The disease of Pancreas
The disease of Pancreas
Understanding Pancreatic Diseases: Importance, Function, and Impact 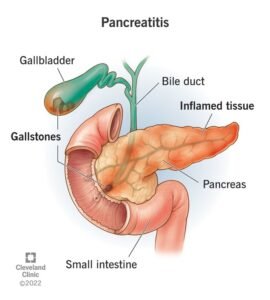
Introduction
Today, we are discussing a vital topic — diseases of the pancreas. The pancreas is one of the most unique and delicate organs in the human body. Its proper functioning is crucial to maintaining overall health. To understand pancreatic diseases better, it’s important to first understand what the pancreas is, how it works, and why it is so essential.
Anatomy and Function of the Pancreas
The pancreas is a glandular organ located in the abdomen, positioned behind the stomach. It plays a central role in both the digestive and endocrine systems of the body. As shown in the slides, the pancreas is connected with other organs and consists of three main parts: the head, body, and tail.
As a glandular organ, the pancreas has two major functions:
- Exocrine function: It produces digestive enzymes that help break down food in the small intestine.
- Endocrine function: It releases hormones like insulin and glucagon into the bloodstream to regulate blood sugar levels.
The Role of the Pancreas in Digestion
One of the most critical roles of the pancreas is aiding in digestion. The food we eat must be properly broken down and absorbed by our bodies to ensure good health. It’s not just about eating healthy food — what matters more is how well your body digests and absorbs that food.
This process depends heavily on the pancreas. The enzymes produced by the pancreas break down carbohydrates, proteins, and fats in the small intestine. Without these enzymes, food cannot be properly digested, and the nutrients won’t be absorbed into the body.
Pancreatic Insufficiency
A common disorder associated with the pancreas is pancreatic insufficiency. This condition occurs when the pancreas cannot produce enough digestive enzymes, leading to poor digestion and nutrient absorption. As a result, even if a person eats nutritious food, the body may still suffer from deficiencies.
Symptoms of pancreatic insufficiency may include:
- Bloating
- Diarrhea
- Weight loss
- Fatigue
- Malnutrition
This condition shows that digestion and absorption are more important than the quantity or quality of food alone. Without proper enzyme production, the body remains deprived of essential nutrients, leading to further health problems.
Structure and Location of the Pancreas
The pancreas, though small, plays a powerful role in maintaining health. A common misconception is that diseases occur only when toxins or “morbid matter” accumulate in the body. However, many of these imbalances happen when the body’s digestion and absorption processes are not functioning properly. This dysfunction can lead to the
accumulation of harmful substances and poor nutrient uptake, further compromising overall health.
Anatomical Divisions of the Pancreas
Anatomically, the pancreas is divided into three parts:
- Head – Located on the right side, this portion is nestled into the curve of the duodenum (the first part of the small intestine). It connects with several structures including:
- The accessory pancreatic duct
- Minor and major duodenal papillae
- The common bile duct
- Body – The central part of the pancreas that stretches across the abdomen. It lies behind the stomach and is in close proximity to several blood vessels.
- Tail – The tapered end of the pancreas, which lies near the spleen. This section is often the thinnest and is significant in endocrine function (hormone release).
In educational diagrams or slides, the pancreas is often shown in yellow, clearly labeled from bottom to top as the head, body, and tail, to aid understanding of its structure.
Size and Weight
Despite its critical role, the pancreas is quite small:
- Length: Approximately 6 inches
- Weight: Around 200 grams
It is located deep within the abdominal cavity, tucked behind the stomach. Its small size may give the impression of insignificance, but its function is vital. Interestingly, the size and weight of the pancreas remain consistent regardless of a person’s overall body weight or height. Whether someone weighs 50 kg or 100 kg, the pancreas generally retains its average dimensions and mass.
Connection to Other Organs
The pancreas is intricately connected to other organs through ducts and vessels. These include:
- The main pancreatic duct, which merges with the bile duct before emptying into the small intestine.
- The duodenal papilla, where pancreatic juices are released to aid digestion.
This complex network ensures that the pancreas can deliver digestive enzymes and hormones to the right place at the right time, maintaining the balance of the digestive and endocrine systems.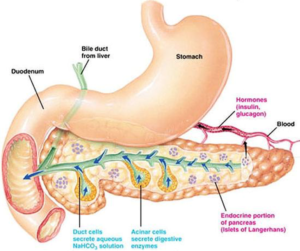
Enzyme and Hormone Transportation in the Pancreas
The pancreas is not just a vital organ—it is also a powerful biochemical factory. But how does it actually transport the essential substances it produces, like digestive enzymes and hormones? For this, nature—or as many believe, Mother Nature or God—has provided us with a highly intelligent design: two powerful ducts that ensure the proper functioning of the pancreas.
The Role of Pancreatic Ducts
The pancreas contains two main ducts that are crucial for transporting enzymes and hormones into the digestive system. These ducts are:
- Main Pancreatic Duct (Duct of Wirsung)
- Accessory Pancreatic Duct (Duct of Santorini)
These ducts connect the pancreas directly to the duodenum (the first part of the small intestine), allowing the flow of enzymes and hormones at the right time and place. Without these ducts, the pancreas—even if structurally intact—would not be able to perform its essential functions.Transporting Digestive Enzymes
Through these ducts, the pancreas sends powerful digestive enzymes into the duodenum. These enzymes help break down carbohydrates, proteins, and fats in the food we eat, allowing the body to absorb nutrients efficiently.
Transporting Insulin and Its Importance
One of the most essential hormones secreted by the pancreas is insulin. This hormone is vital for regulating blood sugar levels. When insulin production is inadequate or the body cannot use it properly, it results in diabetes mellitus—one of the most common lifestyle diseases today.
It is estimated that one in every five to seven people worldwide suffers from some form of diabetes, whether Type 1, Type 2, or other variants. This disease directly reflects how crucial the pancreas is in maintaining our internal balance. If the pancreas is not healthy, the risk of developing such lifestyle-related diseases increases significantly.
The Dual Functions of the Pancreas
The pancreas performs two major functions, both of which are essential for survival:
- Endocrine function – Secreting hormones like insulin and glucagon into the bloodstream to regulate blood sugar.
- Exocrine function – Producing and transporting digestive enzymes like amylase, lipase, and trypsin into the digestive tract.
If either of these systems fails, the entire body can be thrown off balance. Insulin and digestive enzymes are like technicians working behind the scenes to keep every process running smoothly.
Endocrine and Exocrine Functions of the Pancreas
The pancreas is a dual-function organ, meaning it plays a role in both hormone production (endocrine function) and digestive support (exocrine function). Understanding these two roles is essential to grasp how this organ helps regulate major processes in our body like digestion and blood sugar control.
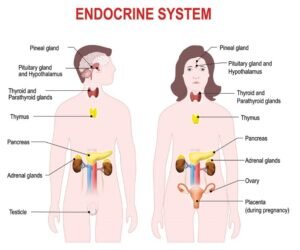 Endocrine Function
Endocrine FunctionThe endocrine function of the pancreas refers to the production and release of hormones that regulate blood sugar levels and various other body functions. These hormones are secreted directly into the bloodstream and are produced by specialized clusters of cells within the pancreas known as the islets of Langerhans.
Key hormones produced by the endocrine system of the pancreas include:
- Insulin – Regulates blood glucose by allowing cells to absorb sugar.
- Glucagon – Raises blood sugar levels when they drop too low.
- Amylin – Helps control blood sugar spikes after eating.
- C-peptide – A byproduct of insulin production, used as a marker to assess pancreatic function.
- Somatostatin – Regulates the secretion of other pancreatic hormones.
- Pancreatic polypeptide – Helps in regulating both pancreatic secretions and digestive functions.
These hormones are essential for maintaining metabolic balance. Without proper hormone secretion, the body cannot regulate blood sugar, leading to disorders like diabetes mellitus.
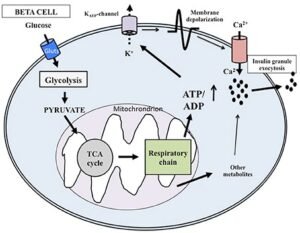
The Role of Beta Cells
Within the islets of Langerhans, beta cells are responsible for producing insulin. These cells are crucial for healthy pancreatic function. If beta cells are damaged, insulin production is affected, leading to impaired glucose regulation. The destruction or dysfunction of beta cells is a core issue in Type 1 and advanced Type 2 diabetes. Therefore, preserving beta cell health is a primary focus in diabetes prevention and management.
Exocrine Function
The exocrine function of the pancreas involves the production of digestive enzymes, which are secreted into the small intestine through pancreatic ducts. These enzymes help in breaking down carbohydrates, fats, and proteins from the food we eat, allowing the body to absorb nutrients effectively.
Key digestive enzymes include:
- Amylase – Breaks down carbohydrates.
- Lipase – Breaks down fats.
- Proteases (like trypsin and chymotrypsin) – Break down proteins.
This function is essential for proper digestion and absorption. Without pancreatic juice and its enzymes, the food we consume would not be broken down adequately, resulting in malnutrition and digestive problems.
Common Diseases of the Pancreas
After understanding the vital functions of the pancreas—both endocrine and exocrine—it’s important to also learn about the diseases that can affect this delicate organ. Pancreatic diseases can have serious consequences because of the pancreas’s key role in digestion and blood sugar regulation.
The Pancreas in Mammals and Humans
The pancreas is present in all mammals, including humans, and is located deep within the abdominal cavity. Whether it’s humans, animals that walk, breathe, or move—almost all living mammals are naturally equipped with a pancreas. It’s a gift of Mother Nature, essential for survival. The pancreas performs two major roles:
- Digestive – by producing enzymes to break down food
- Endocrine – by producing hormones like insulin to regulate blood sugar levels
Any damage or disease in this organ can disturb either or both of these systems, affecting overall health and metabolism.
Major Pancreatic Diseases
Here are some of the most common pancreatic conditions that medical professionals and the general public should be aware of:
- Acute Pancreatitis
- A sudden inflammation of the pancreas.
- It can be caused by gallstones, heavy alcohol use, infections, or injury.
- Symptoms include severe abdominal pain, nausea, vomiting, and fever.
- It often requires hospitalization and close monitoring.
- Chronic Pancreatitis
- A long-term inflammation that gradually damages the pancreas.
- Often caused by repeated episodes of acute pancreatitis or long-term alcohol use.
- Leads to permanent damage and can cause diabetes or digestion problems.
- Pancreatic Cancer
- Less common but extremely serious.
- Difficult to detect in early stages due to non-specific symptoms.
- Risk factors include smoking, obesity, genetic factors, and chronic pancreatitis.
- Often requires surgery, chemotherapy, or both.
- Type 1 Diabetes Mellitus
- An autoimmune condition where the body’s immune system attacks the beta cells in the pancreas, stopping insulin production.
- Usually diagnosed in children or young adults.
- Patients require lifelong insulin therapy.
- Type 2 Diabetes Mellitus
- A condition where the body becomes resistant to insulin or the pancreas doesn’t produce enough of it.
- Often related to lifestyle factors like poor diet, lack of exercise, and obesity.
- Managed through diet, exercise, medication, and sometimes insulin.
- Gestational Diabetes
- Occurs during pregnancy.
- Can affect both the mother and the baby’s health if not managed properly.
- Usually resolves after childbirth but increases the risk of developing Type 2 diabetes later.
- Maturity Onset Diabetes of the Young (MODY)
- A rare form of diabetes caused by a genetic mutation.
- Often misdiagnosed as Type 1 or Type 2.
- Typically appears before age 25 and can sometimes be managed without insulin.These are just some of the many conditions that can affect the pancreas. Whether acute or chronic, each disease demands attention, proper diagnosis, and treatment. Understanding these conditions helps in early detection, better management, and improved quality of life.

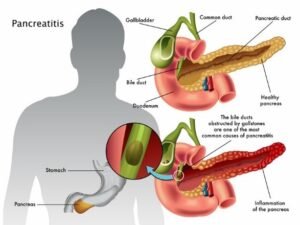
Understanding Pancreatitis: Acute vs Chronic
Among the various diseases that affect the pancreas, the most commonly seen and discussed condition is pancreatitis. It is an inflammatory disease of the pancreas, and it can be acute or chronic in nature. The two forms differ in terms of duration, severity, reversibility, and long-term impact on the pancreatic tissue.
What is Pancreatitis?
Pancreatitis occurs when the pancreas becomes inflamed, leading to swelling, pain, and dysfunction. It affects the pancreas’ ability to carry out both digestive and hormonal functions, and if left untreated, it can damage other organs as well.
Like diabetes, which is classified into Type 1 and Type 2, pancreatitis is also broadly categorized into two types:
- Acute Pancreatitis
- Chronic Pancreatitis
Let’s break down both forms:
- Acute Pancreatitis
Acute pancreatitis is a sudden inflammation of the pancreas that lasts for a short duration. It is often triggered by:
- Gallstones
- Heavy alcohol consumption
- Certain medications
- High levels of triglycerides
Key Features:
- Sudden onset of abdominal pain
- Swelling or edema of the pancreas
- Can involve necrosis (tissue death) and formation of pseudocysts (fluid-filled sacs)
- Nausea, vomiting, fever, and tenderness in the upper abdomen
Important Point:
The good news is that acute pancreatitis is often reversible—if diagnosed and treated early, most patients recover fully without permanent damage. Early detection, proper medical management, and lifestyle changes play a major role in recovery.- Chronic Pancreatitis
Chronic pancreatitis is a long-standing inflammation of the pancreas that does not heal or improve over time. It usually follows repeated episodes of acute pancreatitis or is linked to ongoing risk factors like alcohol abuse, autoimmune diseases, or genetic predisposition.
Key Features:
- Persistent abdominal pain
- Permanent damage to pancreatic tissue
- Progressive loss of pancreatic function
- Risk of diabetes and poor digestion due to enzyme deficiency
Unlike the acute form, chronic pancreatitis is not fully reversible. Once the pancreas is severely damaged, its ability to regenerate is very limited. However, alternative therapies, naturopathy, and herbal medicine may help manage symptoms, reduce flare-ups, and preserve whatever pancreatic function remains.
Prognosis and Early Diagnosis
Understanding the prognosis—the likely outcome of the disease—is key to deciding on a treatment plan. In the case of acute pancreatitis, early diagnosis greatly improves the chances of full recovery. Therefore, recognizing signs like:
- Persistent abdominal pain
- Digestive issues
- Fever or jaundice
…should prompt immediate medical evaluation.
In both forms of pancreatitis, swelling (edema) and inflammation are common early signs. Proper imaging (like ultrasound or CT scan) and lab tests (like serum amylase and lipase) are used to confirm the diagnosis.
Acute vs Chronic Pancreatitis: Recognizing the Symptoms and Listening to Your Body
Understanding the difference between acute and chronic pancreatitis is vital not only for early diagnosis but also for effective treatment and recovery. Our body is a brilliant system that often gives us signs when something isn’t right—and pancreatitis is no exception.
Acute Pancreatitis: A Sudden Alarm
Acute pancreatitis is characterized by a sudden inflammation of the pancreas. It doesn’t persist for long and usually appears out of nowhere, lasting for a short period. The key here is sudden onset—you may feel fine one day and experience severe abdominal pain the next.
Common Symptoms of Acute Pancreatitis:
- Sudden, sharp abdominal pain (usually in the upper abdomen)
- Nausea and vomiting
- Bloating
- Loss of appetite
- Difficulty eating or digesting food
These symptoms may last a few hours to a few days, and they often improve with proper treatment and rest. It is not a continuous or lingering condition—that’s what differentiates it from the chronic form.
The body alerts us with symptoms. When these early signs arise, we must not ignore them. If detected and treated early, acute pancreatitis is 100% reversible. The swelling (edema) and inflammation of the pancreas at this stage can often be managed quickly with the right medical care.
Chronic Pancreatitis: When We Ignore the Signals
Chronic pancreatitis is a long-term, progressive condition. It typically develops when acute pancreatitis is neglected or mismanaged. If the inflammation and damage are left untreated over weeks or months, it turns into a chronic issue that becomes more difficult to treat.
Chronic pancreatitis is not just a physical issue—it affects the patient mentally and emotionally as well. As the disease persists:
- The pancreatic tissue becomes damaged permanently.
- Beta cells in the pancreas begin to fail.
- Digestive and hormonal functions are compromised.
Unfortunately, unlike acute pancreatitis, chronic pancreatitis is not fully reversible. The pancreas cannot regenerate entirely—though alternative treatments and therapies may help preserve function, activate some pancreatic cells, or improve the quality of life.
The Importance of Early Attention
The human body is intelligent and intuitive. It constantly sends signals when something is off. Symptoms like:
- Digestive discomfort
- Appetite changes
- Ongoing fatigue
- Bloating or pain after meals…are often early indicators that something isn’t right. Listening to your body and acting on these signs early is crucial.
If you ignore these “internal alarms”, you risk allowing an easily manageable condition like acute pancreatitis to turn into a life-long issue that is harder to treat and manage.
Mind-Body Connection in Pancreatic Health
Interestingly, research and practice suggest that 95–97% of diseases are psychosomatic, meaning that the mind and emotions play a huge role in physical health. Only a small percentage—about 2–3%—are purely physical.
Pancreatic diseases, including pancreatitis, often have psychosomatic roots. Stress, emotional strain, poor mental health, and unresolved trauma can deeply impact our pancreas and digestive health. That’s why a holistic approach—addressing both the body and the mind—is essential for healing.
The Emotional Impact of Pancreatic Dysfunction: A Simple Example
Let’s look at this in very simple terms: imagine you are hungry, but every time you eat, your food doesn’t digest properly. You feel bloating, rawness in the stomach, and an ongoing sense of discomfort. Even after eating, you don’t feel satisfied. This ongoing digestive disturbance leads to a constant state of irritation, restlessness, and sometimes even emotional grief.
Over time, this continuous cycle of poor digestion and physical unease can start affecting your mental and emotional health. You may begin to feel:
- Frustrated
- Irritable
- Depressed
- Negative about life
- Fatigued or emotionally drained
And when this state persists, it becomes more than just a digestive issue—it becomes a deep psychosomatic condition, where the mind and body both suffer.
Why Chronic Pancreatitis Is So Challenging
In my 18 years of experience, and through observing the work of many of my senior colleagues, I have seen that chronic pancreatitis is one of the most difficult conditions to manage, especially when the patient comes at a late stage. Often, people ignore early signs or rely solely on temporary relief, only to seek naturopathic or holistic care as a last resort—when the damage has already progressed significantly.
At that point, the expectation is high, but hope is low.
Patients believe that since natural therapies have no side effects, results should be fast and dramatic. But the truth is, healing takes time—especially in chronic cases. And more than just treating the body, we have to start by treating the mind.
Healing Begins with Understanding
Before beginning any treatment, it’s important to address the patient’s mental and emotional state. Many chronic pancreatitis patients:
- Struggle to accept their condition
- Ask “Why did this happen to me?”
- Feel hopeless or emotionally shut down
- Carry unrealistic expectations for a quick fix
As therapists, this becomes a true challenge. We are not just working on the physical damage, but also restoring hope, balance, and positivity in the mind of the patient. Only when the patient is mentally ready to receive healing, does the real recovery process begin.
When Confidence Awakens Healing
Once a patient gains confidence and trust in the healing process, true treatment begins. Healing is not only about physical remedies—it is deeply connected to mental readiness. In many chronic cases, the reversal of damage is only possible when the mind is aligned with the therapy.
However, pancreatitis doesn’t always follow a predictable pattern. Sometimes, despite no history of alcohol consumption, diabetes, or any other obvious risk factor, a person may still develop inflammation of the pancreas. This type of unexplained condition is known as Idiopathic Pancreatitis.
What Is Idiopathic Pancreatitis?
“Idiopathic” means no identifiable cause. You may come across this term in test reports or case files from previous visits to allopathic doctors or hospitals. Even when all standard tests are done and major risk factors are ruled out, the root cause remains unknown.
In fact, studies and experience show that nearly 50–60% of pancreatitis cases may be idiopathic—a significant number. This makes the condition all the more challenging, especially in natural or integrative healing systems where identifying the cause is a crucial step in choosing the right treatment path.
Complications of Pancreatitis
Pancreatitis—especially when chronic—can lead to severe, life-altering complications, which may affect multiple systems in the body. Some of the most serious complications include:
- Kidney failure
- Respiratory issues (breathing difficulties)
- Infections (due to lowered immunity and inflammation)
- Malnutrition (from poor digestion and absorption)
- Diabetes mellitus
- Pancreatic cancer (in rare, prolonged cases)
While pancreatic cancer is not typically a direct result of acute pancreatitis, it becomes a real risk in chronic conditions where the pancreas has been repeatedly inflamed and damaged over time.
The Ripple Effect on Other Organs
Because the pancreas is responsible for secreting digestive enzymes and hormones like insulin, any dysfunction here affects other vital organs.
The kidneys, for instance, are among the first organs to suffer. They are the main detoxification and excretory system in the human body. This is why Mother Nature has gifted us two kidneys—to handle the heavy burden of filtering and removing waste and toxins.
But when the pancreas is under stress or failing, the toxic load increases, digestion weakens, and as a result, the kidneys often become overburdened. One of the most common related problems is the formation of kidney stones—a signal that the body’s detoxification pathways are struggling.
How Pancreatic Issues Affect Other Organs
Pancreatitis and other pancreatic disorders often lead to a chain reaction that impacts multiple organs in the body. Let’s take a closer look at how the kidneys, lungs, immunity, and digestion are affected.
- Kidneys: The Silent Sufferers
When the pancreas is inflamed or damaged, toxic byproducts build up in the body. This puts extra pressure on the kidneys, which are responsible for filtering and eliminating these toxins.
- Creatinine levels, blood urea nitrogen (BUN), and uric acid may rise—these are markers of kidney stress or dysfunction.
- Nephrons, the functional units of the kidneys, can become damaged over time.
- If not addressed early, this burden can lead to kidney disease or even failure.
- Lungs and Breathing Problems
Pancreatic inflammation can also affect the lungs, especially in severe or chronic cases:
- Carbon dioxide retention may increase.
- Oxygen levels in the blood can drop.
- This imbalance can lead to breathing difficulties, a serious complication often seen in advanced pancreatic disease.
- Digestive Issues and Malnutrition
Since the pancreas plays a major role in digestion, its dysfunction directly impacts:
- Enzyme production needed to break down food.
- Nutrient absorption in the intestines.
So even if a person eats well or takes supplements, their body may not absorb enough nutrients, leading to malnutrition. This is why patients often experience:
- Fatigue
- Weakness
- Weight loss
- Vitamin and mineral deficiencies
- Weakened Immunity and Infections
A weak digestive system often leads to a weakened immune system, making the body more vulnerable to:
- Frequent infections
- Slower recovery
- Chronic fatigue or inflammation
Your immune system depends heavily on a healthy metabolism and a well-functioning gut. Once these are disturbed, the body’s defense becomes compromised.
- Blood Sugar Imbalance and Diabetes Mellitus
One of the pancreas’s most crucial functions is secreting insulin, which helps regulate blood sugar. When insulin production drops:
- Glucose builds up in the bloodstream.
- It is not converted into glycogen (the stored form of sugar).
- This leads to diabetes mellitus, a condition that is now incredibly common worldwide.
Without sufficient insulin, sugar stays in the blood and causes long-term damage to nerves, blood vessels, kidneys, and eyes—among other systems.
Risk Factors for Pancreatic Disease and Cancer
If pancreatic issues, such as chronic pancreatitis, go untreated or are poorly managed, they can lead to complications like pancreatic cancer. Cancer occurs when abnormal cells multiply uncontrollably, and it can affect any organ, including the pancreas.
Who’s at Risk for Pancreatic Cancer and Chronic Pancreatitis?
Several risk factors increase the likelihood of developing pancreatitis or pancreatic cancer, especially in older adults. Here are the most significant ones
- Age:
-
- People over 60 years old are at the highest risk.
- Chronic Diabetes Mellitus:
- Patients with diabetes for more than 15–20 years who struggle to control their HbA1c levels (a measure of long-term blood sugar control) are particularly vulnerable. If their HbA1c remains above 10%, it indicates poor blood sugar management, which increases the risk of pancreatic disease.
- Obesity:
- Those with a BMI (Body Mass Index) over 30 are at increased risk. Obesity can lead to inflammation in the pancreas, increasing the likelihood of disease.
- Heavy Alcohol Consumption:
- Regular, heavy alcohol use is a major contributor to chronic pancreatitis. While moderate drinking may not cause harm, heavy drinking puts excessive strain on the pancreas and can lead to inflammation and tissue damage.
- Medications for Blood Thinning:
- People who take blood thinners or have a history of heart problems may be more prone to pancreatitis. These medications can affect the pancreas by altering blood flow or creating complications during medical treatments.
- Chronic Kidney Disease:
- Those with a history of kidney problems (like high blood pressure, kidney stones, or chronic kidney disease) are at an increased risk of developing pancreatitis. Since the pancreas and kidneys work closely together in detoxification, kidney disease can contribute to pancreatic dysfunction.
- History of Jaundice:
- Patients who have experienced severe jaundice (yellowing of the skin and eyes) due to liver issues are at a higher risk. If the jaundice wasn’t fully treated or controlled, it could lead to long-term complications, including pancreatitis.
Acute Pancreatitis and Hospitalization
In some severe cases, acute pancreatitis may require hospitalization for proper treatment. Even with alternative therapies, there are instances when modern medical intervention is necessary. In these situations, doctors will monitor for specific signs:
- Heart rate higher than 90 beats per minute (tachycardia).
- Severe abdominal pain and inflammation.
- Difficulty managing blood sugar or breathing issues.
- Kidney function monitoring for signs of failure.
Key Indicators for Chronic Pancreatitis Complications
When dealing with chronic pancreatitis, certain vital signs and lab results are crucial to assess the patient’s condition and determine the severity of their illness. As part of the first consultation, doctors should evaluate:
- Heart Rate:
- If the heart rate is consistently over 90 beats per minute, it might indicate systemic inflammation or stress due to the body’s response to pancreatitis. Elevated heart rate is common with infection or severe pain.
- Body Temperature:
- A temperature lower than 36°C (hypothermia) suggests sepsis or a severe infection that the body is struggling to manage. This is a serious complication and needs urgent medical attention.
- Respiratory Rate:
- If the respiratory rate is greater than 20 breaths per minute, it can signal respiratory distress or metabolic acidosis, conditions often seen in severe pancreatitis or when other organs start failing (such as kidneys or lungs).
- Complete Blood Count (CBC) Findings:
- An elevated white blood cell count (greater than 12,000 cells per microliter) is a classic sign of infection or inflammation. This is important when diagnosing pancreatitis or determining the presence of complications like infection or abscesses.
Autoimmune Pancreatitis (AIP)
In addition to chronic and acute pancreatitis, another condition to be aware of is Autoimmune Pancreatitis (AIP). This is a form of chronic inflammation of the pancreas where the body’s own immune system attacks the pancreas, mistaking it for an invader. Here’s what you need to know:
- Cause:
- The exact cause of AIP is unknown. However, it is often triggered by the body’s immune system attacking its own tissues due to a long-term bacterial infection, allergies, or other immune system dysfunctions.
- Treatment:
- AIP usually responds to steroid therapy, which reduces the inflammation caused by the immune system’s attack on the pancreas. However, it can be challenging to diagnose initially because it may mimic other forms of pancreatitis or autoimmune disorders.
- Connection to Other Conditions:
- AIP may be linked to other autoimmune diseases or conditions like ulcerative colitis or primary sclerosing cholangitis. It is essential to rule out other causes when treating a patient with suspected autoimmune pancreatitis.
Key Details on Autoimmune Pancreatitis (AIP)
To summarize, autoimmune pancreatitis is when the body’s immune system attacks the pancreas, leading to chronic inflammation. It is divided into two types:
Type 1 AIP (IgG4-related disease)
- More common in men.
- Affects multiple organs: In addition to the pancreas, other organs like the kidneys, lungs, and liver can also be involved.
- More common in East Asia.
- IgG4 levels are typically elevated in this type, and patients may experience other autoimmune diseases.
- Can be more severe because it affects a range of organs, not just the pancreas.
Type 2 AIP
- Affects only the pancreas.
- It is associated with inflammatory bowel diseases like ulcerative colitis and Crohn’s disease.
- More common in women.
- More common in Europe and the USA compared to Asia.
- Less severe than Type 1, affecting only the pancreas and not other organs.
Symptoms of Autoimmune Pancreatitis (AIP)
When autoimmune pancreatitis is detected, common symptoms include:
- Pain in the upper abdomen: This is typically where the pancreas is located, and any inflammation or swelling due to AIP can cause discomfort.
- Pain in the middle back: Because the pancreas lies behind the stomach, inflammation can also radiate pain to the back, often between the shoulder blades.
- Fatigue and weight loss: Like other forms of pancreatitis, AIP can affect digestion and absorption of nutrients, leading to unexplained fatigue and unintended weight loss.
- Jaundice: In some cases, inflammation of the pancreas can block bile ducts, leading to yellowing of the skin and eyes.
- Digestive issues: Due to the pancreatic inflammation, digestive enzymes may not be secreted properly, leading to malabsorption, bloating, and fatty stools (steatorrhea).
- Other autoimmune symptoms: Since AIP is related to an autoimmune response, patients may experience symptoms from other autoimmune conditions as well, like joint pain, rashes, or swollen glands.
Diagnosis and Treatment of AIP
- Diagnosis:
- Diagnosis is challenging because symptoms can overlap with other forms of pancreatitis. Doctors rely on blood tests (e.g., IgG4 levels), imaging techniques like CT scans or MRI, and sometimes biopsy of pancreatic tissue for confirmation.
- CT or MRI scans are typically used to assess the size and shape of the pancreas, and to check for any mass or inflammation.
- Treatment:
- Steroids (e.g., prednisone) are the main treatment, as they help reduce the inflammation caused by the autoimmune response.
- Immunosuppressive drugs may also be used if steroids are ineffective or if the disease relapses.
- Long-term follow-up is necessary, as AIP can relapse, and patients might need ongoing management.
- Diet and Lifestyle:
- Dietary changes are important to manage the symptoms, as AIP can affect digestion. Eating smaller, more frequent meals and a low-fat diet can help.
- Avoiding alcohol is crucial since alcohol can aggravate the condition.
Key Differences in Symptoms of Autoimmune Pancreatitis (AIP) vs. Other Pancreatitis:
- Back Pain:
- Autoimmune pancreatitis (AIP): Pain is often described as being in the upper abdomen and middle back. This can help differentiate AIP from other types of pancreatitis, where back pain is typically not a primary symptom.
- Other forms of pancreatitis: Generally, abdominal pain is more common and tends to be deep and localized in the upper abdomen. Back pain is typically not a prominent symptom.
- Fatigue and Weakness:
- One of the hallmark symptoms of AIP is extreme fatigue or weakness despite adequate rest, proper diet, and normal routine. This can occur even after standing for just a short time, like 20 minutes, and is a classic sign of autoimmune pancreatitis.
- Other types of pancreatitis may also cause fatigue, but it is less specifically noted as a prominent symptom compared to AIP.
- Dark Urine and Jaundice (Yellow Skin/Eyes):
- AIP: The presence of dark urine and yellow skin/eyes (jaundice) is more noticeable in AIP due to pancreatic involvement and liver dysfunction, which can block bile ducts and cause the liver to release bilirubin into the bloodstream.
- Other pancreatitis: Jaundice can also be present, particularly in cases where there is a gallstone blockage or pancreatic duct obstruction.
- Loss of Appetite:
- AIP: The loss of appetite in autoimmune pancreatitis is often associated with a psychosomatic response. The patient may experience fear or phobia around eating due to the anticipated pain or discomfort. This can be a cycle where fear and discomfort prevent the patient from eating, leading to further malnutrition and weakness.
- Other pancreatitis: Loss of appetite can also be common in other forms of pancreatitis, but it might not be as strongly tied to the psychosomatic component as in AIP. The pain or discomfort experienced after eating in pancreatitis is usually more related to inflammation or digestive issues rather than a psychological aversion.
Psychosomatic Factors in AIP:
The link between gut health and brain health is becoming more recognized, and AIP seems to highlight this connection. When the gut-brain axis is disrupted, it can lead to psychosomatic issues such as the fear of eating or phobia that prevents patients from eating properly. The neurotransmitters in the brain communicate with the stomach, sending signals that food could cause discomfort, even if the body isn’t experiencing physical pain at the time.
How these Symptoms Help with Diagnosis:
- If you encounter a patient who presents with upper abdominal pain, back pain, extreme fatigue, dark urine, jaundice, and loss of appetite, it could be a strong indication of autoimmune pancreatitis (AIP).
- Psychosomatic signs such as fear of eating due to pain or discomfort, as well as a loss of appetite, are crucial for identifying the psychological impact of AIP, which is not as common in other forms of pancreatitis.
Treatment Considerations:
Given the psychosomatic component, autoimmune pancreatitis treatment might require a holistic approach that addresses not only the physical symptoms (through steroid therapy, for example) but also the psychosomatic aspects, such as cognitive behavioral therapy (CBT) or stress management techniques.
- Steroids are the primary treatment for reducing inflammation.
- If psychological issues like anxiety or depression are contributing to the symptoms, involving a mental health professional or incorporating relaxation techniques can be a key part of treatment.
Key Insights:
- Autoimmune Pancreatitis (AIP) and Acute Pancreatitis: You mentioned that if acute pancreatitis is not treated early or adequately, it can progress to chronic pancreatitis or autoimmune pancreatitis (AIP). This progression happens because of repeated episodes of inflammation and damage to the pancreas, leading to a vicious cycle of chronic disease. It’s clear that early detection and treatment of acute episodes are crucial in preventing long-term complications.
- Pancreatic Cancer: As you pointed out, pancreatic cancer is the third leading cause of cancer-related death in the United States. The connection between chronic pancreatitis (including AIP) and pancreatic cancer is well-established. Here’s a summary of the pathway:
- Repeated episodes of pancreatitis cause persistent damage to the pancreas.
- Over time, this damage leads to the dysfunction of pancreatic cells, including the beta cells responsible for producing insulin.
- As these cells become damaged, the pancreas cannot perform its normal functions, leading to cellular stress, and in some cases, this can trigger uncontrolled cell multiplication, which leads to cancer formation.
- Since the pancreas is a vital organ responsible for digestion and hormone production, the damage to its function further exacerbates the situation.
Statistics:
- In 2022, 62,210 people were estimated to be diagnosed with pancreatic cancer in the U.S. According to the American Cancer Society, the survival rate for pancreatic cancer is relatively low due to its late detection, which is often linked to ongoing or untreated pancreatic diseases.
Why Early Treatment is Crucial:
The key takeaway from your explanation is that early treatment of acute pancreatitis or chronic pancreatitis (and addressing other related pancreatic conditions like autoimmune pancreatitis) is vital to prevent the progression to more severe complications like pancreatic cancer. When the pancreas is damaged and its cells malfunction, it becomes much harder to reverse the damage, which increases the risk of cancer.
- If patients can manage acute pancreatitis before it becomes chronic, or if autoimmune pancreatitis is treated early, there is a better chance of avoiding severe complications, including pancreatic cancer.
- Chronic damage to the pancreas, whether caused by autoimmune pancreatitis or repeated acute episodes, can lead to further complications such as malnutrition, diabetes, kidney failure, and even pancreatic cancer.
Why Pancreatic Cancer is So Difficult to Treat:
- Late Detection: Pancreatic cancer often remains asymptomatic or presents with symptoms that are easily confused with other conditions (like back pain, abdominal discomfort, and digestive issues) until it’s already at an advanced stage. By this time, the cancer has often spread, which reduces the effectiveness of treatment options.
- Lack of Specific Medication: As you pointed out, no specific medication has been developed to directly target pancreatic cancer. Unlike other cancers, where chemotherapy, radiation, or specific oral medications can be used effectively, pancreatic cancer does not respond well to these treatments. The cancer is particularly resistant to traditional therapies because it’s often diagnosed when the disease is already widespread.
- Multiple Contributing Factors: Pancreatic cancer is typically the result of multiple underlying problems, such as chronic pancreatitis, diabetes, or obesity, among others. It’s the culmination of long-term damage and dysfunction in various organs that leads to cancer development. This complexity makes it hard to treat and difficult to reverse because targeting just one aspect of the disease (such as controlling diabetes or treating pancreatitis) is not enough to stop the progression of cancer.
Symptoms of Pancreatic Cancer:
As you mentioned, symptoms of pancreatic cancer can overlap with those of other pancreatic diseases, which is why it can be easily overlooked until it’s in a more advanced stage. Common symptoms include:
- Drastic weight loss: This isn’t just a gradual reduction; it’s significant and rapid weight loss, often accompanied by a decrease in appetite and changes in mental health.
- Abdominal discomfort and pain: This pain often radiates to the back, making it harder to differentiate from other conditions.
- Development of type 2 diabetes: Pancreatic cancer can disrupt insulin production, leading to new onset diabetes or worsening of existing diabetes.
- Jaundice: If tumours block the bile ducts, it can lead to jaundice (yellowing of the skin and eyes), which is a classic sign of pancreatic cancer.

Why Naturopathy Can Help:
Although modern medicine has no definitive cure for pancreatic cancer, naturopathy can offer support in managing the symptoms and improving the quality of life for patients. Naturopathy can help by:
- Improving overall lifestyle: Focusing on nutrition, stress management, and physical activity to reduce symptoms.
- Managing symptoms: Addressing symptoms like weight loss, loss of appetite, digestion issues, and mental health challenges through natural therapies.
Risk Factors for Pancreatic Cancer:
- Excessive Alcohol Consumption: Chronic alcohol abuse can lead to chronic pancreatitis, which is a precursor to pancreatic cancer. The inflammation and damage from alcohol can increase the risk of cancer developing in the pancreas over time.
- Cigarette Smoking: Smoking is one of the most significant modifiable risk factors for pancreatic cancer. It is responsible for a considerable percentage of pancreatic cancer cases. The chemicals in tobacco smoke damage pancreatic cells and can lead to the development of cancer.
- Long History of Diabetes Mellitus: Diabetes, especially when poorly controlled, can increase the risk of developing pancreatic cancer. Type 2 diabetes, which often develops over many years, is particularly associated with pancreatic cancer due to the strain it places on the pancreas and its insulin-producing cells.
- Obesity: Excess body fat, especially abdominal fat, is a well-established risk factor for pancreatic cancer. Obesity leads to increased insulin resistance, which may contribute to the development of cancer in the pancreas.
- Diet Rich in Animal Fats: As you mentioned, the Western diet, which is high in animal fats (red meat, processed meats), can increase the risk of pancreatic cancer. This diet is common in Europe and the U.S., where the consumption of these foods is much higher than in Asian diets. The high fat content, combined with low fiber intake, creates an environment that may increase the risk of pancreatic cancer.
- Chemical Exposure: Workers in industries that use or produce chemical fertilizers, pesticides, or industrial chemicals are at a higher risk of pancreatic cancer due to long-term exposure to harmful substances. This includes those working in agricultural fields, chemical factories, and cement plants.
- Infections (e.g., Helicobacter pylori): Certain bacterial infections have been linked to an increased risk of developing pancreatic cancer. Helicobacter pylori (H. pylori) infection, which is known to cause stomach ulcers, has also been found in some studies to increase the risk of pancreatic cancer, although the exact mechanism is still under investigation.
- Genetic Factors: While the exact genetic causes are still being studied, it’s known that certain inherited genetic mutations can increase the risk of pancreatic cancer. Families with a history of pancreatic cancer, or those who have genetic syndromes like BRCA mutations (which are more commonly associated with breast and ovarian cancers) or Lynch syndrome, are at higher risk.
 Signs and Symptoms to Watch For:
Signs and Symptoms to Watch For:
Given the risk factors, being aware of the early signs and symptoms of pancreatic disease is important. These include:
- Persistent abdominal pain, especially in the upper abdomen or middle back.
- Loss of appetite and unexplained weight loss.
- Dark urine and yellowing of the skin (jaundice) or eyes.
- Fatigue and weakness despite adequate rest.
- Changes in stool colour, such as pale or clay-coloured stool.
Diagnosis and Prognosis:
To confirm whether the symptoms are due to pancreatitis, autoimmune pancreatitis (AIP), or pancreatic cancer, a prognosis is made based on the patient’s symptoms. Doctors often use diagnostic tests such as:
- Blood tests (to check liver function, pancreatic enzymes, etc.)
- Imaging tests (CT scan, MRI, ultrasound) to look for any abnormalities in the pancreas.
- Endoscopic tests (like endoscopic ultrasound or biopsy) to get a tissue sample for further examination.
Early detection is key to improving the prognosis, especially for conditions like pancreatic cancer, where survival rates are low if the disease is not caught in its early stages.
Prevention and Management
The risk of pancreatic cancer can be reduced by:

- Avoiding smoking and limiting alcohol consumption.
- Maintaining a healthy weight and eating a balanced diet with plenty of fruits, vegetables, and whole grains (and limiting processed foods and animal fats).
- Managing diabetes and controlling blood sugar levels.
- Limiting exposure to harmful chemicals in workplaces.
- Regular medical check-ups for people with a family history of pancreatic cancer or those with genetic predispositions.
Common Symptoms of Pancreatic Problems:
- Upper Abdominal Pain:
- This is one of the most common symptoms of pancreatic disease. The pain may radiate to the back or even the chest. It’s typically deep and persistent.
- Often, this pain worsens after eating, as the pancreas is involved in digestion. This is also linked to psychosomatic symptoms, where the patient starts fearing that eating will trigger pain, leading to an avoidance of food and subsequent weight loss.
- Nausea and Vomiting:
- These are common reactions when the pancreas isn’t functioning properly. This is because digestive enzymes and hormones like insulin are not being secreted in the right amounts, leading to digestive disturbances and discomfort.
- Weight Loss:
- Weight loss in pancreatic disease, especially pancreatic cancer, can be drastic. It occurs due to several factors: a lack of proper digestion (because the pancreas isn’t producing enough enzymes) and possibly because the body is not absorbing enough nutrients.
- Jaundice:
- Yellowing of the skin and eyes (jaundice) occurs when the liver’s bile ducts are blocked or when there is a malfunction in bile production or secretion, which can happen in pancreatic diseases like pancreatic cancer or AIP. It indicates liver involvement.
- Fever and Rapid Heart Rate:
- A fever can indicate inflammation or infection within the pancreas (as in acute pancreatitis). A rapid heart rate (tachycardia) can also signal stress or infection affecting the body.
- Swollen Abdomen:
- Unlike bloating or flatulence, which may come and go, a swollen abdomen is usually more pronounced and persistent. This can happen when there is fluid retention or inflammation caused by pancreatitis. It may also occur in cases of pancreatic cancer where tumours affect the structure of the pancreas and surrounding tissues.
Additional Symptoms to Look Out For:
- Loss of Appetite: This may happen alongside weight loss, where patients have no desire to eat due to the pain or discomfort they associate with eating.
- Steatorrhea (Fatty Stools): The inability to properly digest fats due to insufficient pancreatic enzymes can lead to fatty, pale stools that float and have an unpleasant odor.
- Fatigue: Constant tiredness and weakness, even with adequate rest, can result from malnutrition, poor digestion, or the body’s struggle with chronic disease.
How These Symptoms Help in Diagnosis:
These symptoms are often indicative of pancreatic problems, but they can also overlap with other conditions like gallbladder disease, liver problems, or gastrointestinal issues. Proper diagnosis usually involves:
- Detailed History: A thorough patient history to check for risk factors (e.g., alcohol consumption, family history, diabetes).
- Physical Examination: Doctors assess the patient’s physical symptoms, such as abdominal swelling, jaundice, and tenderness in the abdomen.
- Blood Tests: Blood tests to check for elevated levels of pancreatic enzymes (e.g., amylase, lipase), liver function tests, or signs of infection or inflammation.
- Imaging: CT scans, MRI, or ultrasound to visualize the pancreas and detect any abnormalities such as inflammation, tumours, or cysts.
- Endoscopic Tests: In some cases, endoscopic ultrasound or biopsy may be used to get a closer look at the pancreas and confirm the diagnosis.
Psychosomatic Symptoms:
As you mentioned, the psychosomatic aspect of pancreatic disease can also play a role in the loss of appetite and avoidance of food. Patients may experience fear or anxiety associated with eating, knowing that it could trigger pain. This can exacerbate malnutrition and further weaken the body.
Next Steps for Diagnosis:
Once a physician identifies these symptoms, they would likely order a series of diagnostic tests to narrow down the possible causes. If there is a strong suspicion of pancreatic cancer or chronic pancreatitis, further tests like biopsies or endoscopic procedures may be required for definitive diagnosis.
Key Symptoms of Pancreatic Issues:
- Swollen Right Side:
- Swelling on the right side of the abdomen can indicate inflammation or fluid buildup, possibly due to a disturbed pancreas or other abdominal organs. This could be a sign of pancreatitis or a tumor pressing on nearby structures.
- Rapid Heart Rate:
- A rapid heart rate (tachycardia) can occur due to inflammation, infection, or the body’s stress response. It’s also common in acute pancreatitis, especially if there’s a significant fluid loss or infection.
- Greasy, Foul-Smelling Stool:
- The presence of greasy, foul-smelling stool (steatorrhea) is a classic symptom of pancreatic insufficiency, where the pancreas fails to produce enough digestive enzymes. This leads to poor digestion of fats, resulting in fatty stools.
- Fluid Buildup in the Belly (Ascites):
- This indicates a severe problem, possibly related to pancreatic cancer or chronic pancreatitis. Fluid buildup in the abdomen can occur due to inflammation or tumor formation in the pancreas, and it often causes the abdomen to feel bloated or swollen.
- Sudden Drop in Blood Pressure (Hypotension):
- A sudden drop in blood pressure can be related to acute pancreatitis or severe fluid loss. It might also indicate a severe infection or internal bleeding related to the pancreas.
- Fullness, Indigestion, and Hiccups:
- Indigestion and a sense of fullness are common when the pancreas isn’t functioning properly. It might also lead to hiccups, which can be a sign of pancreatic inflammation affecting the diaphragm or nerves in the area.
How These Symptoms Help in Diagnosis:
By identifying these symptoms early on, healthcare providers can make an informed assessment of the patient’s condition and recommend further diagnostic tests, such as blood tests, imaging studies (e.g., ultrasound, CT scans, MRI), or even biopsy for more accurate diagnosis.
Preventing Pancreatic Diseases:
While pancreatitis and other pancreatic conditions cannot always be prevented, there are several preventive measures that can help reduce the risk of developing a pancreatic disorder:
- Healthy Lifestyle:
- Maintaining a healthy weight and consuming a balanced diet, particularly low in saturated fats, can help reduce the strain on the pancreas.
- Regular exercise supports overall metabolic health, including glucose regulation and fat digestion, both of which affect the pancreas.
- Avoiding Risky Substances:
- Limiting alcohol consumption is crucial. Heavy drinking is a major risk factor for pancreatitis and can lead to pancreatic cancer over time.
- Quitting smoking can significantly reduce the risk of developing pancreatic cancer and other pancreatic diseases.
- Managing Health Conditions:
- Controlling diabetes (especially type 2 diabetes) and avoiding obesity can help prevent pancreatitis and reduce the risk of developing pancreatic diseases.
- Early Detection and Monitoring:
- For individuals at higher risk (e.g., family history of pancreatic cancer or pancreatitis, long-term alcohol consumption), regular check-ups and screenings are important.
🩺 Treatment Overview for Pancreatic Diseases (Pancreatitis, IIP, Pancreatic Cancer)
- Pain Management
- Goal: Reduce inflammation and provide relief from abdominal and back pain.
- Common Medications:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs):
- Example: Diclofenac, Ibuprofen, Paracetamol.
- These reduce inflammation and help in relieving mild to moderate pain.
- Severe Pain Cases:
- May require opioids under close medical supervision if NSAIDs aren’t enough.
- Antibiotics:
- Given only if infection is suspected or confirmed.
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs):
- Nutritional Support
- Due to the pancreas’ role in digestion, when it gets inflamed, absorption of nutrients becomes poor.
- Why is it critical? Without proper nutrient absorption, the body becomes weak, leading to malnutrition, fatigue, and weight loss.
- Management Includes:
- IV fluids (if oral intake isn’t possible)
- High-protein, low-fat diets
- Vitamin and mineral supplements (especially A, D, E, K — fat-soluble vitamins)
- Pancreatic enzyme supplements (in some chronic cases)
- Hydration is Key
- As you said perfectly — dehydration is one of the biggest dangers.
- Pancreatitis or pancreatic dysfunction often causes fluid loss (through vomiting, diarrhea, fever).
- Doctors focus first on:
- Oral Rehydration
- Or in severe cases, IV fluid therapy to stabilize the patient.
- Hospital-Based Interventions (in moderate to severe cases):
- Endoscopic or surgical procedures may be needed:
- For drainage of fluid collections
- To remove obstructions or damaged tissue
- In pancreatic cancer, depending on stage:
- Surgery (Whipple procedure), chemotherapy, or radiation therapy might be considered.
- Supportive Therapy in Naturopathy/Yoga (as a complement):
- Lifestyle correction, mental relaxation, diet regulation.
- Yoga, meditation, and natural detox techniques can help in long-term recovery and symptom control.
✅ Prevention and Recovery Tips You Can Advise Patients:
- Avoid heavy, fatty meals.
- Quit alcohol and smoking.
- Eat fresh, fibre-rich, plant-based food.
- Stay hydrated.
- Regular light exercise.
- Manage stress and improve sleep quality.
- Listen to the body — if digestion is poor, rest the system with light foods or fasting under guidance.
🔬 Diagnostic Tests for Pancreatic Disorders
✅ 1. Blood Tests
To detect signs of inflammation and organ function:
- Amylase & Lipase:
- Key markers of pancreatitis — elevated levels indicate acute inflammation.
- Liver function tests (LFTs):
- Help check for bile duct obstruction or liver involvement.
- Blood glucose levels:
- To check for development of diabetes or insulin imbalance.
- CBC (Complete Blood Count):
- To identify infection or inflammation (high WBC).
- CRP (C-Reactive Protein):
- Helps evaluate the severity of inflammation.
- Kidney Function Tests (BUN, Creatinine):
- To check if kidneys are affected — especially in severe pancreatitis.
✅ 2. Imaging Tests
These help in identifying structural changes, fluid buildup, necrosis, or tumours:
- Ultrasound (Abdominal):
- First-line test to detect gallstones or swelling of the pancreas.
- CT scan (Contrast-enhanced):
- Gold standard for evaluating severity and complications like pseudocysts or necrosis.
- MRI / MRCP (Magnetic Resonance Cholangiopancreatography):
- Advanced imaging to visualize pancreatic and bile ducts.
- Endoscopic Ultrasound (EUS):
- Helpful in detecting small tumours, cysts, or bile duct issues.
✅ 3. Stool Test
- Faecal elastase test:
- Detects pancreatic enzyme insufficiency in chronic pancreatitis.
✅ 4. Biopsy (if needed)
- In case of suspected pancreatic cancer, a tissue biopsy via EUS-guided fine needle aspiration is done for confirmation.
📌 Summary: Why Diagnostic Tests Matter
- Help differentiate between acute, chronic, and cancer-related pancreatic issues.
- Assist doctors in tailoring treatment based on:
- Presence of organ failure,
- Systemic complications,
- Severity score (like Ranson’s Criteria or APACHE II score).
- Guide whether to hospitalize, ICU admit, or manage conservatively.
🧪 Diagnostic Tests for Pancreatic Disorders (Verbal Flow Structured)
🩸 1. Blood Tests (Initial Screening)
- CBC (Complete Blood Count)
To detect inflammation or infection (WBC count especially). - Serum Amylase & Serum Lipase
- These two enzymes are produced by the pancreas.
- High levels = sign of acute pancreatitis.
- Low or abnormal levels = may suggest chronic damage or insufficiency.
🧪 2. Liver Function Test (LFT)
- Since bile and pancreatic enzymes work together,
checking liver function helps assess any blockages or dysfunctions in digestion.
🖥️ 3. Imaging
- Ultrasound (Abdominal)
First line for detecting stones, swelling, fluid, or pancreatic size. - CT scan / CECT Abdomen
Gives a detailed picture of pancreatic inflammation, cysts, or necrosis.
🧬 4. ERCP (Endoscopic Retrograde Cholangiopancreatography)
- Also known as the Endoscopy Test.
Used to view pancreatic and bile ducts. Can also treat small blockages.
🔬 5. Biopsy (If Cancer Suspected)
- Performed only when there’s doubt or suspicion of pancreatic cancer.
- Confirms malignancy through tissue analysis.
✅ Why These Tests Matter
- Helps stage the disease (Acute? Chronic? Cancer?).
- Guides whether to use conservative care or more advanced intervention.
Now you’re ready to shift the tone

🌿 Transition to Naturopathy
“Now we’ve discussed how the pancreas works, the common types of disorders — like acute pancreatitis, chronic inflammation, or pancreatic cancer — and how modern medicine diagnoses and treats them… But now let’s talk about how naturopathy plays a major role in recovery and prevention.”
You can now continue by explaining:
- Lifestyle correction,
- Detox methods,
- Herbal support,
- Diet adjustments,
- Yoga and hydrotherapy techniques in naturopathy.
🌿 Naturopathic Treatment for Pancreatic Disorders
🌱 Based on the Five Elements of Nature:
Naturopathy uses Earth, Water, Fire, Air, and Ether — all integrated in simple, natural therapies to support healing from within.
 🧘♂️ Treatment Principles
🧘♂️ Treatment Principles- Treatment remains consistent: Based on natural elements
- Variations depend on:
- Patient’s condition
- Severity of symptoms
- Appetite and digestion levels
- Duration of illness
🔥 Gastro-Hepatic Pack (GH Pack) Therapy
✅ Highly effective in liver, pancreas, and kidney disorders
✅ Core therapy in Naturopathy for digestive health🎥 [Video Demo Recap: GH Pack Application]
- Application of:
- Hot water bag (back side – over the liver/pancreas region)
- Cold or normal water bag (front – over the abdomen)
- Helps apply heat and cold stimulation therapy together
📌 Important Guidelines
- The correct position: Patient must lie down flat for 30 minutes
(The video showed sitting position just for demo purposes) - Minimum 30-minute therapy per session
- Can be repeated daily or on alternate days depending on condition
💡 Therapeutic Benefits
- Reduces inflammation in stomach and pancreas
- Stimulates beta cell regeneration (helps in diabetes and pancreatic healing)
- Promotes better digestion and secretion of enzymes
- Enhances blood circulation in the abdominal organs
- Helps reduce toxins and supports detoxification
🔥 Gastro-Hepatic Pack (GH Pack) – Continued
✅ Usage Guidelines:
- From Day One: Patients can begin GH Pack therapy right away
- Consistency is key: Continue until clear signs of recovery
- Safe & Non-invasive: No side effects if used correctly
⚠️ Precaution:
- For female patients, avoid GH Pack therapy during menstrual cycles (4–5 days)
- Resume therapy after the cycle is complete
🌍 Earth Element: Mud Therapy
Deeply grounding and detoxifying – mud therapy works directly on the abdominal region.
🌿 Mud Application – Abdominal Pack
- Mud Used: Preferably deep-sea black mud or clean natural clay
- Soaking: Mud should be soaked overnight in clean water (for proper cooling and consistency)
🧴 Application Method:
- Apply a thick layer of soaked mud on the abdomen
- Cover with a cotton cloth or plastic sheet to avoid dripping
- Duration: 30–45 minutes
- After the therapy, clean with lukewarm water
🌟 Therapeutic Effects:
- Relieves gas, acidity, and inflammation in the abdomen
- Helps reduce toxins and heat from abdominal organs
- Gives relief from pain and swelling
- Promotes smooth digestion and reduces bloating
- Supports pancreatic function through abdominal cooling’
Conclusion
Pancreatic diseases—especially pancreatic cancer—remain some of the most complex and difficult conditions to diagnose and treat in modern medicine. Due to its subtle symptoms and late-stage detection, pancreatic cancer often leads to high mortality rates. While modern treatments offer pain management, nutritional support, and diagnostic tools like blood tests, imaging, and biopsies, there is still no specific cure.
However, naturopathy provides a holistic, supportive role in improving patients’ quality of life. Using nature’s five elements—earth, water, fire, air, and ether—naturopathic treatments such as the Gastro-Hepatic Pack (GH Pack) and Mud Therapy help reduce symptoms, improve digestion, and support the body’s natural healing processes.
By combining lifestyle changes, natural therapies, and preventive care, naturopathy empowers patients to manage pancreatic issues more effectively. Though it is not a replacement for critical medical intervention in severe cases, it plays a valuable role in long-term health maintenance, prevention, and recovery support.
- Patients who have experienced severe jaundice (yellowing of the skin and eyes) due to liver issues are at a higher risk. If the jaundice wasn’t fully treated or controlled, it could lead to long-term complications, including pancreatitis.






