specific therapies, can be used to block androgen receptors or inhibit the production of androgens, leading to a reduction in their effects on the body.
Dietary Management for PCOS and Insulin Resistance
Dietary management is an important part of managing PCOS, especially when insulin resistance is a concern. Insulin resistance is a common issue in women with PCOS, and it can lead to metabolic syndrome and other health problems like fatty liver.
One of the key aspects of dietary management for PCOS is the control of sugar intake, particularly foods that contain certain sugars like malt dextrin or high-glycemic index sugars. Foods that are high in sugar or those containing alcoholic sugars can lead to an increase in fatty liver—a condition where fat accumulates in the liver, often leading to complications like fatty liver disease.
In women with insulin resistance, giving foods that are high in sugar can exacerbate the metabolic syndrome, leading to further complications. Therefore, avoiding high-sugar foods, especially refined sugars, is important. Instead, a low-glycemic diet with plenty of whole foods and fiber is recommended. Foods that are rich in fiber, low in refined sugars, and have a low glycemic index can help control insulin levels and improve the metabolic profile in women with PCOS.
The Role of Myo-Inositol in Dietary Management
Myo-Inositol is an essential part of the dietary approach for women with PCOS. It has been shown to improve insulin sensitivity and reduce the risk of fatty liver by promoting better metabolic functioning. Foods rich in myo-inositol, such as citrus fruits, blueberries, whole grains, nuts, and legumes, should be incorporated into the diet. These foods help manage insulin resistance and provide additional health benefits such as fiber, which is often lacking in the diets of women with PCOS.
Holistic Treatment Approach for PCOS and Insulin Resistance
When it comes to treating Polycystic Ovary Syndrome (PCOS), a holistic approach is essential. It is not just about focusing on one specific treatment but rather addressing the whole body and lifestyle of the patient. Along with dietary management, the holistic approach incorporates various therapeutic strategies such as weight management, detoxification, and cleansing to improve the overall health of the patient.
Holistic Approach to PCOS Treatment
A holistic treatment approach means looking at the patient’s physical, emotional, and mental well-being. It involves not just medication but also lifestyle changes and natural therapies. Key elements in a holistic approach to PCOS treatment include:
- Dietary Management: A balanced and nutrient-rich diet is critical in managing PCOS. This includes focusing on whole, nutrient-dense foods that regulate hormone levels and address underlying metabolic conditions like insulin resistance.
- Weight Management: Since many women with PCOS struggle with weight gain or difficulty losing weight, managing weight through healthy eating and exercise is a key part of the treatment. Weight loss can improve insulin sensitivity and help regulate hormones.
- Detoxification: Detoxification is another important aspect of the holistic treatment approach. By helping the body cleanse itself, detoxification aids in the proper functioning of internal organs and reduces the buildup of toxins that could be hindering overall health.
Detoxification Methods for PCOS
Detoxification in a holistic treatment approach may involve various techniques designed to cleanse the body and support the organs. Some common detoxification practices include:
- Ghee and Herbal Detox: Consuming ghee and herbal teas, which help in flushing out toxins and improving digestion. These can be included in the diet for better internal cleansing.
- Enemas: A procedure like colonic irrigation or enemas can be used to cleanse the digestive tract, promoting the removal of toxins and improving digestion. This is particularly beneficial for patients who suffer from constipation or sluggish digestion.
- Internal Organ Cleansing: Cleansing and detoxifying the liver, kidneys, and other organs are part of the detox process. This is done through specific herbs and practices that support the body’s natural detoxification processes.
Managing Insulin Resistance in PCOS
A common issue in PCOS is insulin resistance, where the body’s cells become less responsive to insulin. This leads to elevated insulin levels and can worsen hormonal imbalances. While naturopathic therapies and detoxification techniques can support overall health, it’s important to recognize that they cannot directly reduce insulin resistance.
Naturopathy focuses on providing supportive treatments that can help mitigate some of the symptoms of insulin resistance. However, insulin resistance itself requires medical intervention, including medication, lifestyle changes, and possibly dietary modifications, to improve insulin sensitivity.
Holistic and Medical Approach for Insulin Resistance in PCOS
When it comes to managing Polycystic Ovary Syndrome (PCOS), especially in cases where insulin resistance is present, a combined approach of both medical intervention and holistic treatment is essential. The focus should be on improving the patient’s overall lifestyle while providing appropriate medical treatments to manage insulin resistance effectively.
Medical Intervention in PCOS with Insulin Resistance
Insulin resistance is a hallmark of many PCOS cases, where the body’s cells do not respond effectively to insulin, leading to higher insulin levels and subsequent hormonal imbalances. While naturopathy and lifestyle modifications can significantly support overall health, they are not a cure for insulin resistance.
Medical interventions are necessary in this case, as they focus on improving insulin sensitivity and controlling blood sugar levels. This can include:
- Medications: Such as metformin, which is commonly prescribed to help manage insulin resistance and regulate blood sugar levels.
- Hormonal therapies: In cases where hormonal imbalances are present, medications to regulate hormones such as estrogen and testosterone may also be prescribed.
The key takeaway is that insulin resistance is a chronic condition that requires long-term management. It is not something that can be reversed overnight, and it is essential to address the root causes over an extended period of time with both medical and lifestyle modifications.
Holistic Approach to Managing Insulin Resistance
While medical interventions are critical, a holistic approach can significantly enhance the management of PCOS symptoms, especially in addressing the underlying causes of insulin resistance. Here are some key components of the holistic approach:
- Low Glycemic Index (GI) Diet: For patients with insulin resistance, the focus should be on a low-glycemic diet. Foods with a low glycemic index help regulate blood sugar levels and improve insulin sensitivity. This includes whole grains, legumes, lean proteins, and non-starchy vegetables, while high-sugar and high-fat foods should be avoided.
- Weight Management: Weight management is a critical component in managing insulin resistance. Excess body fat, especially around the abdominal area, can worsen insulin resistance. A healthy diet, combined with regular physical activity, can help manage weight and improve insulin sensitivity.
- Regular Exercise: Physical activity plays a vital role in improving insulin sensitivity. Moderate-intensity exercises like walking, swimming, and strength training can be beneficial for PCOS patients. Exercise helps reduce insulin resistance by improving glucose uptake in the muscles and enhancing overall metabolism.
- Stress Management: Chronic stress can exacerbate insulin resistance and worsen hormonal imbalances in PCOS. Relaxation techniques, such as meditation, deep breathing exercises, and yoga, can help reduce stress levels and support hormonal balance.
Importance of Lifestyle Modifications in Holistic Treatment
In addition to medical treatments, lifestyle modifications are a key part of managing insulin resistance in PCOS. A comprehensive approach includes:
- Adequate Sleep: Quality sleep is essential for maintaining proper hormonal function. Insulin resistance is often worsened by irregular sleep patterns and poor sleep quality, which disrupts the circadian rhythm.
- Detoxification: Incorporating detox practices, such as drinking herbal teas and staying hydrated, helps support the body’s natural cleansing processes and improve overall metabolic function.
- Avoiding Inflammatory Foods: In patients with insulin resistance, it is crucial to avoid inflammatory foods that could worsen insulin sensitivity. Highly processed foods, refined carbohydrates, and foods high in saturated fats should be limited.
The Long-Term Commitment to Managing Insulin Resistance
It’s important to understand that insulin resistance is a long-term condition that requires a sustained effort for improvement. It is not something that can be quickly reversed or treated with just one intervention. A combination of medical treatment and holistic practices over an extended period will help manage the symptoms of insulin resistance and reduce its impact on the patient’s overall health.
Understanding the Connection between Insulin Resistance and PCOS/PCOD
In the management of Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD), it is essential to understand the significant role that insulin resistance plays in these conditions. While every patient’s experience may differ based on their individual circumstances, a holistic approach, in conjunction with medical intervention, is crucial in addressing insulin resistance, which is often at the heart of both PCOS and PCOD.
Insulin Resistance in PCOS/PCOD
Insulin resistance is a condition where the body’s cells fail to respond properly to insulin, a hormone that helps regulate blood sugar levels. In PCOS and PCOD, this resistance can lead to higher insulin levels, which, in turn, can cause an imbalance in hormone levels and disrupt the normal functioning of the ovaries.
The primary cause of PCOS and PCOD in many cases is insulin resistance. This condition results in elevated insulin levels that trigger the ovaries to produce more androgens (male hormones), leading to symptoms such as irregular periods, excess hair growth, and ovarian cysts.
Holistic and Medical Approach to Managing Insulin Resistance
In treating insulin resistance associated with PCOS and PCOD, a holistic approach that includes both lifestyle modifications and medical intervention is vital for managing the condition effectively. Here are key strategies:
- Fasting and Meal Timing: One of the most effective ways to combat insulin resistance is through intermittent fasting. By limiting food intake to a restricted time frame (e.g., eating only three meals a day), the body is given a break from constant insulin production. This helps improve insulin sensitivity. Reducing munching or snacking throughout the day also plays a role in decreasing insulin resistance.
- Sleep and Rest: Adequate sleep is crucial for managing insulin resistance. Poor sleep can negatively impact insulin sensitivity. For optimal results, patients should aim for 7-9 hours of restful sleep each night. This helps maintain proper hormonal balance and supports insulin function.
- Dietary Modifications: Along with intermittent fasting, patients should follow a low-glycemic index diet, focusing on whole grains, lean proteins, and non-starchy vegetables. Avoiding processed foods, sugars, and high-glycemic foods is essential for maintaining balanced insulin levels.
- Medical Intervention: While lifestyle changes play a critical role, medical treatment is necessary for managing insulin resistance. Medications like metformin can help improve insulin sensitivity and regulate blood sugar levels. For patients with significant hormonal imbalances, medications to address hormonal regulation may also be required.
The Main Cause of Insulin Resistance in PCOS/PCOD
The primary cause of insulin resistance in PCOS and PCOD is thought to be related to genetic factors and hormonal imbalances. Elevated insulin levels contribute to higher androgen production in the ovaries, which disrupts the menstrual cycle and leads to the formation of cysts.
However, insulin resistance itself may be exacerbated by other lifestyle factors such as poor diet, lack of exercise, stress, and sleep disturbances. These factors contribute to the underlying metabolic dysfunction, making it essential to address both the physical and lifestyle components of treatment.
Understanding Insulin Resistance: Causes, Treatment, and Management
Insulin resistance is a condition in which the body’s cells become less responsive to the hormone insulin, leading to higher levels of insulin in the bloodstream. This condition plays a significant role in the development of Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD), but its impact extends beyond these conditions. In this article, we will explore the causes, treatment options, and management strategies for insulin resistance, shedding light on the factors that contribute to it and how to address it effectively.
What is Insulin Resistance?
Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels by allowing glucose (sugar) to enter the cells of the body to be used for energy. In insulin resistance, the body’s cells do not respond well to insulin. As a result, the pancreas produces more insulin to compensate for the body’s inability to use it effectively. Over time, this can lead to higher levels of insulin in the blood, which may cause various health issues, including weight gain, fatigue, and increased risk for developing conditions like diabetes, cardiovascular disease, and hormonal imbalances such as PCOS and PCOD.
Causes of Insulin Resistance
Insulin resistance can occur due to several factors, many of which are intertwined. These include:
- Genetic Factors: A family history of insulin resistance, type 2 diabetes, or other metabolic disorders can increase the risk of developing insulin resistance. Some individuals may be genetically predisposed to this condition.
- Lifestyle Factors: Poor dietary habits, lack of physical activity, stress, and insufficient sleep are significant contributors to insulin resistance. A diet high in processed foods, sugary beverages, and refined carbohydrates can contribute to this condition. Similarly, sedentary behavior and high levels of stress can exacerbate insulin resistance.
- Obesity: Excess body fat, particularly abdominal fat, can make the body less responsive to insulin, leading to insulin resistance. Individuals who are overweight or obese are at a higher risk of developing this condition.
- Hormonal Imbalances: Conditions like PCOS and PCOD are directly linked to insulin resistance, as elevated insulin levels can increase androgen production in the ovaries, leading to further hormonal imbalances and metabolic dysfunction.
- Age and Gender: Insulin resistance can become more common as individuals age, especially in women during menopause. Hormonal changes during this period can also contribute to the development of insulin resistance.
How to Treat Insulin Resistance
While insulin resistance is a chronic condition that requires ongoing management, there are several effective ways to treat and reverse it. A holistic approach that includes both lifestyle changes and medical interventions is often the most effective strategy.
- Dietary Modifications:
- Low Glycemic Index (GI) Foods: Eating foods that have a low glycemic index can help control blood sugar levels and improve insulin sensitivity. These foods include whole grains, vegetables, lean proteins, and fruits.
- Avoiding Processed and Sugary Foods: Reducing the intake of refined sugars, processed snacks, and high-calorie foods can help prevent insulin spikes and support the body’s ability to manage blood sugar effectively.
- Gluten-Free Diet: While not everyone may need to avoid gluten, for some individuals, especially those with inflammation, cutting out gluten can help reduce insulin resistance. However, for individuals with genetic predispositions that make gluten a staple in their diet (such as certain cultural groups), gluten should not be universally avoided.
- Exercise: Regular physical activity helps improve insulin sensitivity by promoting better glucose uptake by the muscles. Both strength training and aerobic exercises such as walking, swimming, and cycling are beneficial for individuals with insulin resistance.
- Intermittent Fasting: Fasting for certain periods has been shown to help reduce insulin levels and improve insulin sensitivity. Both long fasting methods and eating smaller, more frequent meals have been tested and found effective for managing insulin resistance.
- Stress Management: Chronic stress can exacerbate insulin resistance, so it’s important to incorporate stress-reducing techniques into daily life. Practices such as meditation, deep breathing, yoga, and other relaxation methods can help lower stress hormones like cortisol, which in turn helps improve insulin sensitivity.
- Adequate Sleep: Lack of sleep is a major contributing factor to insulin resistance. Ensuring 7-9 hours of restful sleep per night helps regulate hormones and improve overall metabolic function.
- Medical Intervention: In some cases, medications may be necessary to manage insulin resistance. Metformin, a drug commonly prescribed to individuals with type 2 diabetes, can help improve insulin sensitivity and regulate blood sugar levels. For individuals with PCOS, medical treatments may also be required to manage hormonal imbalances.
Key Takeaways
- Insulin resistance is a condition in which the body’s cells become less responsive to insulin, leading to higher blood insulin levels. It is a key factor in the development of PCOS and PCOD.
- The causes of insulin resistance are genetic, lifestyle-related, and influenced by obesity, hormonal imbalances, and stress.
- Dietary changes, regular physical activity, stress management, and adequate sleep are essential in treating and managing insulin resistance.
- Medical intervention, such as the use of metformin and other medications, may be necessary for individuals with more severe insulin resistance.
Understanding Insulin Resistance: Causes, Management, and Prevention
Insulin resistance is a condition where the body’s cells, particularly in the muscles, fat, and liver, do not respond properly to the hormone insulin. As a result, glucose (sugar) cannot enter these cells effectively. To compensate, the pancreas produces more insulin to help push the glucose into the cells. Over time, this increased insulin production can lead to several health issues, including fatty liver disease, type 2 diabetes, and metabolic disorders like PCOS (Polycystic Ovary Syndrome) and PCOD (Polycystic Ovary Disease).
While insulin resistance is often associated with the development of diabetes, it is not a disease in itself but rather a lifestyle disorder. It arises due to poor lifestyle choices, such as unhealthy eating habits, lack of physical activity, stress, and other environmental factors. However, with proper lifestyle modifications, insulin resistance can be effectively managed, and its impact minimized.
In cases where insulin resistance is not addressed, it can eventually lead to type 2 diabetes. Additionally, PCOS and PCOD patients often experience insulin resistance, which contributes to the hormonal imbalances they face.
The Impact of Insulin Resistance on Health
When the body becomes resistant to insulin, the glucose that is not absorbed by the cells remains in the bloodstream, leading to higher blood sugar levels. Over time, this can cause a variety of health issues:
- Fatty Liver Disease: As glucose cannot be utilized for energy, it is stored as fat in the liver, leading to non-alcoholic fatty liver disease (NAFLD).
- Type 2 Diabetes: If left unmanaged, insulin resistance can eventually progress to type 2 diabetes, where blood sugar levels become dangerously high due to the body’s inability to use insulin effectively.
- PCOS and PCOD: Insulin resistance plays a significant role in PCOS and PCOD, contributing to hormonal imbalances, which may lead to irregular menstrual cycles, infertility, and excess hair growth.
- Hypertension: Insulin resistance is often associated with higher blood pressure, contributing to hypertension.
How to Manage and Prevent Insulin Resistance
Insulin resistance is a lifestyle disorder, not a disease, and can be managed through a combination of healthy lifestyle changes. With the right approach, insulin resistance can be reversed or its effects minimized.
- Dietary Modifications:
- Low Glycemic Index (GI) Foods: Consuming foods with a low glycemic index, such as whole grains, vegetables, lean proteins, and fruits, can help regulate blood sugar levels.
- Avoid Sugary and Processed Foods: Reducing the intake of refined carbohydrates, sugary drinks, and processed snacks is crucial in preventing blood sugar spikes.
- Healthy Fats and Protein: Including healthy fats (e.g., olive oil, nuts, and seeds) and lean proteins in the diet can help stabilize blood sugar and improve insulin sensitivity.
- Exercise: Regular physical activity, including aerobic exercises like walking or swimming and strength training, helps improve insulin sensitivity and aids in the absorption of glucose into cells.
- Stress Management: Practices like yoga, meditation, and deep breathing exercises can help manage stress and reduce cortisol levels, which improve insulin function.
- Adequate Sleep: Ensuring sufficient sleep (7-9 hours per night) is crucial for maintaining hormonal balance and managing insulin sensitivity.
- Fasting: Intermittent fasting or regular fasting periods can improve insulin sensitivity by reducing insulin production and giving the body time to process glucose.
- Medical Intervention: In some cases, medications like metformin can be prescribed to improve insulin sensitivity and help manage blood sugar levels.
Testing and Diagnosis of Insulin Resistance
Insulin resistance can often be detected through blood tests. Common tests to evaluate insulin resistance include:
- Fasting Insulin Test: Measures the level of insulin in the blood after an overnight fast. Higher insulin levels may indicate insulin resistance.
- HOMA-IR (Homeostasis Model Assessment of Insulin Resistance): This calculation is used to estimate insulin resistance by evaluating fasting blood glucose and insulin levels.
- Oral Glucose Tolerance Test (OGTT): This test measures the body’s ability to process glucose over a set period, typically after consuming a sugary solution.
For individuals as young as 15 or 16, insulin resistance tests can help predict the likelihood of developing diabetes later in life. Early detection and intervention can play a critical role in preventing or delaying the onset of diabetes.
Insulin Resistance Syndrome: Testing, Causes, and Its Connection to Lifestyle and Diseases
Insulin resistance is a key factor that contributes to many health conditions, including fatty liver disease, type 2 diabetes, PCOS (Polycystic Ovary Syndrome), PCOD (Polycystic Ovary Disease), and more. While the condition is often overlooked, understanding its impact is essential to preventing more severe diseases. Insulin resistance is not always immediately apparent, but it can significantly affect a person’s overall health, leading to a range of chronic conditions.
Insulin Resistance Syndrome Test
The Insulin Resistance Syndrome test is a common diagnostic tool used to determine whether someone is at risk of developing insulin resistance. This test can be done in different ways:
- Fasting Test: This test measures insulin and blood glucose levels after an overnight fast.
- Postprandial Test (Post-Meal Test): Measures insulin and glucose levels after eating.
- Random Test: Taken at any point during the day without regard to meals.
These tests help assess insulin levels and give an indication of whether someone is at risk of developing diabetes, fatty liver disease, or other related conditions. Even if a person is not diabetic today, they may have elevated insulin levels, which suggests they are on the path to developing insulin resistance.
The Connection between Insulin Resistance and Disease
Insulin resistance is often considered the starting point for many chronic conditions, and it all begins with the pancreas. The pancreas, which sits between the liver and the spleen, plays a central role in regulating insulin levels. When the pancreas doesn’t function properly, it can have a cascading effect on various organs in the body.
Here’s how insulin resistance connects to several health conditions:
- Fatty Liver Disease: Insulin resistance is a significant contributor to the development of fatty liver disease, a condition where excess fat builds up in the liver. When insulin is not functioning correctly, it leads to higher blood glucose levels, and the liver stores this excess glucose as fat.
- Type 2 Diabetes: Insulin resistance is a major precursor to type 2 diabetes. When the body’s cells can’t properly use insulin, the pancreas overcompensates by producing more insulin. Over time, this imbalance can lead to chronic high blood sugar levels, eventually resulting in diabetes.
- PCOS and PCOD: Polycystic Ovary Syndrome (PCOS) and Polycystic Ovary Disease (PCOD) are both linked to insulin resistance. Elevated insulin levels contribute to hormonal imbalances in women with PCOS and PCOD, leading to symptoms such as irregular periods, infertility, and excessive hair growth.
- Hypertension and Other Conditions: Insulin resistance is also associated with high blood pressure (hypertension) and other metabolic conditions, all of which are interconnected.
Lifestyle Factors Leading to Insulin Resistance
Insulin resistance is often caused by poor lifestyle choices, and addressing these can help prevent or manage the condition. Some of the major lifestyle factors include:
- Dietary Habits: Consuming high-glycemic foods, processed foods, and sugary snacks can contribute to insulin resistance. A diet high in refined carbohydrates and fats can impair the body’s ability to regulate insulin effectively.
- Lack of Exercise: Physical inactivity is a major risk factor for insulin resistance. Exercise helps increase insulin sensitivity, allowing the body to use glucose more efficiently.
- Stress: Chronic stress increases the production of cortisol, a hormone that can negatively affect insulin function. Managing stress through mindfulness techniques or physical activity can help mitigate this impact.
- Obesity: Excess fat, particularly around the abdomen, is a major risk factor for insulin resistance. Losing weight and maintaining a healthy weight can improve insulin sensitivity.
How Insulin Resistance Develops
While insulin resistance is primarily driven by lifestyle factors, it also has a genetic component. Some individuals may be genetically predisposed to insulin resistance, while others may develop it due to poor diet and lack of exercise.
In insulin resistance, the cells in the body—particularly in the liver, fat, and muscles—become less responsive to insulin. This means that the glucose in the bloodstream is not absorbed into the cells for energy. As a result, the pancreas continues to produce more insulin to try to force the glucose into the cells. Over time, this leads to higher levels of insulin and glucose in the blood, contributing to the development of various chronic diseases.
Managing Insulin Resistance
Insulin resistance is a lifestyle disorder that can be managed with proper interventions. These include:
- Dietary Changes: Focus on a balanced diet with low glycemic index foods that help regulate blood sugar levels. Avoid processed foods, sugary drinks, and refined carbohydrates.
- Regular Exercise: Physical activity, particularly strength training and aerobic exercise, can improve insulin sensitivity and help manage insulin resistance.
- Stress Management: Practice relaxation techniques like yoga, deep breathing, and meditation to lower stress levels and reduce cortisol production.
- Weight Management: Maintaining a healthy weight, particularly reducing abdominal fat, can improve insulin sensitivity and reduce the risk of developing diabetes and other conditions associated with insulin resistance.
- Medical Intervention: In some cases, medications like metformin can be prescribed to help improve insulin sensitivity and manage blood sugar levels.
The Importance of Early Detection
Early detection of insulin resistance can help prevent the development of more serious conditions, including diabetes and fatty liver disease. Individuals at risk of insulin resistance should undergo regular testing to monitor their insulin and blood glucose levels. Early intervention through lifestyle changes can significantly reduce the risk of developing chronic diseases.
Understanding Bulky Ovaries: Causes, Investigations, and Treatment

A bulky ovary is a condition where one or both ovaries appear enlarged, which can be a common concern for many women. The term “bulky” refers to the size of the ovary being larger than normal, but it does not necessarily indicate a serious issue. However, it is important to understand the potential causes and when medical investigation is necessary to ensure proper health management.
What Causes Bulky Ovaries?
A bulky ovary can result from various conditions, but it is not always a sign of a severe underlying problem. Some of the possible causes include:
- Ovarian Cysts: Fluid-filled sacs that can develop on or inside the ovaries. While often benign, some cysts can cause the ovaries to appear enlarged.
- Ovarian Fibroids: Though less common than cysts, fibroids (non-cancerous growths) in or around the ovaries can lead to enlargement.
- Hormonal Imbalance: An imbalance in hormones can cause the ovaries to grow larger than usual, particularly in conditions like Polycystic Ovary Syndrome (PCOS).
- Pregnancy: In some cases, pregnancy can cause temporary changes in the ovaries due to hormonal shifts.
- Other Conditions: Rarely, conditions like ovarian cancer or infections may also cause the ovaries to become bulky, but these cases are not as common.
Investigating Bulky Ovaries
If a woman notices that her ovaries appear bulky or experiences symptoms such as pelvic pain or changes in menstrual cycles, a thorough investigation is crucial. This typically involves:
- Ultrasound Examination: An ultrasound is the primary diagnostic tool used to determine the size and condition of the ovaries. It can help identify any cysts, fibroids, or other abnormalities that might be contributing to the enlargement.
- Blood Tests: Hormonal imbalances can also be checked through blood tests to see if they are contributing to the changes in the ovaries.
- Pelvic Exam: A physical pelvic examination may also be performed to check for any noticeable changes in the uterus, ovaries, or surrounding areas.
When Should You Be Concerned?
If no cysts, fibroids, or significant abnormalities are found, and the ovaries are simply enlarged without causing pain or other symptoms, it is generally not considered a serious condition. However, it’s important to monitor the situation, especially if other symptoms develop over time. In such cases, the condition may resolve on its own, and no specific treatment may be necessary.
Treatment for Bulky Ovaries
In most cases, if a bulky ovary is not accompanied by serious conditions like cysts or fibroids, it does not require immediate treatment. However, some general approaches to managing the condition may include:
- Hormonal Therapy: If hormonal imbalance is identified as a contributing factor, treatments such as birth control pills or hormone therapy may be recommended to regulate the menstrual cycle and reduce ovarian enlargement.
- Lifestyle Adjustments: Healthy lifestyle choices, such as maintaining a balanced diet, regular exercise, and stress management, can help support hormonal balance and reduce the likelihood of further ovarian issues.
- Regular Monitoring: If no immediate action is required, regular check-ups and monitoring through ultrasound or other diagnostic tests can ensure that the condition does not worsen or lead to other complications.

Overall Conclusion
The article highlights the complex interplay between lifestyle, hormonal imbalances, and conditions like PCOS (Polycystic Ovary Syndrome) and PCOD (Polycystic Ovary Disease). Both of these conditions are closely linked to insulin resistance, which plays a critical role in their development and progression. The main takeaway is that insulin resistance is not just a disease but a lifestyle disorder influenced by factors like diet, stress, and exercise habits.
Addressing insulin resistance and hormonal imbalances requires a holistic approach, combining medical interventions with lifestyle modifications, such as proper diet management, regular exercise, and stress reduction techniques like yoga and meditation. Dietary management includes focusing on low glycemic index foods, avoiding inflammatory foods, and ensuring proper hydration and detoxification. Holistic treatments like hydrotherapy (e.g., tonic sit baths) and mind-body practices further support this approach.
Additionally, managing insulin resistance involves addressing metabolic dysfunctions through intermittent fasting or smaller, more frequent meals, and prioritizing adequate sleep to support circadian rhythms and overall hormonal balance.
For conditions like bulky ovaries, the article emphasizes that, while it may not always indicate a serious condition, proper investigation (e.g., ultrasound) is necessary to rule out complications such as cysts or fibroids. In the absence of significant findings, bulky ovaries are generally not a cause for concern.
Ultimately, the article stresses that addressing conditions like PCOS and PCOD is not about quick fixes but requires ongoing management, regular monitoring, and a commitment to a healthy, balanced lifestyle. By integrating medical care with holistic practices, women can significantly improve their reproductive health and reduce the long-term risks associated with these conditions.
- For PCOS:
- PCOD (Polycystic Ovarian Disease):