INFERTILITY
Understanding Infertility: Types, Causes, and Implications
Infertility affects millions of couples worldwide, often causing emotional, physical, and psychological challenges. The condition refers to a couple’s inability to conceive after a year of regular, unprotected intercourse. Here, we explore the different types of infertility and physiological factors involved.
Definition of Infertility:
- Infertility is diagnosed when a couple cannot achieve pregnancy after one year of regular, unprotected intercourse.
- It serves as an indication for both partners to undergo medical evaluations to determine potential underlying issues.
Types of Infertility:
- Primary Infertility: This occurs when conception has never taken place in a couple.
- Secondary Infertility: This applies to couples who have previously conceived but are unable to conceive again.
Physiological Infertility:
Certain life stages naturally result in temporary or permanent infertility due to physiological factors. These stages include:
- Before Puberty: The body is not yet capable of reproduction.
- After Menopause: The natural end of a woman’s reproductive years results in permanent infertility.
- Lactational Period: During breastfeeding, hormonal changes may temporarily suppress ovulation, making conception less likely.
When to Seek Help:
Couples are advised to consult a healthcare provider if:
- They have been unable to conceive after a year of unprotected intercourse.
- The woman is over the age of 35, in which case, it’s recommended to seek help after six months of trying.
Infertility can stem from a variety of factors, both medical and physiological. Understanding the types and timing of infertility can help couples approach the issue with clarity and seek appropriate assistance when needed.
Types and Factors of Infertility: A Comprehensive Overview
Infertility is a complex condition with various contributing factors for both men and women. Understanding the types, key concepts, and optimal conditions for conception can help couples approach fertility challenges with better insight and make informed decisions about seeking treatment.
Types of Infertility:
- Female Infertility: This can stem from a range of factors affecting a woman’s reproductive system.
- Ovulatory Causes (20-40%): Involves issues related to ovulation, such as hormonal imbalances that prevent the release of a healthy egg.
- Tubal/Uterine Causes (30-40%): Involves blockages or structural issues in the fallopian tubes or uterus, which can prevent fertilization or implantation.
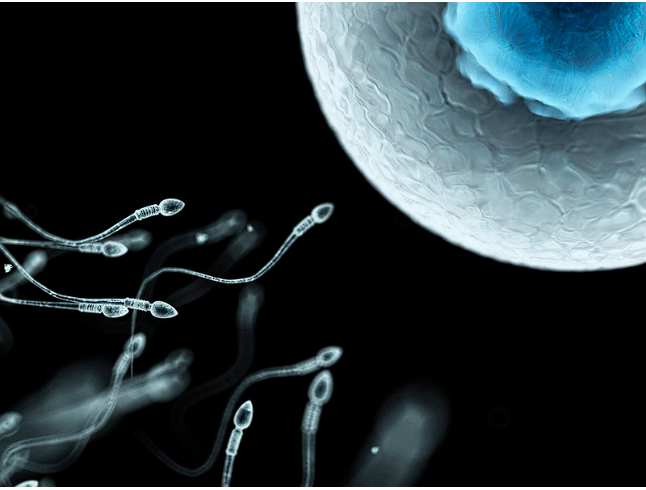
- Male Infertility (30-40%): Factors contributing to male infertility include sperm abnormalities, reduced sperm count, or functional issues that affect sperm’s ability to fertilize an egg.
Key Terms in Infertility:
- Sterility: Refers to the absolute inability to conceive, either due to biological or irreversible factors in one or both partners.
- Fecundability: The probability of achieving pregnancy within a single menstrual cycle. This term reflects a couple’s ability to conceive naturally.
- Fecundity: The probability of achieving a live birth in one menstrual cycle, representing not only conception but the successful progression to a viable birth.
World Health Organization (WHO) Definition of Reproductive Health:
According to the WHO, positive reproductive health in women is defined as a state of complete physical, mental, and social well-being, not merely the absence of reproductive diseases or disorders. This definition emphasizes the importance of a holistic approach to reproductive health, addressing both medical and psychosocial aspects.
Incidence of Infertility:
- The global incidence of infertility is estimated at approximately 15-25%, highlighting its widespread impact.
- Various factors, including lifestyle, environmental conditions, and genetics, contribute to infertility rates in different populations.
Optimal Age for Conception:
- For women, the optimal age for conception is generally between 20-35 years. After age 40, fertility declines significantly, and the risk of chromosomal abnormalities and fetal malformations increases.
- For men, fertility may decline after age 50, primarily due to a decrease in libido and potential sexual dysfunction, though men can remain fertile later into life than women.
Importance of Counseling and Partner Investigation:
When addressing infertility, simultaneous counseling and investigation of both partners is crucial to accurately diagnose the underlying causes and devise an effective treatment plan. Professional support can also help couples manage the emotional and psychological challenges that often accompany fertility issues.
Understanding the types and contributing factors of infertility enables couples to take a proactive approach to reproductive health. By recognizing key terms and optimal conditions for conception, they can make more informed decisions and pursue timely medical interventions if necessary.
Understanding Female Infertility Factors: Causes and Implications

Female infertility can arise from a range of physiological, anatomical, and psychological factors, each affecting different parts of the reproductive system. Recognizing these specific causes can aid in accurate diagnosis and effective treatment.
Psychological and Physical Conditions Affecting Female Fertility:
- Vaginismus: A condition characterized by hyperesthesia, causing involuntary vaginal spasms during intercourse or medical examination, which can hinder conception.
- Dyspareunia: Refers to painful or difficult intercourse, potentially due to physical or emotional factors.
- Anxiety: Physical and psychological anxiety can interfere with sexual function and overall reproductive health.
Ovulatory Factors (20-40% of Female Infertility Cases):
Ovulatory issues impact the release or maturation of eggs and are often linked to hormonal imbalances or underlying health conditions. Key causes include:
- Anovulation: The absence of ovulation, preventing egg release.
- Polycystic Ovarian Disease (PCOD): A hormonal disorder causing irregular ovulation or anovulation.
- Luteal Phase Deficiency (LPD): Insufficient hormone production in the luteal phase, disrupting the menstrual cycle.
- Endocrine Disorders: Conditions like hypothyroidism, hyperprolactinemia, and diabetes that impact hormone levels and ovulation.
- Hypothalamic Dysfunction: Affects hormone production, leading to irregular or absent ovulation.
- Other Causes: Luteinized unruptured follicle syndrome, periovarian adhesions, and related issues can interfere with ovulation.
Tubal Factors:
Damage or obstruction in the fallopian tubes can block sperm from reaching the egg or prevent fertilized eggs from reaching the uterus. Major causes include:
- Bilateral Tubal Obstruction: Partial or complete blockage of both fallopian tubes.
- Tuberculosis (TB): A common cause of tubal infertility, especially in regions where TB is prevalent.
- Pelvic Inflammatory Disease (PID): Infections that cause scarring or blockage in the reproductive tract.
- Post-Abortive or Post-Puerperal Infections: Infections following abortion or childbirth can lead to tubal scarring.
- Endometriosis: The presence of endometrial tissue outside the uterus, which can create adhesions or obstructions in the tubes.
Uterine Factors:
Issues within the uterus can prevent implantation or sustain a pregnancy. Common uterine infertility causes include:
- Congenital Malformations: Structural anomalies present from birth that affect the uterus shape or size.
- Asherman’s Syndrome: Scarring within the uterus often caused by surgical procedures.
- Post-Myomectomy Complications: Scarring or structural issues following surgery to remove fibroids.
- Endometrial Polyps: Growths in the uterine lining that may interfere with implantation.
- Other Causes: Conditions like tuberculosis, endometriosis, repeated pregnancy loss, fibroids, and menstrual irregularities (e.g., hypomenorrhea, amenorrhea).
Cervical Factors:
The cervix plays a crucial role in facilitating sperm entry and movement towards the egg. Cervical infertility causes include:
- Antisperm Antibodies: The presence of antibodies in the cervix that may attack or immobilize sperm.
- Non-Progressively Motile Sperm: Sperm that lack the ability to move effectively through cervical mucus.
- Infections: Infections in the vaginal and cervical areas can impair sperm function.
- Cervical Stenosis: Narrowing of the cervical canal, which can restrict sperm passage.
Other Contributing Factors:
- Peritoneal Causes: Peritoneal or pelvic adhesions, often resulting from endometriosis, can create a hostile environment for conception.
- Chronic Ill Health: Conditions like hypothalamic/pituitary diseases and adrenal cortical dysfunction can impact overall reproductive health and fertility.
Female infertility arises from a diverse set of factors impacting ovulation, tubal health, the uterus, cervix, and general well-being. Addressing these factors through medical evaluation and targeted treatment can improve the chances of conception and support women in their journey toward fertility.
Understanding Male
Infertility: Causes, Investigations, and Naturopathic Perspectives
Male infertility can arise from various health conditions and lifestyle factors that affect sperm production, quality, and functionality. This article provides an overview of the common causes, essential investigations, and naturopathic approaches to address male infertility holistically.
Common Causes of Male Infertility:
Several medical conditions and lifestyle factors can impair male fertility. The primary causes include:
- Cryptorchidism: Undescended testicles, which can affect sperm production and quality.
- Orchitis: Inflammation of the testicles, often due to infection, leading to potential fertility issues.
- Thyroid Gland Abnormalities: Thyroid imbalances that can affect hormone levels necessary for sperm production.
- Aspermia: Complete absence of semen, leading to challenges with conception.
- Oligospermia: Low sperm count, which reduces the likelihood of fertilization.
- Asthenospermia: Low sperm motility, affecting the ability of sperm to reach and fertilize the egg.
- Necrozoospermia: Presence of dead or immotile sperm, making conception difficult.
- Varicocele: Enlarged veins in the scrotum, which can increase temperature around the testes and affect sperm quality.
Essential Investigations for Diagnosing Male Infertility:
Diagnosis of male infertility typically involves a thorough medical history and physical examination to determine potential underlying causes.
- Medical History: Information on age, weight, and personal health history is essential, as well as any history of conditions such as tuberculosis, diabetes, thyroid disorders, or prior use of contraception.
- Physical Examination: This may include measuring blood pressure and evaluating signs such as hirsutism, thyroid function, breast growth (gynecomastia), fibroids, and other growths. Prolactin levels, infections, uterine size, and masses are also examined as part of a comprehensive fertility assessment.
- Sperm Analysis: This is a primary test for male infertility, measuring sperm count, motility, and quality to assess sperm health and functionality.
Naturopathic Perspective on Male Infertility: Addressing Root Causes:
In naturopathy, male infertility is often addressed by focusing on balancing the body’s energy systems, specifically targeting imbalances that may affect reproductive health.
- Pitta Aggravation: From a naturopathic perspective, an aggravated Pitta dosha (associated with heat and inflammation) is believed to contribute to fertility issues. Cooling therapies and dietary modifications are often recommended to help balance Pitta.
- Cold Formation: Cooling therapies, such as mud applications and cold water treatments, may help reduce internal heat and inflammation.
Naturopathic Therapies and Lifestyle Approaches:
Several naturopathic approaches can support fertility and overall reproductive health:
- Enema: Enemas may be used in naturopathy to cleanse the digestive system, which is believed to contribute to overall health and reproductive wellness.
- Mud Application: Applying mud packs to the abdomen is thought to aid in cooling the body and reducing inflammation, supporting reproductive health.
- Diet: A balanced, cooling diet rich in natural, unprocessed foods is recommended to balance Pitta and improve fertility.
- Pranayama & Yoga: Specific breathing techniques and yoga poses are thought to improve circulation, reduce stress, and enhance reproductive health. Recommended poses include:
- Uttana Prishthasana (Extended Puppy Pose)
- Mandukasana (Frog Pose)
- Janu Shirshasana (Head-to-Knee Pose)
Addressing male infertility involves a comprehensive approach that includes medical investigations, lifestyle modifications, and, in the case of naturopathy, balancing bodily energies. Through appropriate diagnostic steps and naturopathic practices, men can take steps to improve their fertility and overall reproductive health.
Herbs That Heal: Natural Remedies for Health and Wellness

Herbal medicine has long been valued for its therapeutic benefits and natural healing properties. This guide explores a variety of potent herbs known to support health and wellness. Each of these herbs has unique properties, traditionally used to enhance vitality, support specific health conditions, and promote overall well-being.
Key Healing Herbs and Their Benefits:
- Ashwagandha
Known as a powerful adaptogen, Ashwagandha helps the body manage stress, reduce inflammation, and support mental clarity. It’s widely used in Ayurvedic medicine to enhance energy levels, improve sleep quality, and support a healthy immune response. - Shatavari
Shatavari is renowned for its ability to balance hormones and support female reproductive health. Often used to aid in fertility and ease menopausal symptoms, this herb is also rich in antioxidants that promote overall vitality. - Kaucha
Also known as Mucuna Pruriens, Kaucha is a natural source of L-DOPA, which supports brain health by boosting dopamine levels. It’s known to enhance mood, reduce stress, and improve sexual health. - Shilajit
A mineral-rich resin found in the Himalayan mountains, Shilajit is highly prized for its rejuvenating properties. It boosts energy levels, improves stamina, and supports cognitive health, acting as a natural anti-aging remedy. - Vidarikand
This tuberous root is commonly used to support kidney health, enhance reproductive function, and nourish bodily tissues. It’s known for its cooling properties, which help balance Pitta and soothe inflammation. - Kamdudha Ras
A traditional Ayurvedic remedy, Kamdudha Ras is used to calm the mind, balance stomach acids, and support digestive health. It’s particularly beneficial for people experiencing acid reflux or gastritis. - Avipatikar
Avipatikar powder is a blend of herbs that aid in digestion, relieving acidity, and cleansing the gastrointestinal tract. It supports regular bowel movements and alleviates symptoms of indigestion. - Wheatgrass
Known for its high concentration of chlorophyll, Wheatgrass is a natural detoxifier that purifies the blood and supports liver health. It also provides a rich source of vitamins, minerals, and antioxidants. - Alfa-Alfa (Alfalfa)
Alfalfa is nutrient-dense, offering a natural source of vitamins A, C, E, and K. It is often used to boost energy levels, support digestive health, and aid in detoxification. - Ashokarishta
An herbal tonic used mainly in women’s health, Ashokarishta helps regulate menstrual cycles, reduces inflammation, and balances hormonal levels. It’s particularly beneficial for relieving symptoms of menstrual discomfort. - Kanchar Gugal
Traditionally used in Ayurvedic medicine to support thyroid health, Kanchar Gugal is beneficial for treating glandular imbalances and promoting metabolic health. It’s also valued for its anti-inflammatory properties. - Ashwagandharishta
This herbal preparation combines Ashwagandha with other medicinal herbs to support energy levels, enhance immunity, and alleviate stress. It’s often recommended for improving mental clarity, resilience, and endurance.
These natural herbs offer a range of healing benefits, from supporting mental clarity and hormonal balance to promoting detoxification and immune health. Incorporating these herbs into one’s wellness routine, under the guidance of a healthcare provider, can provide a holistic approach to health and vitality.








